Genetic Testing for Inherited Cancer Risk
What is genetic testing for inherited cancer risk?
Genetic testing looks for specific inherited changes (sometimes called mutations or pathogenic variants) in a person’s genes that may increase the risk of diseases such as cancer. About 5%–10% of all cancers are thought to be caused by harmful genetic changes that are inherited from a parent.
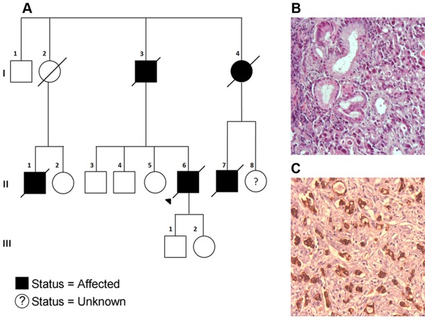
Cancer can sometimes appear to run in families even if there is not an inherited harmful genetic change in the family. For example, a shared environment or behavior, such as tobacco use, can cause similar cancers to develop among family members. However, certain patterns that are seen in members of a family—such as the types of cancer that develop, other non-cancer conditions that are seen, and the ages at which cancer typically develops—may suggest the presence of an inherited harmful genetic change that is increasing the risk for cancer.
Many genes in which harmful genetic changes increase the risk for cancer have been identified. Having an inherited harmful genetic change in one of these genes is sometimes referred to as having a hereditary cancer syndrome. Genetic testing of the blood or saliva can be used to identify whether someone has an inherited harmful genetic change in one of these genes.
Genetic testing for inherited cancer risk is different from genetic testing of tumors, which is sometimes used to guide treatment. Tumor genetic testing, which may also be referred to as tumor DNA sequencing, somatic testing, or biomarker testing, looks for genetic changes that occurred during someone’s lifetime. It can sometimes detect inherited changes as well, but it does not replace testing for inherited cancer risk. Genetic testing of tumor cells is addressed in the Biomarker Testing for Cancer Treatment page.
How is genetic testing done?
Genetic tests are usually requested by a genetic counselor, doctor, or other health care provider who has reviewed an individual’s personal and family medical history and identified a potential inherited cancer pattern.
Testing is done on a small sample of bodily fluid or tissue—usually blood but sometimes saliva, cells from inside the cheek, or skin cells. The sample is then sent to a genetic testing laboratory. Test results are usually returned in about 2 to 3 weeks.
Health insurance typically covers genetic counseling and genetic tests that are considered medically necessary. Uninsured individuals can access affordable genetic testing through organizations offering subsidized programs. NCI’s Cancer Information Service can help with locating such organizations. A person considering genetic testing should discuss costs and health insurance coverage with their health care provider and insurance company before being tested.
Who should consider genetic testing for inherited cancer risk?
Clinical practice guidelines recommend genetic testing for anyone diagnosed with triple-negative breast cancer, ovarian cancer, pancreatic cancer, colorectal cancer before age 50, metastatic prostate cancer, or male breast cancer. For people with these cancers, knowing whether their cancer is related to an inherited harmful genetic change may help to select the optimal treatment for them. This information may also be relevant to their blood relatives.
It is generally recommended that people with certain personal or family medical histories that suggest the possibility of a hereditary cancer syndrome consult with their doctor or a genetic counselor to see if genetic testing might be appropriate for them. Features that suggest the possibility of a hereditary genetic syndrome include:
- Family member with a known inherited harmful genetic change that increases cancer risk
- Cancer was diagnosed at a young age (for example, colon cancer diagnosed before age 50)
- Several different types of cancer occurred in the same person
- Cancer was diagnosed in multiple family members, particularly with patterns such as
- several first-degree relatives (the parents, siblings, or children of an individual) with the same type of cancer
- family members with breast or ovarian cancer
- family members with colon cancer and endometrial cancer
- Cancer in both organs in a set of paired organs, such as both kidneys or both breasts
- Rare types of cancer (for example, male breast cancer)
- The presence of birth defects that are known to be associated with inherited cancer syndromes, such as certain noncancerous illnesses or physical abnormalities
- Being a member of a racial or ethnic group that is known to have an increased risk of having a certain inherited cancer susceptibility syndrome and having one or more of the above features as well
It is generally recommended that, when possible, genetic counseling and testing for a hereditary cancer syndrome begin with a family member who has had cancer.
What genetic tests are available for inherited cancer risk?
