Intraperitoneal Chemotherapy in Advanced Ovarian Cancer Improves Survival, But Is Underused
, by NCI Staff
Combining intraperitoneal (IP) chemotherapy with intravenous (IV) chemotherapy improves survival in women with advanced ovarian cancer, though its use in clinical practice has been limited, according to findings from a new study.
Published August 3 in the Journal of Clinical Oncology, the prospective cohort study found that, compared with IV chemotherapy alone, treatment with both IP and IV chemotherapy was associated with improved 3-year overall survival in women with stage III ovarian cancer who, after surgery, had only very small tumor deposits remaining (1 cm or less in size). IP chemotherapy was used in less than half of women in the study.
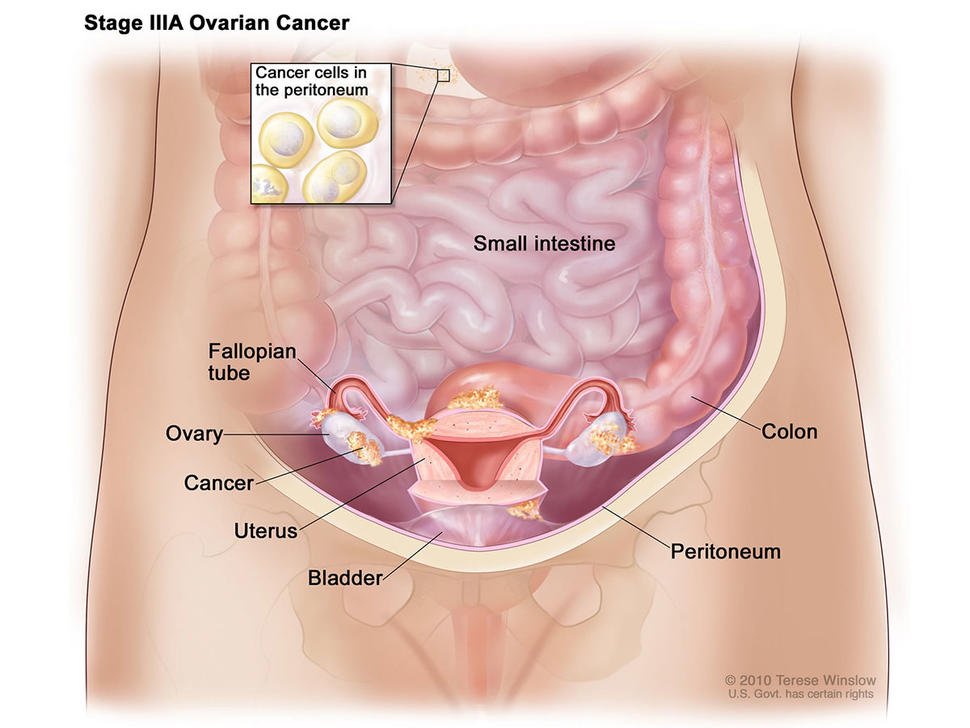
IP chemotherapy is delivered through an implanted subcutaneous port that drains into the cavity of the abdomen, allowing direct access for the drug to the peritoneal cavity, where ovarian cancer has spread. Its use, however, can cause more frequent and more severe side effects than IV chemotherapy, including abdominal pain, nausea, and vomiting.
In 2006, results from a large clinical trial showed that treatment with IP and IV chemotherapy extended median overall survival for patients with ovarian cancer by more than a year, compared with women treated with IV chemotherapy alone.
Following release of the trial results, NCI issued a clinical announcement detailing findings from the trial and other trials of IP chemotherapy in patients with ovarian cancer, noting that the treatment approach was associated with a “significant survival benefit… compared to IV chemotherapy alone.”
However, it wasn’t known whether IP chemotherapy (in combination with IV chemotherapy) is routinely used in clinical practice. To investigate, Alexi Wright, M.D., of the Dana-Farber Cancer Institute, and her colleagues prospectively collected treatment plans and outcomes from 2005-2012, and retrospectively from 2003-2005, for 823 patients who were diagnosed with advanced ovarian cancer at six National Comprehensive Cancer Network (NCCN) centers. All of the patients were treated outside of a clinical trial.
They found that use of IP treatments increased from 0 to 33 percent between 2003 and 2006, and up to 50 percent by 2008, leveling off from that point forward. Use of IP chemotherapy in eligible patients, however, varied substantially by NCCN center, from 4 percent to 67 percent. When IP chemotherapy was used, the treatment was modified in more than 40 percent of patients from the approach used in the definitive phase III clinical trial.
The 3-year overall survival was 81 percent in women treated with IP/IV chemotherapy (402 women), compared with 71 percent in those treated with IV chemotherapy alone. Nearly 60 percent of women who received IP chemotherapy completed all planned cycles of therapy, and there were no differences in infections or nausea and vomiting between the two groups.
“In our study we looked at ovarian cancer patients who were treated in clinical practice and found the same results as the clinical trial, but with less toxicity to patients,” Dr. Wright said. “This suggests that IP chemotherapy really is feasible to use in clinical practice and should be more widely used. It is low hanging fruit to improve outcomes for patients with ovarian cancer.”
The study did not examine why IP chemotherapy is underused outside of clinical trials, explained Elise Kohn, M.D., head of Gynecologic Cancer Therapeutics in NCI’s Division of Cancer Treatment and Diagnosis.
“However, we know many patients in clinical trials stop IP chemotherapy early because it is too toxic,” Dr. Kohn said. “IP therapy may be cut short, for example, if the port delivery system malfunctions, if there is an infection at the site of implant, or if patients are unable to tolerate pain or other side effects associated with drug administration.”
The centers in the study used many different drugs, schedules, and doses, Dr. Wright explained, so the researchers were unable to directly compare the effectiveness of each of the different treatment combinations and modifications.
The types of modifications made, including lowering chemotherapy doses and switching the drugs being used, “suggests that clinicians were doing so to avoid harming their patients,” Dr. Wright continued.
Nevertheless, the improved survival with IP chemotherapy “suggests this may be due to the route of delivery, not differences in drugs,” Dr. Wright concluded.
Dr. Kohn noted that NCI is supporting trials to better understand how best to use IP chemotherapy, including a multi-center phase III trial testing IP/IV chemotherapy in combination with bevacizumab in patients with stage II-III ovarian cancer.