Informal Caregivers in Cancer: Roles, Burden, and Support (PDQ®)–Health Professional Version
Overview
Informal caregiving is broadly defined as services provided by an unpaid person, such as helping with personal needs and household chores, managing a person's finances, arranging for outside services, or visiting regularly.[1,2] An informal caregiver is usually a relative or friend and may or may not live in the same household as the person with cancer.
Informal caregiving provides significant practical and economic benefits. This summary describes the experiences of informal caregivers of people with cancer, explains the risk factors for caregiver burden (which is often associated with negative psychological consequences), and evaluates evidence-based interventions designed to reduce the burden of informal caregiving. The goal of the summary is to provide the oncology clinician with both a deeper appreciation of the importance of informal caregivers, and the information necessary to recognize burdened caregivers and effectively intervene.
Who Are Informal Caregivers and What Roles Do They Play?
In 2016, the National Alliance for Caregiving reported an analysis of the survey responses of 111 caregivers who self-identified as providing care to a person with cancer.[3] The respondents were part of a much larger study that identified a representative sample of adult caregivers who provided unpaid care to an adult relative or friend in the 12 months preceding the time of the survey.
The following findings provide a snapshot of informal caregivers of people with cancer and the challenges they face:
- 58% were women.
- 88% cared for a relative.
- 39% lived with the person being cared for.
- 50% reported high emotional stress related to caregiving.
- 25% reported high financial strain.
- 50% were employed while caregiving, working an average of 35 hours per week.
- 73% were involved in discussions about care during hospitalization; however, only about half of them (54%) were asked what help was needed after discharge.
- 72% assisted with medical tasks.
- 43% reported needing help to manage emotional and physical stress.
- 40% wanted help making end-of-life decisions.
- 33% wanted help keeping their friend or relative safe at home.
- Caregiving for patients with cancer was noted to be episodic and lasted for approximately 2 years on average.
Caregiving is also relational.[4,5] In addition, there are important implications for the interconnectedness between patient and caregiver that the oncology clinician should be aware of, including the following:
- Patients and caregivers influence each other’s mental and physical health (partner effects) in addition to their own outcomes (actor effects).[6]
- The psychological well-being of caregivers seems to influence patients’ evaluations of the quality of their care. One survey of 689 patients and their caregivers demonstrated that higher levels of depression in caregivers were associated with patients’ ratings of lower quality of care.[7]
- There are important distinctions between the experiences of patients and informal caregivers. A semistructured interview study of 23 patients with advanced colorectal cancer and 23 caregivers demonstrated the prevalence and nature of these differences.[8] Participants agreed on four challenges:
- Emotionally processing the initial diagnosis or recurrence.
- Managing the practical and emotional aspects of patient care.
- Facing an uncertain future.
- Encountering symptom-related suffering.
In no instance, however, did patient and caregiver identify the same key challenge. Clinicians are advised to assess caregiver needs independent of patient needs.
- The caregiver may not be an accurate informant of the patient’s experience. One study demonstrated that caregivers correctly reported 67% of patients’ physical difficulties, 69% of patients’ psychological difficulties, and 40% of patients’ social difficulties.[9] There were no predictive demographic factors. In further support of the need for caution, an analysis of office visits recorded on audiotape revealed that caregivers often spoke on behalf of patients without validation by the patients.[10] In addition to this pseudo-surrogacy, caregivers often conflated their concerns with those of the patients.
The Psychological Consequences of Caregiving
The psychological consequences of caregiving vary widely. Some caregivers report positive outcomes such as post-traumatic growth and benefit finding. But a minority of caregivers experience anxiety, depression, or post-traumatic stress disorder (PTSD).
Benefit finding: Results of several qualitative studies (interviews or narrative questionnaires) of caregivers of either adult cancer survivors [11,12] or childhood cancer survivors [13,14] revealed common themes on the positive aspects of caregiving:
- Closer relationships with others, including partners and children.
- Greater appreciation of life.
- Clarification of life priorities.
- Increased faith.
- More empathy for others.
- Better health habits.
These common themes are more quantitatively measured by using the Benefit Finding Scale. Six domains of caregivers’ personal growth have been identified [15] and are consistent for both caregivers of survivors and those in bereavement:[16]
- Acceptance.
- Empathy.
- Appreciation.
- Family.
- Positive self-view.
- Reprioritization.
Anxiety and depression: Several large survey studies provide more accurate estimates of the prevalence and potential covariates or risk factors for anxiety and depression:
- In a systematic review and meta-analysis of 35 studies representing 11,396 caregivers of people with cancer, the pooled prevalence of depressive symptoms was 42.08% (95% confidence interval, 34.71%–49.45%). Studies were included in the meta-analysis if they used validated instruments to assess depression. However, the authors did not differentiate between studies that used cutoff scores associated with mild depressive symptoms and clinically significant depression.[17][Level of evidence: II]
- A telephone survey of 196 caregivers of patients with renal cell carcinoma studied the associations between psychological adjustment and caregivers’ experiences and unmet needs. Investigators demonstrated that 64% of caregivers had at least one significant unmet need, 53% had three or more unmet needs, and 29% had ten or more unmet needs.[18] Investigators found elevated anxiety in 29% of respondents and depression in 11%. Unmet information needs and worse experiences of care during surgery were risk factors for caregiver depression. Unmet information needs were the only risk factor for anxiety.
- A cross-sectional analysis assessed baseline data on caregivers of patients with advanced-stage lung or colorectal cancers enrolled in a randomized trial of early palliative care.[19] A significant proportion of caregivers reported elevated levels of anxiety (42.2%) or depression (21.5%). Risk factors for caregiver depression were patients’ expectation of cure and patients’ use of emotional support coping. Patients’ use of acceptance coping was associated with less caregiver anxiety. A study of caregivers of patients with pancreatic cancer reported similar results: 39% of caregivers had elevated levels of anxiety, and 14% had elevated levels of depression, compared with community norms.[20]
PTSD: One of the negative consequences of caregiving that persists is PTSD. A preliminary study of caregivers of patients with head and neck cancer 6 months after diagnosis demonstrated that approximately 20% met the criteria for PTSD.[21] Risk factors for PTSD included the following:
- Caregiver perception of low treatment benefit.
- Caregiver perception of many patient symptoms.
- Caregiver use of avoidant coping strategies.