There are several types of genetic tests that are used to look for harmful inherited gene changes that may be present in a family. The standard approach uses tests that look for harmful variants in multiple genes at the same time. These tests, called multigene (or panel) tests, are often used when there is not a known gene mutation in a family. Depending on the patient’s personal and family history as well as their preference for the amount of information they want, the health care provider may order a panel test that focuses on genes for a particular type of cancer, or they may order a broad panel test that looks at genes linked to a variety of common cancers.
When a gene variant is known to be present in the family, sometimes the entire gene is tested for changes. Alternatively, testing may focus on just the specific variant that is known to be present in the family.
What do the results of genetic testing mean?
Genetic testing can give several possible results: positive, negative, true negative, uninformative negative, or variant of uncertain significance (VUS).
Positive result. A positive test result means that the laboratory found a genetic change that is associated with an increased cancer risk. Such harmful genetic changes are called pathogenic or likely pathogenic variants. A positive result may:
- Confirm, for a person who has cancer, that the cancer was likely due to an inherited genetic change and potentially help guide treatment choices
- Indicate an increased risk of developing certain cancer(s) in the future and guide future management to lower that risk, including:
- Being checked at a younger age or more often for signs of cancer
- Taking medications or having surgery to reduce cancer risk
- Changing personal behaviors (like quitting smoking, getting more exercise, and eating a healthier diet) to reduce the risk of certain cancers
- Getting help to guide decisions about fertility and pregnancy
- Provide important information that can help other family members make decisions about their own health care, such as whether to have genetic testing to see if they have also inherited the harmful genetic change
Negative result. A negative test result means that the laboratory did not find any harmful genetic changes in the genes tested with currently available technology. This result is most useful when a specific disease-causing variant is known to be present in a family. In such a case, a negative result can show that the tested family member has not inherited the variant that is present in their family. Such a test result is called a true negative. A true negative result does not mean that there is no cancer risk, but rather that the risk is probably the same as that of someone in the general population.
When a person has a strong family history of cancer but the family has not been found to have any harmful genetic changes known to be associated with that cancer, a negative test result is classified as an uninformative negative. The family may still have an undetected variant leading to increased cancer risk. With more research and technology advances, it is possible additional genetic testing in the future may identify a harmful genetic change.
In the case of a negative test result, it is important that the person’s doctors and genetic counselors ensure that the person is receiving appropriate medical follow up based on their personal and family history and any other risk factors they may have. Even when the genetic testing is negative, some individuals may still benefit from more frequent checkups—particularly in the case of an uninformative negative.
Variant of uncertain significance. A variant of uncertain significance (VUS) is a genetic change for which there is not enough data available to know whether it increases the cancer risk or not. A VUS may be reclassified in the future as researchers learn more about these genetic changes. Most often, a VUS is reclassified as being benign (does not increase cancer risk), so this result is typically not considered in making health care decisions.
Sometimes a VUS may eventually be found to be associated with increased risks for cancer. Therefore, it is important for a person with a VUS result to keep in touch with the provider who performed the testing to ensure that they will be informed of any new information on the variant.
When should repeat genetic testing be considered?
A person’s genetic makeup does not change over time, so usually it is not necessary to repeat a specific genetic test. However, in certain situations further genetic testing may be appropriate:
- After an uninformative negative result, future testing may reveal a harmful variant that was not known at the time of the original test. New candidate genes are being discovered regularly, and ongoing improvements to testing technology may enable clinicians to identify previously undetectable variants in known genes.
- Occasionally, a repeat genetic test on a second tissue type (for example, a skin biopsy) may be needed to confirm an inconclusive result found in blood or saliva.
- When a new clinical feature or cancer occurs that suggests the possibility of an inherited variant in a gene that was not included in the original test, testing of additional genes may be appropriate.
What is the role of genetic counseling in genetic testing for inherited cancer risk?
Genetic counseling is generally recommended before any genetic testing for inherited cancer risk. It may also be performed after the test, especially if a positive result is found and a person needs to learn more about what this result means for them. This counseling should be performed by a trained genetic counselor or other health care professional who is experienced in cancer genetics.
Genetic counseling usually covers many aspects of the testing process, including:
- Assessment of the likelihood that there is an inherited cancer risk in the family
- Discussion of:
- The appropriateness of genetic testing and potential harms and benefits of testing
- The medical implications of positive, negative, and uncertain test results
- The psychological risks and benefits of learning genetic test results
- The risk of passing a variant to children
- The impact of testing for the family
- The genetic testing options that would be most appropriate based on personal and family history
- Explanation of the specific test(s) that might be used and the technical accuracy of the test(s) and their interpretation
Genetic counseling may also include discussing recommendations for risk-reduction strategies and enhanced screening approaches, referrals to support groups and other information resources, and emotional support for the person receiving the results.
