HPV Vaccine Effective Against Infection at Multiple Sites, Provides Partial Protection in Women with Previous Infections
, by NCI Staff
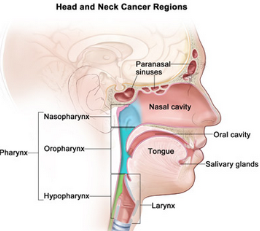
Vaccination against high-risk types of human papillomavirus (HPV) protected young women from infection with these HPV types at the cervix, anus, and mouth—the three primary anatomic sites where persistent HPV infections can cause cancer. The multi-site protection also was observed, though at lower levels, in women previously exposed to the virus. NCI researchers reported this finding last week at the 2015 annual meeting of the American Association for Cancer Research (AACR) in Philadelphia.
The findings are among the latest to emerge from the HPV Vaccine Trial in Costa Rica, which was launched a decade ago by NCI, in collaboration with researchers in Costa Rica, to test the efficacy of the bivalent HPV vaccine Cervarix in preventing cervical HPV and pre-cancer in women vaccinated between the ages of 18 to 25.
Previous reports from the trial have demonstrated that the vaccine is highly effective in preventing HPV infections in the cervix, anus, or mouth—especially among women not infected prior to vaccination—when these sites were looked at separately.
“This is the first study to analyze multi-site protection,” explained the lead author on the study, Daniel C. Beachler, Ph.D., a postdoctoral fellow in NCI’s Division of Cancer Epidemiology and Genetics.
The findings presented at the AACR meeting—which involved analysis of samples from all three anatomic sites obtained from nearly 4,200 women—showed that 4 years after the initial vaccination, there was a 65 percent reduction in HPV at any of the three sites.
Women without evidence of prior HPV 16 or 18 exposure—defined as the absence of HPV 16 or 18 antibodies in blood, and no DNA evidence of cervical HPV 16 or 18 infection at time of first vaccination—experienced the greatest protection, with an efficacy of approximately 84 percent at any site, Dr. Beachler reported.
The vaccine efficacy was lower but still present among women who had evidence of prior exposure to HPV 16 or 18. Overall, the efficacy increased to 91 percent against HPV infection at two or three anatomical sites.
The HPV vaccine, Dr. Beachler stressed, cannot help clear current infections. “But it may provide some protection at one or more sites in women exposed to HPV prior to vaccination.”
The results, he added, support current recommendations for routine HPV vaccination starting at age 11 or 12, and vaccination through age 26 for those not vaccinated previously.
In addition to Cervarix, two other HPV vaccines are available in the United States: the quadrivalent vaccine Gardasil and the recently approved Gardasil9, which protects against seven cancer-causing types of HPV.
FURTHER READING
Gardasil 9 Vaccine Protects against Additional HPV Types