What is computed tomography?
Computed tomography (CT) is a noninvasive imaging procedure that uses special x-ray equipment to create detailed pictures, or scans, of areas inside the body.
Each picture created during a CT procedure shows the organs, bones, and other tissues in a thin “slice” of the body. The entire series of pictures produced in CT is like a loaf of sliced bread—you can look at each slice individually (2-dimensional pictures), or you can look at the whole loaf (a 3-dimensional picture). Computer programs are used to create both types of pictures.
Modern CT machines take continuous pictures in a helical (or spiral) fashion rather than taking a series of pictures of individual slices of the body, as the original CT machines did. Helical CT (also called spiral CT) has several advantages over older CT techniques: it is faster and produces better quality 3-D pictures of areas inside the body, which may improve detection of small abnormalities.
CT has many uses in the diagnosis, treatment, and monitoring of cancer, including
- screening for cancer
- helping diagnose the presence of a tumor
- providing information about the stage of a cancer
- determining exactly where to perform (i.e., guide) a biopsy procedure
- guiding certain local treatments, such as cryotherapy, radiofrequency ablation, and the implantation of radioactive seeds for brachytherapy
- helping plan external-beam radiation therapy or surgery
- determining whether a cancer is responding to treatment
- detecting recurrence of a tumor
In addition, CT is widely used to help diagnose circulatory (blood) system diseases and conditions, such as coronary artery disease (atherosclerosis), blood vessel aneurysms, and blood clots; spinal conditions; kidney and bladder stones; abscesses; inflammatory diseases, such as ulcerative colitis and sinusitis; and injuries to the head, skeletal system, and internal organs. CT imaging is also used to detect trauma, brain bleeds, and abnormal brain function or deposits in adult patients with cognitive impairment who are being evaluated for Alzheimer’s disease and other causes of cognitive decline.
What can a person expect during a CT procedure?
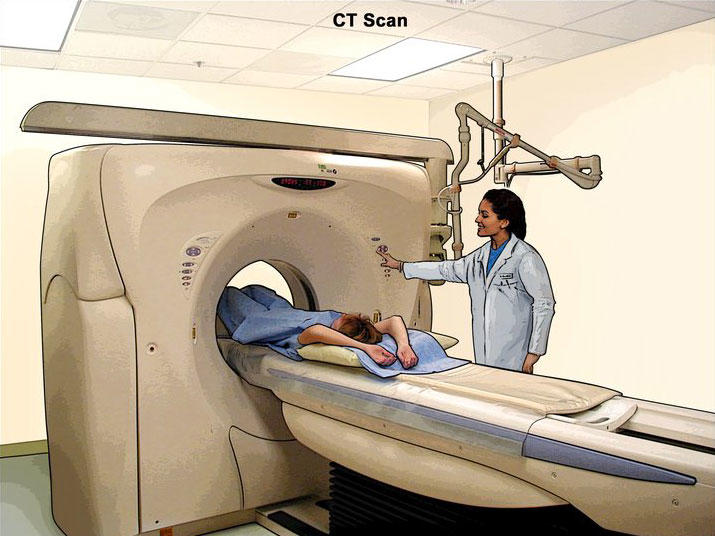
During a CT procedure, the person lies very still on a table, and the table passes slowly through the center of a large donut-shaped x-ray machine. The person might hear whirring sounds during the procedure. At times during a CT procedure, the person may be asked to hold their breath to prevent blurring of the images.
Sometimes, people having CT are given a contrast (imaging) agent, or dye, before the procedure. The contrast dye highlights specific areas inside the body, resulting in clearer pictures. The dye may be given by mouth, injected into a vein, or given by enema. Iodine and barium are two dyes commonly used in CT.
In very rare cases, the contrast agents used in CT can cause allergic reactions. Some people experience mild itching or hives (small bumps on the skin). Symptoms of a more serious allergic reaction include shortness of breath and swelling of the throat or other parts of the body. People should tell the technologist immediately if they experience any of these symptoms so they can be treated promptly. Very rarely, the contrast agents used in CT can cause kidney problems for certain patients, such as those with impaired kidney function. Kidney function can be checked with a simple blood test before the contrast agent is injected.
