Study Identifies New Opportunities for Targeted Immunotherapy
, by NCI Staff
A team of NCI researchers has reported that several types of gastrointestinal cancers have tumor-specific mutations that can be recognized by the immune system, potentially offering a new therapeutic opportunity for patients with these tumors.
In the study, published October 29 in Science, researchers showed that T lymphocytes (cell-killing white blood cells) targeting tumor-specific genetic mutations can be identified in metastatic gastrointestinal tumors, according to the study’s senior author, Steve Rosenberg, M.D., chief of the Surgery Branch in NCI’s Center for Cancer Research.
The finding is important, Dr. Rosenberg said, because the most common form of immunotherapy, checkpoint inhibition, hasn’t shown efficacy against most gastrointestinal cancers.
But this new study, he continued, “opens the door” to the development of a different type of immunotherapy, called adoptive cell transfer, for these and possibly many other cancers.
Single Patient Prompted Study
Some cancers, such as melanoma and smoking-induced lung cancer, have many genetic mutations, making them particularly immunogenic—that is, they tend to elicit very strong immune responses.
Checkpoint inhibitors, such as nivolumab (Opdivo®) and pembrolizumab (Keytruda®) have shown the most effectiveness against these types of cancer.
But, Dr. Rosenberg said, it’s been unclear whether common epithelial cancers, including gastrointestinal cancers, which tend to have far fewer mutations than melanoma and lung cancer, induce a tumor-specific immune response.
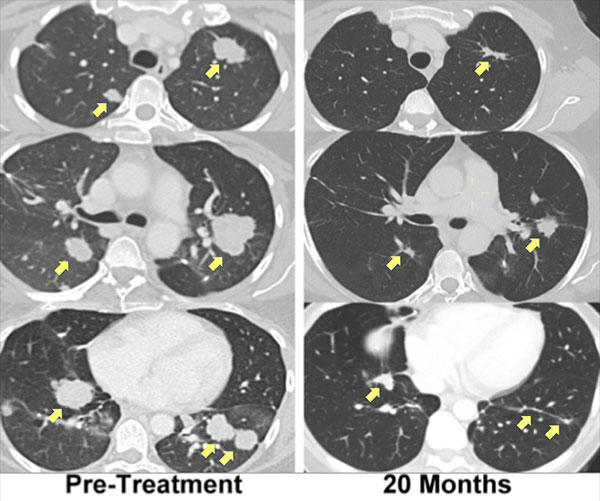
Last year his research team reported that T cells directed against a unique mutation in the tumor of a woman with advanced cholangiocarcinoma (bile duct cancer) were identified in lung metastases. The patient then underwent adoptive cell transfer, using an expanded pool of her own mutation-specific T cells, and experienced regression of her metastatic lung and liver tumors that is ongoing for more than 2 years.
The new study, which builds on that finding, included nine additional patients being treated at NCI as part of an ongoing clinical trial. The patients all had metastatic cancer, including colorectal, pancreatic, bile duct, and esophageal cancer. The analysis also included data from the patient with cholangiocarcinoma.
More Patients and More Possibilities
Overall, the patients’ tumors had a modest number of genetic mutations. Even so, the researchers were able to identify T cells that recognized at least one tumor-specific mutation in metastatic tumors in 9 of the 10 evaluated patients. The NCI team has since expanded this effort, identifying mutation-specific immune cells in 15 of 16 patients studied, Dr. Rosenberg said.
In several patients, the research team isolated immune cells that recognized a mutation in the KRAS gene that is commonly seen in patients with pancreatic and colorectal cancers and many other cancers. The KRAS mutation was the only mutation recognized by the immune system seen in more than one patient’s metastases.
Given the general frequency of the KRAS mutation in some cancers, the finding lays the groundwork for a possible “off-the-shelf” immunotherapy treatment—T cells engineered to express a receptor that recognizes tumors with this mutation, Dr. Rosenberg noted.
Two other patients from the original group of 10 were additionally treated with their own mutation-specific T cells but did not respond to treatment. In these patients, the researchers found, few if any infused T cells remained in the patients’ circulation for a prolonged period. In the patient with cholangiocarcinoma, however, at one month after treatment, nearly a quarter of her circulating T cells were the mutation-specific adoptively transferred cells.
A Blueprint for Many Cancers
There is still much research to be done, Dr. Rosenberg said, including how to improve the persistence of the transferred T cells. But he is optimistic about what this finding could represent.
“The whole idea of identifying mutations in a patient’s cancer and identifying and engineering T cells that specifically recognize those mutations is a blueprint for treating many different types of cancer,” he said.
The NCI team is already moving ahead with plans for an early phase clinical trial that follows on these findings, Dr. Rosenberg said.