The same investigators also showed in a similar population that differences in illness perceptions were dynamic over 6 months, but greater differences were correlated with reduced health-related quality of life (QOL) in patients.[22]
Decline in caregiver QOL: Several investigators have published measures of caregiver QOL while patients were undergoing active treatment. One study demonstrated that caregivers of patients undergoing hematopoietic stem cell transplant experience a decline in their QOL, as measured by the physical and mental component of the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36).[5]
Patients receiving palliative therapy also rely heavily on informal caregivers. In a study of 201 informal caregivers of patients undergoing palliative radiation therapy for advanced cancer, additional employment of the caregiver, cohabitation, poor patient performance status, and interest in accessing more support services were significantly correlated with higher caregiver burden (poorer QOL).[23]
In summary, a caregiver provides essential support and resources to the person with cancer. However, the role of informal caregiver creates demands that may exceed the caregiver’s resources and, ultimately, cause negative psychological consequences. The rest of this summary focuses on the significant minority of caregivers who experience unmet needs and increased physical and psychological distress. After a brief review of the concept of caregiver burden, information about the demands on caregivers, resources valued by caregivers, potential moderators of caregiver burden, and coping strategies will be presented.
References
- Caregiving in the U.S. 2020. Washington, DC: National Alliance for Caregiving, 2020. Available online. Last accessed May 1, 2025.
- Kim Y, Kashy DA, Kaw CK, et al.: Sampling in population-based cancer caregivers research. Qual Life Res 18 (8): 981-9, 2009. [PUBMED Abstract]
- Cancer Caregiving in the U.S.: An Intense, Episodic, and Challenging Care Experience. Bethesda, Md: National Alliance for Caregiving, 2016. Available online. Last accessed May 1, 2025.
- Litzelman K, Green PA, Yabroff KR: Cancer and quality of life in spousal dyads: spillover in couples with and without cancer-related health problems. Support Care Cancer 24 (2): 763-771, 2016. [PUBMED Abstract]
- El-Jawahri AR, Traeger LN, Kuzmuk K, et al.: Quality of life and mood of patients and family caregivers during hospitalization for hematopoietic stem cell transplantation. Cancer 121 (6): 951-9, 2015. [PUBMED Abstract]
- Kershaw T, Ellis KR, Yoon H, et al.: The Interdependence of Advanced Cancer Patients' and Their Family Caregivers' Mental Health, Physical Health, and Self-Efficacy over Time. Ann Behav Med 49 (6): 901-11, 2015. [PUBMED Abstract]
- Litzelman K, Kent EE, Mollica M, et al.: How Does Caregiver Well-Being Relate to Perceived Quality of Care in Patients With Cancer? Exploring Associations and Pathways. J Clin Oncol 34 (29): 3554-3561, 2016. [PUBMED Abstract]
- Mosher CE, Adams RN, Helft PR, et al.: Family caregiving challenges in advanced colorectal cancer: patient and caregiver perspectives. Support Care Cancer 24 (5): 2017-2024, 2016. [PUBMED Abstract]
- Libert Y, Merckaert I, Slachmuylder JL, et al.: The ability of informal primary caregivers to accurately report cancer patients' difficulties. Psychooncology 22 (12): 2840-7, 2013. [PUBMED Abstract]
- Mazer BL, Cameron RA, DeLuca JM, et al.: "Speaking-for" and "speaking-as": pseudo-surrogacy in physician-patient-companion medical encounters about advanced cancer. Patient Educ Couns 96 (1): 36-42, 2014. [PUBMED Abstract]
- Mosher CE, Adams RN, Helft PR, et al.: Positive changes among patients with advanced colorectal cancer and their family caregivers: a qualitative analysis. Psychol Health 32 (1): 94-109, 2017. [PUBMED Abstract]
- Von Ah D, Spath M, Nielsen A, et al.: The Caregiver's Role Across the Bone Marrow Transplantation Trajectory. Cancer Nurs 39 (1): E12-9, 2016 Jan-Feb. [PUBMED Abstract]
- Willard VW, Hostetter SA, Hutchinson KC, et al.: Benefit Finding in Maternal Caregivers of Pediatric Cancer Survivors: A Mixed Methods Approach. J Pediatr Oncol Nurs 33 (5): 353-60, 2016. [PUBMED Abstract]
- Hensler MA, Katz ER, Wiener L, et al.: Benefit finding in fathers of childhood cancer survivors: a retrospective pilot study. J Pediatr Oncol Nurs 30 (3): 161-8, 2013 May-Jun. [PUBMED Abstract]
- Kim Y, Schulz R, Carver CS: Benefit-finding in the cancer caregiving experience. Psychosom Med 69 (3): 283-91, 2007. [PUBMED Abstract]
- Kim Y, Carver CS, Schulz R, et al.: Finding benefit in bereavement among family cancer caregivers. J Palliat Med 16 (9): 1040-7, 2013. [PUBMED Abstract]
- Bedaso A, Dejenu G, Duko B: Depression among caregivers of cancer patients: Updated systematic review and meta-analysis. Psychooncology 31 (11): 1809-1820, 2022. [PUBMED Abstract]
- Oberoi DV, White V, Jefford M, et al.: Caregivers' information needs and their 'experiences of care' during treatment are associated with elevated anxiety and depression: a cross-sectional study of the caregivers of renal cancer survivors. Support Care Cancer 24 (10): 4177-86, 2016. [PUBMED Abstract]
- Nipp RD, El-Jawahri A, Fishbein JN, et al.: Factors associated with depression and anxiety symptoms in family caregivers of patients with incurable cancer. Ann Oncol 27 (8): 1607-12, 2016. [PUBMED Abstract]
- Janda M, Neale RE, Klein K, et al.: Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatology 17 (2): 321-327, 2017 Mar - Apr. [PUBMED Abstract]
- Richardson AE, Morton RP, Broadbent EA: Illness perceptions and coping predict post-traumatic stress in caregivers of patients with head and neck cancer. Support Care Cancer 24 (10): 4443-50, 2016. [PUBMED Abstract]
- Richardson AE, Morton RP, Broadbent EA: Changes over time in head and neck cancer patients' and caregivers' illness perceptions and relationships with quality of life. Psychol Health 31 (10): 1203-19, 2016. [PUBMED Abstract]
- Duimering A, Turner J, Chu K, et al.: Informal caregiver quality of life in a palliative oncology population. Support Care Cancer 28 (4): 1695-1702, 2020. [PUBMED Abstract]
Caregiver Burden
The term caregiver burden describes a caregiver’s perceptions of the demands of caregiving and the resources available for addressing those demands. The Transactional Model of Stress and Coping is a useful framework for describing the relationships among caregiver demands, resources, burden, and the psychological consequences of being burdened.[1] From this perspective, a burden is perceived when the demands on the caregiver exceed the resources available. See the figure below for an illustration of how this framework may be applied to caregiver burden.
The process begins with the primary appraisal, which is a judgment about the relevance of the health threat and any demands on the caregiver. A demand that is judged to be relevant receives a secondary appraisal to evaluate the likelihood that available resources have the potential to reduce or overcome the demand. Burden is perceived to be high when the difficulty of the demand outweighs the available resources. Coping strategies may also determine whether the psychological consequences of the perceived burden are negative or positive.