CT is a noninvasive procedure and does not cause any pain. However, lying in one position during the procedure may be slightly uncomfortable. The length of a CT procedure depends on the size of the area being scanned, but it usually lasts only a few minutes to half an hour. For most people, CT is performed on an outpatient basis at a hospital or a radiology center, without an overnight hospital stay.
Some people are concerned about experiencing claustrophobia during a CT procedure. However, most CT scanners surround only portions of the body, not the whole body. Therefore, people are not enclosed in a machine and are unlikely to feel claustrophobic.
People should let their health care provider and the technologist know if there is any possibility that they are pregnant. Depending on the part of the body to be scanned, the provider may reduce the radiation dose or use an alternative imaging method. However, the level of radiation exposure in a CT scan is believed to be too low to harm a growing fetus.
How is CT used in cancer screening?
CT is used in both colorectal cancer screening (including screening for large polyps) and lung cancer screening.
Colorectal cancer
A procedure called CT colonography (also known as virtual colonoscopy) can be used to screen for both large colorectal polyps and colorectal tumors. Virtual colonoscopy is the use of CT to produce a series of pictures of the colon and the rectum from outside the body instead of using a colonoscope to view the inside of the colon and rectum. The effective dose to the patient from a CT colonography procedure is similar to that of a standard CT scan of the abdomen and pelvis, which is about 6 millisieverts (mSv) (1). (By comparison, the estimated average annual dose received from natural sources of radiation is about 3 mSv.)
Although CT colonography is effective for visualizing tumors and adenomas, it has potential downsides. One is that if polyps or other abnormal growths are found during a virtual colonoscopy, a standard colonoscopy is needed to remove them. Also, CT colonography can lead to the unintentional discovery of medical findings in areas outside the colon and rectum that require additional follow-up procedures to rule out the unlikely possibility that these findings indicate real problems.
Lung cancer
Low-dose CT of the lungs is used to screen for lung cancer in adults who are increased risk because of their smoking history. The risk of lung cancer in those who have never smoked tobacco products is generally so low that they would be unlikely to benefit from lung cancer screening.
The U. S. Preventive Services Task Force (USPSTF) recommends annual lung cancer screening with low-dose CT for people ages 50 to 80 years who have a 20 pack-year or more smoking history (which they could have if, for example, they smoked one pack of cigarettes per day for 20 years or two packs of cigarettes per day for 10 years) and either currently smoke or quit smoking within the last 15 years (2). The estimated effective dose of radiation in a low-dose lung CT scan is 1.5 mSv (1).
The National Lung Screening Trial (NLST) demonstrated that three annual low-dose CT screens for lung cancer reduced lung-cancer mortality by 20% (3). However, there are potential harms as well as benefits. For example, people screened with low-dose lung CT can have false-positive results (that is, findings that appear to be abnormal even though no cancer is present), which need monitoring and may necessitate invasive procedures to rule out cancer. Overdiagnosis—finding and treating a cancer that would not have caused problems during someone’s lifetime—is also a possibility, although there is little, if any, evidence of overdiagnosis after extended follow-up of the NLST (4). Also, because low-dose lung CT can produce images of organs and tissues outside the lung, it is possible that abnormalities outside of the lungs, such as renal or thyroid masses, may be found. As with extracolonic findings from CT colonography, some such findings will be serious, but many will not. NCI’s Patient and Physician Guide: National Lung Screening Trial provides more information on the benefits and harms of CT screening for lung cancer.
What is total-body, or whole-body, CT?
Total-body, or whole-body, CT creates pictures of nearly every area of the body—from the chin to below the hips. This procedure, which is used routinely in patients who already have cancer, can also be used in people who do not have any symptoms of disease.
However, whole-body CT has not been shown to be an effective screening method for healthy people. Most abnormal findings from this procedure do not indicate a serious health problem, but the tests that must be done to follow up and rule out a problem can be expensive, inconvenient, and uncomfortable. Also, they may expose the patient to extra risks, such as from an invasive procedure like a biopsy that may be needed to evaluate the findings.