Written informed consent is obtained before a genetic test is ordered. People give their consent by signing a form confirming that they have been told about, and understand, the purpose of the test, its medical implications, its risks and benefits, possible alternatives to the test, and their privacy rights.
What are the health implications of genetic test results for blood relatives?
Unlike most other medical tests, genetic tests can reveal information not only about the person being tested but also about that person’s blood relatives. Family members may have different opinions about whether they want to learn if they have an inherited change that increases their cancer risk.
A conversation with a genetic counselor may help family members of someone with a positive test learn about their genetic testing options and better understand the choices they may face should they learn they have a genetic change that puts them at increased risk of cancer.
What are the benefits and downsides of genetic testing for cancer risk?
There are benefits to genetic testing, regardless of the results.
- Testing can provide peace of mind if it finds that a person did not inherit a harmful genetic change identified in the family (an informative or true negative result).
- Testing that rules out the presence of harmful changes in all known cancer genes allows a person to manage their cancer risk based on their personal and family history.
- Testing that identifies a harmful genetic change (a positive test result) provides the person an opportunity to understand and, in some cases, potentially manage their cancer risk.
- For people who are already diagnosed with a cancer, results of genetic testing may help suggest the most appropriate treatments and provide information about their risk of other cancers.
- Genetic testing provides an opportunity for family members to learn about their own cancer risk.
The potential downsides of genetic testing include:
- Psychological stress from learning that one has a genetic change that increases not only their own cancer risk, but also that of their blood relatives, including children (sometimes called “parental guilt”)
- Feelings of “survivor guilt” on learning that one doesn’t have a harmful change that is present in other members of the family
- Uncertainty and stress from receiving an uninformative test result, such as a report of a variant of uncertain significance (VUS)
- Cost of genetic testing, if not covered by insurance
- Need for potentially costly and time-consuming medical follow-up and prevention measures if testing is positive
- Privacy and discrimination issues
- The possibility of a rare false-positive result (leading to unnecessary follow-up and psychological stress) or a false-negative result (leading to a mistaken sense of decreased cancer risk)
- The possibility of an individual acting on incorrect, incomplete, or misleading information, if their test results are not appropriately explained to them
Who has access to a person's genetic test results?
Medical test results are normally included in a person’s medical records, particularly if a doctor or other health care provider has ordered the test or has been consulted about the test results. Therefore, people considering genetic testing must understand that their results may become known to others with legitimate, legal access to their medical records.
Generally, a person’s genetic results and information in their medical record is covered by the Privacy Rule of the Health Information Portability and Accountability Act (HIPAA) of 1996. The HIPAA Privacy Rule requires that health care providers and others with medical record access protect a person’s identifiable health information by setting limits on the uses and disclosure of this information. It also empowers people to control certain uses and sharing of their health-related information; usually this means that a person must first grant permission if a person or organization not involved in their medical care wants to access to their medical records. Many states also have laws to protect patient privacy and limit the release of genetic and other health information.
Additionally, even if genetic test results are accessed or known, legal protections are in place to prevent genetic discrimination; this could occur if health insurance companies or employers were to treat people differently because they have a gene change that increases their risk of a disease such as cancer, or because they have a strong family history of a disease such as cancer.
The Genetic Information Nondiscrimination Act (GINA), which became law in 2008, prohibits discrimination based on genetic information in determining health insurance eligibility or rates and suitability for employment. However, GINA does not cover members of the military and it does not apply to life insurance, disability insurance, or long-term care insurance. Some states have additional genetic nondiscrimination legislation that addresses the possibility of discrimination in those contexts.
The National Human Genome Research Institute’s Genetic Discrimination page includes links to more information about GINA, HIPAA, and other legislation related to genetic discrimination in insurance or employment.
Can at-home or direct-to-consumer (DTC) genetic tests be used to test for cancer risk?
An increasing number of companies offer at-home genetic testing, in contrast to genetic testing that a health care provider orders in a clinical setting. People collect a saliva sample or a mouth swab themselves and submit the sample through the mail. Companies report test results in different ways, but most deliver results on a secure website or send a report by mail.
There are two broad categories of at-home testing: direct-to-consumer testing, and consumer-directed genetic testing (sometimes referred to as patient-initiated, direct access, or provider-mediated genetic testing).
Direct-to-consumer (DTC) genetic tests. These are genetic tests that customers can order themselves without a doctor’s order. People often use DTC tests to explore ancestry, to learn about personal traits such as an aversion to cilantro, and to get health information (such as predicting disease risk). However, these tests do not give complete genetic health information, and in most cases the information that they do give is not intended for use in making health decisions (that is, it is not clinically actionable).