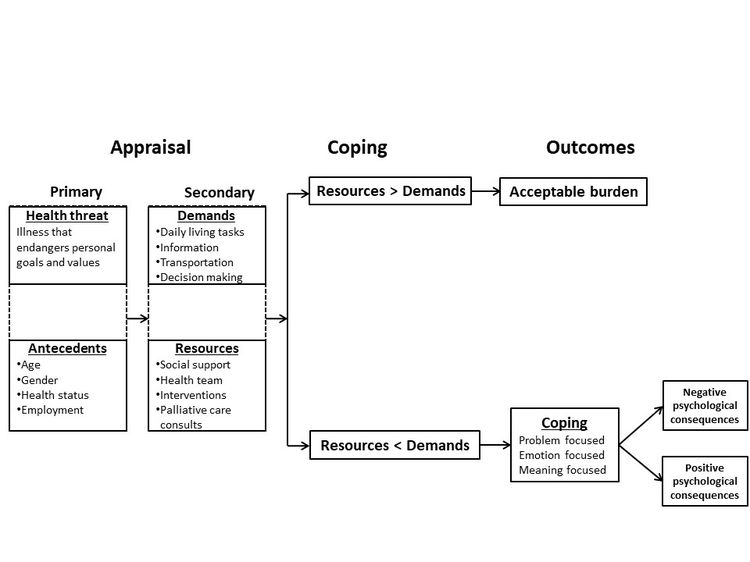
The Transactional Model of Stress and Coping shown above has not been validated and serves to organize the rest of the summary.
Primary Appraisal: Demands on Informal Caregivers
Qualitative analysis of interviews: A mixed-methods study of 48 informal caregivers of patients undergoing chemotherapy demonstrated several notable findings.[2] First, 68% of the caregivers had one or no unmet needs. A minority (23%) had five to ten unmet needs. Second, the most common needs were for information about the risks and potential benefits of chemotherapy (79%) and managing side effects at home (78%). Other information-related needs included information about self-care, complementary and alternative therapies, and local community-based resources.
Another group of investigators interviewed six patients with head and neck cancer and their spouses within 6 months of completing treatment. Thematic analysis identified several unmet needs, including the following:[3]
- Better preparation for side effects.
- Clearer timeline of recovery.
- Strategies to deal with the emotions experienced by patients and spouses during treatment.
The complexity of a caregiver’s life was further highlighted in a systematic review of qualitative studies of informal caregivers of patients with cancer and symptoms or signs of cachexia.[4] Several themes were identified:
- Impact on everyday life.
- Attempts of caregiver to take charge.
- Need for health care provider input.
- Conflict with patient.
- Negative emotions.
Surveys: To provide a more accurate assessment of caregiver needs, investigators developed and demonstrated the psychometric validity of the Supportive Care Needs Survey—Partners and Caregivers (SCNS–P&C).[5] More than 500 caregivers of patients enrolled in a cancer survivor study returned surveys for analysis. The mean age of caregivers was 60.6 years (range, 16–85 years).
The diagnoses of survivors included the following:
- Prostate cancer (32%).
- Blood cancer (16.3%).
- Breast cancer (13.2%).
- Melanoma (11.5%).
- Colorectal cancer (11.3%).
- Head and neck cancer (8.6%).
- Lung cancer (7.1%).
Analysis revealed four domains of needs:
- Health care service.
- Psychological and emotional.
- Work and social.
- Informational.
Investigators used the SCNS–P&C to conduct a telephone survey of 196 caregivers of patients with renal cell carcinoma. They found that 64% of caregivers had at least one significant unmet need, 53% had three or more unmet needs, and 29% had ten or more unmet needs.[6] For each domain of needs, the proportion of respondents reporting a moderate or high unmet need was:
- Health care service, 30%.
- Psychological and emotional, 30%.
- Work and social, 23%.
- Informational, 18%.
In another study, 188 patient-caregiver dyads completed the SCNS–P&C.[7] The caregivers were predominantly female Their average age was 57.8 years. Caregivers reported higher levels of distress and anxiety than patients. A minority (14%) reported no unmet needs, and a plurality (44%) reported ten or more unmet needs. The principal unmet caregiver needs were:
- Support in managing fears about the patient’s condition.
- Receiving disease-related information.
- Receiving emotional support for themselves.
There were no strong predictors of caregiver needs. However, unmet patient needs and caregiver anxiety were modestly associated with unmet needs in caregivers.
Similarly, the SCNS–P&C was administered to 166 lung cancer patient–caregiver dyads in Taiwan.[8] The top unmet needs were information needs.
Caregiver tasks: A cross-sectional study demonstrated that assisting patients in activities of daily living (ADLs) increased caregiver burden.[9] This study enrolled 100 caregivers of older adults (age >65 years) with cancer. The caregivers were mostly women, married to and living with the patients. Employment status and participation in ADLs were risk factors for increased burden on multivariate analysis. Similarly, a survey of 590 caregivers showed that primary caregivers assumed a significant workload.[10] As a consequence, they experienced challenges in maintaining employment and social relations, and had financial difficulties. On the other hand, primary caregivers experienced the most personal growth through their experiences. A subsequent systematic review supported the results of the two studies.[11] A more nuanced view is that the perceived burden and psychological consequences may relate to the sense of mastery for any given caregiver task.[12]
Secondary Appraisal: Resources for Informal Caregivers
This list captures the resources that caregivers identified in multiple studies as important:
- Recognition by health care providers of the informal caregivers’ roles, responsibilities, and challenges.
- Information about treatment plans, goals, anticipated complications or side effects, and likely outcomes.
- Guidance for how to respond to changes in patients’ physical and emotional health over the disease trajectory.
- Support in coping with the stress of caregiving (for which they are most often unprepared and untrained).
- Detailed education about medical and nursing tasks they are expected to perform, such as giving injections, providing wound care, and managing side effects.
Potential Moderators of Caregiver Burden
Factors associated with increased caregiver burden include the following:
- Female gender.
- Age (younger or older with impaired health status).
- Race and ethnicity.
- Lower socioeconomic status.
- Employment status.
- Role strain.
- Site of care.
- Patient characteristics (e.g., level of anxiety, depression, functional status, and quality of life [QOL]).[13][Level of evidence: II]
Female gender
Female gender is an established risk factor for increased burden.[14,15][Level of evidence: II] A survey of 308 self-identified caregivers of patients with advanced cancer sought to characterize potential determinants of the increased burden for female caregivers.[16] Results demonstrated that hope and perceived fulfillment of support needs were the most significant protective factors against burden for any gender. Women who were employed or who used emotion-focused coping were more likely to perceive burden. These results suggest that interventions to address role strain and alternative coping strategies may be useful.