In addition, whole-body CT can expose people to relatively large amounts of ionizing radiation—an effective dose of about 10 to 20 mSv, or more than three times the estimated average annual dose received from natural sources of radiation.
Most doctors recommend against whole-body CT for people without any signs or symptoms of disease.
What is combined PET/CT?
Combined PET/CT uses two imaging methods, CT and positron emission tomography (PET), in one procedure. CT is done first to create anatomic pictures of the organs and structures in the body, and then PET is done to create pictures that provide functional data about the metabolic pathways (chemical reactions that take place in a cell to create and use energy) that are active in tissues or cells. Cancer cells often use different metabolic pathways than normal cells.
Patients undergoing a PET/CT procedure are administered a positron-emitting (radioactive) substance, or radiopharmaceutical, that is designed to target cancer cells specifically. Numerous radiopharmaceuticals have been developed. However, the most common PET procedure uses an imaging agent called FDG (a radioactive form of the sugar glucose). Because cancerous tumors usually metabolize glucose more rapidly than normal tissues, they take up more FDG and appear different from other tissues on a PET scan.
Other PET imaging agents can provide information about the level of oxygen in a particular tissue, the formation of new blood vessels, the presence of bone growth, whether tumor cells are actively dividing and growing, and whether cancer may have spread. For example, two prostate-specific membrane antigen (PSMA)–targeted imaging drugs with attached radioactive tracers—piflufolastat F-18 (Pylarify) and Ga-68 gozetotide (Locametz)—are used for PET/CT imaging of PSMA-positive lesions in men with suspected prostate cancer metastases. The estimated effective dose from a PSMA PET procedure is 3 mSv (5).
Combining CT and PET may provide a more complete picture of a tumor’s location and growth or spread than either test alone. The combined procedure may improve the ability to diagnose cancer, to determine how far a tumor has spread, to plan treatment, and to monitor response to treatment. Combined PET/CT may also reduce the number of additional imaging tests and other procedures a patient may need. The effective dose from a whole-body combined PSMA PET/CT procedure can range from 4 to 23 mSv depending on the specifics of the imaging protocol (1, 6).
Is the radiation from CT harmful?
Some people may be concerned about the amount of radiation they receive during CT. CT imaging involves the use of x-rays, which are a form of ionizing radiation. Exposure to ionizing radiation is known to increase the risk of cancer. Standard x-ray procedures, such as routine chest x-rays and mammography, use relatively low levels of ionizing radiation. The radiation exposure from CT is higher than that from standard x-ray procedures, but the increase in cancer risk from one CT scan is still small. The benefits of a CT scan, especially if it is being used to diagnose cancer or another serious condition in someone who has signs or symptoms of disease, greatly outweigh any potential health risks.
It is also important to note that everyone is exposed to some background level of naturally occurring ionizing radiation every day. The average person in the United States receives an estimated effective dose of about 3 millisieverts (mSv) per year from naturally occurring radioactive materials, such as radon and radiation from outer space (1). By comparison, the radiation exposure from one low-dose CT scan of the chest (1.5 mSv) is comparable to 6 months of natural background radiation, and a typical CT scan of the chest (6.1 mSv) is comparable to 2 years of natural background radiation (1).
The widespread use of CT and other procedures that use ionizing radiation to create images of the body has raised concerns that even small increases in cancer risk could lead to large numbers of future cancers (7, 8). Women are at a somewhat higher risk than men of developing cancer after receiving the same radiation exposures at the same ages (9).
People considering CT should talk with their doctors about whether the procedure is necessary for them and about its risks and benefits. Some organizations recommend that people keep a record of the imaging examinations they have received in case their doctors don’t have access to all of their health records. A sample form, called My Medical Imaging History, was developed by the Radiological Society of North America, the American College of Radiology, and the U.S. Food and Drug Administration. It includes questions to ask the doctor before undergoing any x-ray exam or treatment procedure.