DTC genetic tests that are specifically for variants that confer a high cancer risk and are clinically actionable must be approved by the Food and Drug Administration (FDA) before they can be marketed. As of January 2024, the only FDA-approved DTC genetic test for inherited cancer risk tests for three different BRCA gene variants that are common in people of Ashkenazi Jewish descent. However, there are hundreds of BRCA gene variants that could increase cancer risk in a person and family, so a negative BRCA result on a DTC test is not informative in most people. About 80% of cancer-causing BRCA variants are missed by this approach.
Many DTC tests advertise that they can give a variety of interesting health results or that they will provide an individual’s raw genetic data that can be used to assess many different kinds of genomic variants. However, concerns have been raised about the claims made and practices used by some of these companies, and online tools that can be used to analyze and interpret raw data are prone to inaccuracies.
Consumer-directed genetic testing. These tests are initiated by a consumer but ultimately ordered by a doctor—either someone’s own doctor, or a doctor that the testing company identifies. Doctors identified by a testing company may have an incentive to order the company’s brand of testing, whether or not it is the best test for the patient. These doctors do not meet with patients and may not have all the information necessary to provide guidance in the best testing options for a patient.
Although the tests used in consumer-directed testing are similar to those ordered by one’s own provider in a clinical setting, people considering consumer-directed testing should be aware that the tests ordered may look at more genes than is clinically necessary, increasing the potential for unexpected and anxiety-provoking positive results and findings of variants of uncertain significance. Most companies that provide consumer-directed genetic testing do offer genetic counseling; however, if someone does not opt for counseling, they may not have an opportunity to go over their results with a health care professional. Without guidance about what genetic testing is most appropriate for them given their personal and family history or about the implications of their results, people taking at-home genetic tests may experience unneeded anxiety or false reassurance or may make important decisions about medical treatment or care based on incomplete information.
DTC and consumer-initiated genetic testing both come with an increased risk of misinterpreting information. For example, a person may have a negative genetic testing result and not understand that they are still at increased risk of disease and qualify for increased surveillance based on their family history. Some insurance companies may only pay for a certain amount or type of genetic testing, so if individuals use insurance to pay for DTC testing they may find out that follow-up testing ordered by their doctor is not covered.
The privacy of at-home genetic test results is dependent on individual company policies. Companies’ disclosure policies are not always provided, or they may be difficult to find and understand. In addition, companies that provide at-home testing may not be subject to the federal and state privacy laws and regulations that protect genetic and other health information (e.g., the HIPAA Privacy Rule). People considering at-home consumer-based genetic testing should make sure that they understand a company’s privacy policy and terms of use before sending a sample.
The FDA has a page about DTC tests with information about how these tests are regulated. In 2024, the FDA indicated that it will start regulating lab-developed tests, which include many of the tests used in consumer-directed genetic testing.
MedlinePlus, a consumer health website from the National Library of Medicine at the National Institutes of Health, has information about DTC genetic testing.
How are genetic testing labs regulated?
US laboratories that perform health-related testing, including genetic testing, are regulated under the Clinical Laboratory Improvement Amendments (CLIA) program. Laboratories that are certified under CLIA are required to meet federal standards for quality, accuracy, and reliability of tests. All laboratories that do genetic testing and share results must be CLIA certified. However, CLIA certification only indicates that appropriate laboratory quality control standards are being followed; it does not guarantee that a genetic test being done by a laboratory is medically useful or properly interpreted. Additionally, direct-to-consumer genetic testing labs are not required to comply with CLIA, but they may choose to do so. The National Human Genome Research Institute has more information available on its Regulation of Genetics Tests page.
What research is being done to improve genetic testing for inherited cancer risk?
Research is ongoing to find better ways to detect, treat, and prevent cancer in people who carry genetic variants that increase the risk of certain cancers. Scientists are also doing studies to identify novel genetic changes that can increase a person’s risk of cancer. There is also much work being done to increase the accuracy and consistency of classifying the genetic variants detected by testing.
The goal of another avenue of research is to provide doctors and patients with better information about the actual cancer risks associated with specific genetic variants, particularly variants of uncertain significance.
Although clinical practice guidelines recommend that all people diagnosed with certain cancers undergo testing for an inherited genetic change, only a small percentage do get tested. Likely contributors to the low testing rates include both limited access to genetic counselors and uncertainty or mistrust of genetic testing. The development and testing of new care delivery models to improve the rates of cancer susceptibility genetic testing is a major goal of the Cancer Moonshot.