Age
Family caregivers often feel unprepared, have inadequate knowledge, and receive little guidance from the oncology team for caring for a cancer patient.[17] Older caregivers are especially vulnerable because they may present with comorbidities, be living on fixed incomes, and have reduced social support networks. In addition, older caregivers of cancer patients may neglect their own health needs, have less time to exercise, forget to take their own prescription medications, and become fatigued from interrupted sleep. It is common for older caregivers to have poor physical health, depression, and even increased mortality.[18,19]
Younger caregivers generally juggle work, family responsibilities, and sacrifices involving their social lives. Middle-aged caregivers typically worry about missed workdays, interruptions at work, taking leaves of absence, and reduced productivity.[20,21]
Race and ethnicity
Differences among racial and ethnic groups in caregiver time commitment, levels of support and resources, and attitudes have been noted. In a meta-analysis of 116 empirical studies, Asian American caregivers provided more caregiving hours than White, African American, and Hispanic caregivers; used lower levels of formal support services; and had fewer financial resources, lower levels of education, and higher levels of depression than other groups.[22] These findings are important for the oncology team because caregivers with no outside help are more depressed than are those who receive help.
A study involving unmet needs and service barriers among Asian American caregivers found that caregivers refused outside help because they “felt too proud to accept it” or “didn’t want outsiders coming in.” Other barriers included “bureaucracy too complex” or “can’t find qualified providers.”[23] A study of hospice use by Asian American patients found that family reluctance to discuss a patient's health status among themselves resulted in lower rates of hospice enrollment. This reluctance was rooted in the belief that talking about death or dying is bad luck, which could complicate discussions about prognosis and informed consent.[24] Keeping a cancer diagnosis secret from a patient and avoiding discussions about disease progression can add to a caregiver’s sense of burden and responsibility.
Similarly, Hispanic and African American patients and caregivers underutilize community health resources, including counseling and support groups, home care, residential care, and hospice services. Strong family ties may prevent these caregivers from seeking help outside of the family unit.[25] A study that compared African American, White, and Hispanic caregivers found that 75% of Hispanic patients and 60% of African American patients lived with the family of the primary caregiver. The racial and ethnic minority families relied more on informal caregiving from friends and relatives and had larger social support networks than the White families. However, this increased sense of obligation to care for older family members was associated with more caregiving hours, greater resignation about caregiving, higher levels of caregiver strain, and a larger reduction in household income compared with White caregivers.[25,26] For more information, see the Disparities in Hospice Utilization section in Hospice.
Another study analyzed reports of employment loss due to caregiving responsibilities. Results showed that African American and Hispanic caregivers were more likely than White caregivers to reduce their work hours to care for patients. In addition, African American and Hispanic caregivers were reluctant to use formal nursing home services for their loved ones. The decision to reduce work hours rather than place a relative in a nursing home was associated with increased psychological, social, and financial burden.[27]
Socioeconomic status
Substantial out-of-pocket costs related to caregiving can create financial strain for the families of patients with cancer. Low personal and household incomes and limited financial resources may also place families at risk of treatment noncompliance or making treatment-related decisions based on income.[28]
Investigators assessed caregiver burden in 414 caregivers of older patients with advanced cancer in a secondary analysis of longitudinal data (at baseline, 4–6 weeks, and 3 months) collected during the Improving Communication in Older Cancer Patients and their Caregivers trial.[29][Level of evidence: II] The authors used the Caregiver Reaction Assessment, which includes five subscales measuring domains of caregiving burden: self-esteem, disrupted schedule, financial problems, lack of family support, and health problems. Also assessed was caregivers' rurality, defining rural residence as living in 2010 Rural-Urban Commuting Area Codes other than 1.0, 1.1, 2.0, 2.1, 3.0, 4.1, 5.1, 7.1, 8.1, or 10.1. In the analysis, rural residence was significantly associated with more disrupted schedules, financial problems, and lack of social support among caregivers with a high school education or less.
Employment status
Informal caregiving is known to impose economic burdens on families. One study analyzed data from 458 cancer survivors who responded to the U.S. Medical Expenditure Panel Survey (MEPS) Experiences with Cancer Survivorship Survey (ECSS) and from 4,706 cancer survivors who responded to the LIVESTRONG 2012 Survey for People Affected by Cancer (SPAC). Results demonstrated that 25% of those responding to the MEPS ECSS and 29% of those responding to the SPAC reported that their caregivers made extended employment changes, including taking paid or unpaid time off and making changes in hours, duties, or employment status.[30] The work productivity of 70 caregivers of patients with advanced cancer showed a 23% decline because of missed work.[31] More hours of caregiving were associated with greater loss in productivity, which was associated with higher rates of caregiver depression and anxiety. In a study of 89 caregivers of advanced-cancer patients, 69% of caregivers reported some form of adverse impact on work. This portion increased to 77% during the end-of-life period.[32]
Some research has shown an incremental increase in the economic burden of caregiving, assessed from disease and demographic characteristics. A study of 78 caregivers of women with advanced breast cancer showed that loss of productivity (absenteeism and reduced productivity at work) was greater for caregivers of women with progressive disease than for caregivers of those who were free of disease.[33] A survey of 1,629 caregivers of people with lung and colorectal cancers demonstrated that economic burden was highest for caregivers of individuals with lung cancer or stage IV disease.[34] In a study of 54 caregivers, African American and Hispanic caregivers reported greater distress related to employment and finances than White caregivers.[35] A study of partner caregivers of men with prostate cancer showed that caregivers with lower incomes (<$40,000/year) spent more time on informal caregiving than those with higher incomes.[36]
The Family and Medical Leave Act of 1993 was designed to give employees the option of taking time off from work for their own serious medical condition or that of a relative without losing their jobs or benefits.[37] Family members are entitled to a maximum of 12 weeks’ leave under the law.
Role strain
Role strain is experienced when the perceived rights, duties, and behaviors of one socially defined role (e.g., employee) conflict with the rights, duties, and behaviors of a different role (e.g., student). The multiple roles performed by caregivers of cancer patients can compete for caregivers’ physical and emotional resources. A study of 457 middle-aged caregivers showed that the more social roles a caregiver performed, the more likely the caregiver was to experience stress and negative affect.[38] In a population-based study of 1,234 adult-child and spousal caregivers of patients with lung or colorectal cancer, caregiver employment was associated with higher social/emotional caregiver burden.[39][Level of evidence: II] It is important to recognize, however, that employed caregivers may benefit from the respite provided by work and from the support of employers and coworkers, which enable them to replenish their psychological resources.[38] Thus, multiple roles do not always engender strain.
Site of care
Cancer care is provided in multiple locations that vary in their ability to provide support services for caregivers. Thus, site of care may be considered a risk factor for caregiver burden. This claim is further supported by the results of a qualitative interview study of 12 patients and 12 caregivers about the challenges faced in transitioning from hospital to home.[40] The investigators identified four salient themes:
- Ongoing concerns related to disease and its treatment.
- Needing timely help.
- Resuming control and normality.
- Appreciating the care transition.