What are the risks of CT scans for children?
Radiation exposure from CT scans affects adults and children differently. Children are more sensitive to radiation than adults because of their growing bodies and the rapid pace at which the cells in their bodies divide. In addition, because children have potentially many more years of life ahead of them than adults, there is a greater opportunity for them to develop radiation-related cancers (10).
In a large multinational study, individuals who had at least one CT scan before the age of 22 were found to have an increased risk of developing hematological cancers, particularly lymphoid and myeloid cancers and acute leukemia (11). In the 12 years after a single CT scan, the risk of cancer was about 1–2 cases for every 10,000 scans performed on children and young people.
In talking with health care providers, three key questions that parents can ask are:
- Why is the test needed?
- Will the results change the treatment decisions?
- Is there an alternative test that doesn’t involve radiation?
If the test is clinically justified, then the parents can be reassured that the benefits will outweigh the small long-term risks.
What is being done to reduce the level of radiation exposure from CT?
In response to concerns about the increased risk of cancer associated with CT and other imaging procedures that use ionizing radiation, several organizations and government agencies have developed guidelines and recommendations regarding the appropriate use of these procedures.
- The Image Gently campaign seeks to raise awareness about methods to reduce radiation doses during pediatric medical imaging examinations.
- The Image Wisely campaign aims to lower the amount of radiation used in medically necessary imaging studies and eliminating unnecessary procedures.
- The U.S. Food and Drug Administration (FDA)’s Initiative to Reduce Unnecessary Radiation Exposure from Medical Imaging focuses on the safe use of medical imaging devices, informed decision-making about when to use specific imaging procedures, and increasing patients’ awareness of their radiation exposure.
- The NIH Clinical Center requires that radiation dose exposures from CT and other imaging procedures be included in the electronic medical records of patients treated at the center (12). In addition, all imaging equipment purchased by NIH must provide data on exposure in a form that can be tracked and reported electronically. This patient protection policy is being adopted by other hospitals and imaging facilities.
- NCI’s guide for health care providers, Radiation Risks and Pediatric Computed Tomography (CT): A Guide for Health Care Providers, addresses the value of CT as a diagnostic tool in children, unique considerations for radiation exposure in children, risks to children from radiation exposure, and measures to minimize exposure.
- The American College of Radiology (ACR) has developed the ACR Appropriateness Criteria®, evidence-based guidelines to help providers make appropriate imaging and treatment decisions for a number of clinical conditions.
- ACR has also established the Dose Index Registry, which collects anonymized information related to dose indices for all CT exams at participating facilities.
- CT scanner manufacturers are developing newer detector systems and image reconstruction algorithms that can provide higher quality images at much lower radiation doses.
What is NCI doing to improve CT imaging?
Researchers funded by NCI are studying ways to improve the use of CT in cancer screening, diagnosis, and treatment. NCI also conducts and sponsors clinical trials that are testing ways to improve CT or new uses of CT imaging technology. Some of these clinical trials are run by the ECOG-ACRIN Cancer Research Group, one of the groups in NCI’s National Clinical Trials Network.
NCI’s Cancer Imaging Program (CIP), part of the Division of Cancer Treatment and Diagnosis (DCTD), funds cancer-related basic, translational, and clinical research in imaging sciences and technology. CIP supports the development of novel imaging agents for CT and other types of imaging procedures to help doctors better locate cancer cells in the body. In addition, CIP maintains the Cancer Imaging Archive, which is a library of medical images of cancer, including low-dose CT images, that are accessible for public download. This library has been used extensively by outside researchers in developing computer-aided diagnosis to help radiologists interpret CT images, for example, in lung cancer screening.
Where can people get more information about CT?
Additional information about CT imaging is available from the U.S. Food and Drug Administration (FDA), the federal agency that regulates food, drugs, medical devices, cosmetics, biologics, and radiation-emitting products.
Information about diagnostic radiology, including CT imaging, is also available at RadiologyInfo.org, the public information website of the Radiological Society of North America and the American College of Radiology.