An independent study of dyads demonstrated that the transition to home is stressful because of the need to deal with symptoms, and uncertainty about prognosis and disease progression.[41] Increased caregiver burden caused by transitions in sites of care should be recognized and ameliorated, when possible, with home nursing visits.
Unplanned changes in sites of care, such as hospital readmission, also place increased demands on caregivers. A total of 129 dyads of older adults with cancer and their family caregivers were studied to determine factors for unplanned hospital admissions.[42] Investigators found that severity of symptoms, rather than caregiver knowledge—a target of many interventions—predicted unplanned hospital admissions in older adults with cancer during the active treatment. These results suggest that symptom management interventions may reduce stressful events more than increasing caregiver knowledge about symptoms.
Patient characteristics
Patient characteristics may also influence caregiver burden. In a cross-sectional study of 441 older patient-caregiver dyads with advanced cancer, patients with higher levels of anxiety and depression, worse functional status, and poorer QOL were associated with increased reports of caregiver burden, regardless of time spent caregiving.[13][Level of evidence: II]
Similarly, in a cross-sectional study of 172 dyads of patients with advanced cancer and their caregivers, caregivers of patients admitted to an acute palliative care unit reported worse stress burden and mental health than caregivers of patients receiving outpatient supportive care.[43][Level of evidence: II]
References
- Lazarus RS, Folkman S: Stress, Appraisal, and Coping. Springer Publishing Co, 1984.
- Ream E, Pedersen VH, Oakley C, et al.: Informal carers' experiences and needs when supporting patients through chemotherapy: a mixed method study. Eur J Cancer Care (Engl) 22 (6): 797-806, 2013. [PUBMED Abstract]
- Badr H, Herbert K, Reckson B, et al.: Unmet needs and relationship challenges of head and neck cancer patients and their spouses. J Psychosoc Oncol 34 (4): 336-46, 2016 Jul-Aug. [PUBMED Abstract]
- Wheelwright S, Darlington AS, Hopkinson JB, et al.: A systematic review and thematic synthesis of quality of life in the informal carers of cancer patients with cachexia. Palliat Med 30 (2): 149-60, 2016. [PUBMED Abstract]
- Girgis A, Lambert S, Lecathelinais C: The supportive care needs survey for partners and caregivers of cancer survivors: development and psychometric evaluation. Psychooncology 20 (4): 387-93, 2011. [PUBMED Abstract]
- Oberoi DV, White V, Jefford M, et al.: Caregivers' information needs and their 'experiences of care' during treatment are associated with elevated anxiety and depression: a cross-sectional study of the caregivers of renal cancer survivors. Support Care Cancer 24 (10): 4177-86, 2016. [PUBMED Abstract]
- Sklenarova H, Krümpelmann A, Haun MW, et al.: When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121 (9): 1513-9, 2015. [PUBMED Abstract]
- Chen SC, Chiou SC, Yu CJ, et al.: The unmet supportive care needs-what advanced lung cancer patients' caregivers need and related factors. Support Care Cancer 24 (7): 2999-3009, 2016. [PUBMED Abstract]
- Hsu T, Loscalzo M, Ramani R, et al.: Factors associated with high burden in caregivers of older adults with cancer. Cancer 120 (18): 2927-35, 2014. [PUBMED Abstract]
- Lund L, Ross L, Petersen MA, et al.: Cancer caregiving tasks and consequences and their associations with caregiver status and the caregiver's relationship to the patient: a survey. BMC Cancer 14: 541, 2014. [PUBMED Abstract]
- Ge L, Mordiffi SZ: Factors Associated With Higher Caregiver Burden Among Family Caregivers of Elderly Cancer Patients: A Systematic Review. Cancer Nurs 40 (6): 471-478, 2017 Nov/Dec. [PUBMED Abstract]
- Stetz KM: Caregiving demands during advanced cancer. The spouse's needs. Cancer Nurs 10 (5): 260-8, 1987. [PUBMED Abstract]
- Semere W, Althouse AD, Rosland AM, et al.: Poor patient health is associated with higher caregiver burden for older adults with advanced cancer. J Geriatr Oncol 12 (5): 771-778, 2021. [PUBMED Abstract]
- Kim Y, van Ryn M, Jensen RE, et al.: Effects of gender and depressive symptoms on quality of life among colorectal and lung cancer patients and their family caregivers. Psychooncology 24 (1): 95-105, 2015. [PUBMED Abstract]
- Decadt I, Laenen A, Celus J, et al.: Caregiver distress and quality of life in primary caregivers of oncology patients in active treatment and follow-up. Eur J Cancer Care (Engl) 30 (3): e13399, 2021. [PUBMED Abstract]
- Schrank B, Ebert-Vogel A, Amering M, et al.: Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psychooncology 25 (7): 808-14, 2016. [PUBMED Abstract]
- Scherbring M: Effect of caregiver perception of preparedness on burden in an oncology population. Oncol Nurs Forum 29 (6): E70-6, 2002. [PUBMED Abstract]
- Given CW, Stommel M, Given B, et al.: The influence of cancer patients' symptoms and functional states on patients' depression and family caregivers' reaction and depression. Health Psychol 12 (4): 277-85, 1993. [PUBMED Abstract]
- Schulz R, Beach SR: Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA 282 (23): 2215-9, 1999. [PUBMED Abstract]
- Cameron JI, Franche RL, Cheung AM, et al.: Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer 94 (2): 521-7, 2002. [PUBMED Abstract]
- Given B, Sherwood PR: Family care for the older person with cancer. Semin Oncol Nurs 22 (1): 43-50, 2006. [PUBMED Abstract]
- Pinquart M, Sörensen S: Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist 45 (1): 90-106, 2005. [PUBMED Abstract]
- Li H: Barriers to and unmet needs for supportive services: experiences of Asian-American caregivers. J Cross Cult Gerontol 19 (3): 241-60, 2004. [PUBMED Abstract]
- Ngo-Metzger Q, McCarthy EP, Burns RB, et al.: Older Asian Americans and Pacific Islanders dying of cancer use hospice less frequently than older white patients. Am J Med 115 (1): 47-53, 2003. [PUBMED Abstract]
- Guarnaccia PJ, Parra P: Ethnicity, social status, and families' experiences of caring for a mentally ill family member. Community Ment Health J 32 (3): 243-60, 1996. [PUBMED Abstract]
- Cox C, Monk A: Strain among caregivers: comparing the experiences of African American and Hispanic caregivers of Alzheimer's relatives. Int J Aging Hum Dev 43 (2): 93-105, 1996. [PUBMED Abstract]
- Covinsky KE, Eng C, Lui LY, et al.: Reduced employment in caregivers of frail elders: impact of ethnicity, patient clinical characteristics, and caregiver characteristics. J Gerontol A Biol Sci Med Sci 56 (11): M707-13, 2001. [PUBMED Abstract]
- Hayman JA, Langa KM, Kabeto MU, et al.: Estimating the cost of informal caregiving for elderly patients with cancer. J Clin Oncol 19 (13): 3219-25, 2001. [PUBMED Abstract]
- Xu H, Kadambi S, Mohile SG, et al.: Caregiving burden of informal caregivers of older adults with advanced cancer: The effects of rurality and education. J Geriatr Oncol 12 (7): 1015-1021, 2021. [PUBMED Abstract]
- de Moor JS, Dowling EC, Ekwueme DU, et al.: Employment implications of informal cancer caregiving. J Cancer Surviv 11 (1): 48-57, 2017. [PUBMED Abstract]
- Mazanec SR, Daly BJ, Douglas SL, et al.: Work productivity and health of informal caregivers of persons with advanced cancer. Res Nurs Health 34 (6): 483-95, 2011. [PUBMED Abstract]
- Grunfeld E, Coyle D, Whelan T, et al.: Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 170 (12): 1795-801, 2004. [PUBMED Abstract]
- Lambert-Obry V, Gouault-Laliberté A, Castonguay A, et al.: Real-world patient- and caregiver-reported outcomes in advanced breast cancer. Curr Oncol 25 (4): e282-e290, 2018. [PUBMED Abstract]
- Van Houtven CH, Ramsey SD, Hornbrook MC, et al.: Economic burden for informal caregivers of lung and colorectal cancer patients. Oncologist 15 (8): 883-93, 2010. [PUBMED Abstract]
- Siefert ML, Williams AL, Dowd MF, et al.: The caregiving experience in a racially diverse sample of cancer family caregivers. Cancer Nurs 31 (5): 399-407, 2008 Sep-Oct. [PUBMED Abstract]
- Li C, Zeliadt SB, Hall IJ, et al.: Burden among partner caregivers of patients diagnosed with localized prostate cancer within 1 year after diagnosis: an economic perspective. Support Care Cancer 21 (12): 3461-9, 2013. [PUBMED Abstract]
- Chen ML: The Growing Costs and Burden of Family Caregiving of Older Adults: A Review of Paid Sick Leave and Family Leave Policies. Gerontologist 56 (3): 391-6, 2016. [PUBMED Abstract]
- Kim Y, Baker F, Spillers RL, et al.: Psychological adjustment of cancer caregivers with multiple roles. Psychooncology 15 (9): 795-804, 2006. [PUBMED Abstract]
- Fenton ATHR, Keating NL, Ornstein KA, et al.: Comparing adult-child and spousal caregiver burden and potential contributors. Cancer 128 (10): 2015-2024, 2022. [PUBMED Abstract]
- Ang WH, Lang SP, Ang E, et al.: Transition journey from hospital to home in patients with cancer and their caregivers: a qualitative study. Support Care Cancer 24 (10): 4319-26, 2016. [PUBMED Abstract]
- Rocío L, Rojas EA, González MC, et al.: Experiences of patient-family caregiver dyads in palliative care during hospital-to-home transition process. Int J Palliat Nurs 23 (7): 332-339, 2017. [PUBMED Abstract]
- Geddie PI, Wochna Loerzel V, Norris AE: Family Caregiver Knowledge, Patient Illness Characteristics, and Unplanned Hospital Admissions in Older Adults With Cancer. Oncol Nurs Forum 43 (4): 453-63, 2016. [PUBMED Abstract]
- Tanco K, Prado B, Qian Y, et al.: A Comparison of Caregiver Burden of Patients with Advanced Cancer in Different Palliative Cancer Care Settings. J Palliat Med 24 (12): 1766-1775, 2021. [PUBMED Abstract]
Coping Strategies and Self-Efficacy
As conceptualized, coping strategies mediate the relationship between positive or negative consequences and the perception that the demands of caregiving exceed the available resources. One group of investigators interviewed and surveyed 50 family caregivers of cancer patients receiving palliative care.[1] The aim was to describe the relationships between coping strategies and anxiety in caregivers. Anxiety was common in caregivers (76%). Emotion-based coping was associated with less anxiety, while dysfunctional coping was associated with increased anxiety. Perceived burden was also associated with increased anxiety.
As shown in the Transactional Model of Stress and Coping, caregivers and patients are interconnected. Evidence demonstrates a link between patient coping style and caregiver adjustment. A cross-sectional study of baseline data from a trial of subspecialty palliative care confirmed the relationship in 275 family caregivers of patients with incurable lung or colorectal cancer.[2] The investigators demonstrated that caregivers experienced greater depressive symptoms when patients used emotional support coping or expressed optimism about their prognosis. Among patients, less use of emotional support coping was associated with greater caregiver anxiety.
This interconnectedness between caregiver and patient also involves threat appraisal (the first step in the Transactional Model of Stress and Coping). A study of 484 dyads demonstrated that patient and caregiver symptom distress influenced their own, and in some cases each other’s, cognitive appraisals.[3]
References
- Perez-Ordóñez F, Frías-Osuna A, Romero-Rodríguez Y, et al.: Coping strategies and anxiety in caregivers of palliative cancer patients. Eur J Cancer Care (Engl) 25 (4): 600-7, 2016. [PUBMED Abstract]
- Nipp RD, El-Jawahri A, Fishbein JN, et al.: Factors associated with depression and anxiety symptoms in family caregivers of patients with incurable cancer. Ann Oncol 27 (8): 1607-12, 2016. [PUBMED Abstract]
- Ellis KR, Janevic MR, Kershaw T, et al.: The influence of dyadic symptom distress on threat appraisals and self-efficacy in advanced cancer and caregiving. Support Care Cancer 25 (1): 185-194, 2017. [PUBMED Abstract]
Assessment of Caregivers
Caregiver assessment can be performed at any point of contact within the health care system. Ideally, a comprehensive caregiver assessment should be performed when the following occurs:[1]
- The patient is first diagnosed with cancer.
- The patient presents in the emergency department.
- A major transition is planned.
In systems where caregivers are assessed, practitioners can acknowledge caregivers as valued members of the health care team. Caregiver assessment can identify family members most at risk of developing physical and mental health difficulties, so that additional services can be planned accordingly.[1]
Multiple instruments to measure caregiver burden are available, including the Zarit Burden Interview,[2] among others.[3-10] Objective measures of caregiver burden comprise variables such as the number of hours spent providing care and a count of tasks the caregiver performs.[11][Level of evidence: II][12] Objective measures are usually short and easy to answer, often pointing to a clear direction for problem solving and direct intervention.[13] Caregiver assessment should reflect culturally competent practices.[14]
Although there are many tools for measuring caregiver burden, a review [15] found only eight tools in English for the psychometric evaluation of cancer caregivers. Of the eight, the Caregiver Reaction Assessment and Caregiver Quality of Life Index-Cancer had the best psychometric performance. Additionally, 16 conceptual domains within five overarching themes were identified across the eight instruments. Although the tools showed overlap in several domains, no single tool measured all domains. In assessing caregiver burden, it is prudent to use two or more instruments to obtain an evaluation across all domains.
References
- Feinberg LF: Caregiver assessment. Am J Nurs 108 (9 Suppl): 38-9, 2008. [PUBMED Abstract]
- Zarit SH, Reever KE, Bach-Peterson J: Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 20 (6): 649-55, 1980. [PUBMED Abstract]
- Glajchen M, Kornblith A, Homel P, et al.: Development of a brief assessment scale for caregivers of the medically ill. J Pain Symptom Manage 29 (3): 245-54, 2005. [PUBMED Abstract]
- Weitzner MA, Jacobsen PB, Wagner H, et al.: The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res 8 (1-2): 55-63, 1999. [PUBMED Abstract]
- Weitzner MA, McMillan SC: The Caregiver Quality of Life Index-Cancer (CQOLC) Scale: revalidation in a home hospice setting. J Palliat Care 15 (2): 13-20, 1999. [PUBMED Abstract]
- Given CW, Given B, Stommel M, et al.: The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 15 (4): 271-83, 1992. [PUBMED Abstract]
- Robinson BC: Validation of a Caregiver Strain Index. J Gerontol 38 (3): 344-8, 1983. [PUBMED Abstract]
- Minaya P, Baumstarck K, Berbis J, et al.: The CareGiver Oncology Quality of Life questionnaire (CarGOQoL): development and validation of an instrument to measure the quality of life of the caregivers of patients with cancer. Eur J Cancer 48 (6): 904-11, 2012. [PUBMED Abstract]
- Wells DK, James K, Stewart JL, et al.: The care of my child with cancer: a new instrument to measure caregiving demand in parents of children with cancer. J Pediatr Nurs 17 (3): 201-10, 2002. [PUBMED Abstract]
- Zaleta AK, Miller MF, Fortune EE, et al.: CancerSupportSourceTM -Caregiver: Development of a distress screening measure for cancer caregivers. Psychooncology 32 (3): 418-428, 2023. [PUBMED Abstract]
- Bookwala J, Schulz R: A comparison of primary stressors, secondary stressors, and depressive symptoms between elderly caregiving husbands and wives: the Caregiver Health Effects Study. Psychol Aging 15 (4): 607-16, 2000. [PUBMED Abstract]
- Gaugler JE, Hanna N, Linder J, et al.: Cancer caregiving and subjective stress: a multi-site, multi-dimensional analysis. Psychooncology 14 (9): 771-85, 2005. [PUBMED Abstract]
- Honea NJ, Brintnall R, Given B, et al.: Putting Evidence into Practice: nursing assessment and interventions to reduce family caregiver strain and burden. Clin J Oncol Nurs 12 (3): 507-16, 2008. [PUBMED Abstract]
- Pinquart M, Sörensen S: Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist 45 (1): 90-106, 2005. [PUBMED Abstract]
- Shilling V, Matthews L, Jenkins V, et al.: Patient-reported outcome measures for cancer caregivers: a systematic review. Qual Life Res 25 (8): 1859-76, 2016. [PUBMED Abstract]
The Needs of Caregivers During the Cancer Trajectory
The cancer experience can be viewed in several distinct phases, from screening to diagnosis to treatment to either long-term survivorship or the end of life.[1] The phases differ in likely activities, goals, and outcomes for the patient. It seems reasonable to assume that the experiences of the caregiver also vary, given the interdependence of caregiver and patient.
Studies Comparing Caregivers at Different Points in the Cancer Trajectory
Few studies directly compare caregivers of cancer patients across the disease trajectory or patients at different stages of disease. One research group conducted a qualitative study and interviewed 15 cancer caregivers before, during, and 4 months after bone marrow transplant. Although the exemplars varied across the trajectory, two consistent themes emerged: caregivers' uncertainty and the need for more information.[2]
Another study compared the results of two cross-sectional studies of caregivers of cancer patients who were in the late palliative phase or were attending a pain clinic (which the authors termed the curative phase).[3] The authors found no differences in the mean scores of the Hospital Anxiety and Depression Scale or the Medical Outcomes Study 36-Item Short Form Health Survey as measures of quality of life (QOL). The results should be interpreted with caution, given the different inclusion criteria and different time periods of the study. Furthermore, the group means may obscure meaningful changes in individual caregivers over time.
A separate analysis demonstrated that symptom burdens in patients did not vary between cohorts, but both groups scored high on measures of weakness and fatigue.[4] Caregivers reported higher rates of depression when patients had insomnia, but the association did not vary between cohorts. However, the methodology of the studies limits the drawing of firm conclusions.
In a cross-sectional study of 1,580 caregivers of patients with different cancer types, caregivers of patients undergoing active treatment had a significantly lower mean score on the Distress Thermometer than caregivers of patients in follow-up.[5][Level of evidence: II] Mean scores on another measure of caregiver distress, the Caregiver Risk Screen, were not significantly different across groups. Conversely, caregivers of patients undergoing active treatment reported significantly worse QOL on the Caregiver Quality of Life Index–Cancer than caregivers of patients in follow-up. One possible explanation for these findings is that while patients’ physical and practical needs may decrease after treatment, caregivers may experience heightened uncertainty and fear of cancer recurrence during survivorship.[6,7]
Survivorship
The evidence demonstrates that although the prevalence of unmet needs diminishes over time, many caregivers continue to experience needs related to the cancer experience during the survivorship phase.
For example, a longitudinal study was designed to track the psychosocial, financial, and occupational impact of having ongoing needs as a caregiver in Australia.[8] The investigators analyzed responses to the Supportive Care Needs Survey—Partners and Caregivers (SCNS–P&C) from 547 caregivers at 6 months, 519 caregivers at 12 months, and 443 caregivers at 24 months after the cancer diagnosis. Of note, 444 of the original 547 participants completed surveys at 12 months, and 372 completed surveys at 24 months.
Several findings deserve emphasis:
- The proportion of caregivers reporting any unmet need decreased from 50.2% at 6 months to 30.7% at 24 months.
- A similar decline was seen for caregivers who reported at least five or ten unmet needs, although the baseline prevalence was lower.
- The most pressing unmet needs were related to concerns about cancer recurrence, reducing stress in the survivor’s life, and understanding the survivor’s experience.
- Unmet needs were negatively associated with caregivers’ well-being (although not uniformly).
In a longitudinal study of 120 dyads of patients with hepatobiliary or pancreatic cancer and their caregivers, at diagnosis 25% of caregivers reported high levels of chronic depressive symptoms, and 21% had high levels of stress.[9][Level of evidence: II] Levels of depressive symptoms and stress at diagnosis remained high up to 18 months postdiagnosis, while those with low to moderate levels of depressive symptoms and stress at diagnosis saw those levels decline over time. Patient depressive symptoms also predicted caregiver stress. These findings suggest that caregivers with higher levels of depressive symptoms and stress at diagnosis may be the most vulnerable over time, but further research is needed in more diverse samples, as most caregivers were women (85%). Similarly, a 2021 study found that in 111 caregivers of newly diagnosed cancer patients, poorer caregiver QOL was associated with higher levels of caregiver depression, anxiety, and stress, and that caregiver QOL and levels of social support changed over the treatment trajectory.[10][Level of evidence: II]
End of Life
The end-of-life experiences of patients with advanced cancer influence the burden on caregivers and their eventual psychological adjustment during bereavement. A longitudinal study of caregivers of women with advanced-stage ovarian cancer provides valuable insights into the caregiver’s experience in the last year of the patient’s life.[11] Ninety-nine caregivers completed measures every 3 months for 2 years. The caregivers reported lower-than-expected mental and physical QOL. The average distress level and number of unmet needs increased over time. Perceived social support did not change. Caregiver distress was predicted by lower optimism, higher unmet needs, and shortened time to patient death. Patient QOL was not a predictor. In the last 6 months of the patient’s life, managing emotions about poor prognosis and balancing work with caregiving demands were related to high unmet needs among caregivers.
One potential source of caregiver distress toward the end of life is the ambiguity around caregivers' role in decisions to limit potentially life-sustaining treatments such as chemotherapy or resuscitation. Two studies provide clarifying observations.[12,13] One study embedded researchers during hospitalizations of patients with advanced cancer to record the participation of caregivers in decisions to limit treatment.[12] The investigators identified 70 patients, but only 63 had caregivers present. In the cohort, only 32% of relatives were involved, both positively and negatively. Clinicians were more often aware of patients’ preferences when relatives were present (78% vs. 29%, P = .014). However, caregivers did not always agree with patients and, in one-third of the observations, contradicted the patients. Thus, caregivers may be a source of insight but do not necessarily accurately reflect patients’ wishes.
The caregiver’s importance to the decision-making process may vary based on clinicians’ attitudes. In an interview study of oncology physicians and nurses, two broad perspectives were found: maintaining patient autonomy independent of caregiver influence and facilitating decision-making by actively involving caregivers seeking consensus.[13] These perspectives were based on a desire to enhance the positive aspects of caregivers’ support (e.g., emotional, encouragement to plan, and understanding of information) while minimizing the potential barriers (e.g., family reluctance to accept the patient is at the end of life, the need to mediate conflicts, and the increased time required to include caregivers). These findings highlight the potential value of caregivers and the need to develop specific strategies for including them in end-of-life discussions.
Hospice care can provide critical support to caregivers as well as patients. One group of investigators compared the burden and QOL of caregivers of patients with advanced cancer who were receiving active treatment with the burden and QOL of caregivers of patients who were receiving hospice care.[14] The goal was to characterize the demands unique to the hospice phase of care. The investigators found no difference in the perceived burden of caregiving and increased role limitations due to mental or emotional challenges. However, caregivers in the hospice group reported fewer physical limitations. Similarly, another group reported that longer hospice stays were associated with better patient QOL and better caregiver adjustment during bereavement.[15]
A potential explanation for the benefit of hospice is that caregivers are reassured by the higher quality of end-of-life care and the honoring of patients’ goals. One study analyzed interviews with 1,146 family members of Medicare beneficiaries who died of advanced-stage lung or colorectal cancer.[16] The results demonstrated that hospice enrollment was associated with more “excellent” ratings for quality of care reported by family members. Similarly, patients who received intensive care or had short hospice enrollments were less frequently reported to have died in their preferred place.[17] For more information, see Hospice.
Caregivers may also require support to effectively participate in decisions about whether to provide patients with artificial nutrition or hydration (ANH). Investigators conducted a prospective cross-sectional survey of 39 patients with advanced cancer and 30 relatives about their views on ANH.[18] Only 24% of relatives stated they would opt out of ANH if deciding on behalf of their loved ones, and 48% were against hydration. Patients were less concerned than their relatives about adverse physical symptoms such as pain, agitation, and hunger. Patients endorsed their family members’ opinions as important in these decisions. For more information, see the Artificial Hydration section in Last Days of Life.
References
- Levit LA, Balogh EP, Nass SJ, et al., eds.: Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. The National Academies Press, 2013. Also available online. Last accessed May 1, 2025.
- Von Ah D, Spath M, Nielsen A, et al.: The Caregiver's Role Across the Bone Marrow Transplantation Trajectory. Cancer Nurs 39 (1): E12-9, 2016 Jan-Feb. [PUBMED Abstract]
- Grov EK, Valeberg BT: Does the cancer patient's disease stage matter? A comparative study of caregivers' mental health and health related quality of life. Palliat Support Care 10 (3): 189-96, 2012. [PUBMED Abstract]
- Valeberg BT, Grov EK: Symptoms in the cancer patient: of importance for their caregivers' quality of life and mental health? Eur J Oncol Nurs 17 (1): 46-51, 2013. [PUBMED Abstract]
- Decadt I, Laenen A, Celus J, et al.: Caregiver distress and quality of life in primary caregivers of oncology patients in active treatment and follow-up. Eur J Cancer Care (Engl) 30 (3): e13399, 2021. [PUBMED Abstract]
- Shilling V, Starkings R, Jenkins V, et al.: The pervasive nature of uncertainty-a qualitative study of patients with advanced cancer and their informal caregivers. J Cancer Surviv 11 (5): 590-603, 2017. [PUBMED Abstract]
- Balfe M, O'Brien K, Timmons A, et al.: The unmet supportive care needs of long-term head and neck cancer caregivers in the extended survivorship period. J Clin Nurs 25 (11-12): 1576-86, 2016. [PUBMED Abstract]
- Girgis A, Lambert SD, McElduff P, et al.: Some things change, some things stay the same: a longitudinal analysis of cancer caregivers' unmet supportive care needs. Psychooncology 22 (7): 1557-64, 2013. [PUBMED Abstract]
- Chen Q, Terhorst L, Geller DA, et al.: Trajectories and predictors of stress and depressive symptoms in spousal and intimate partner cancer caregivers. J Psychosoc Oncol 38 (5): 527-542, 2020 Sep-Oct. [PUBMED Abstract]
- Peh CX, Liu J, Mahendran R: Quality of life and emotional distress among caregivers of patients newly diagnosed with cancer: Understanding trajectories across the first year post-diagnosis. J Psychosoc Oncol 38 (5): 557-572, 2020 Sep-Oct. [PUBMED Abstract]
- Butow PN, Price MA, Bell ML, et al.: Caring for women with ovarian cancer in the last year of life: a longitudinal study of caregiver quality of life, distress and unmet needs. Gynecol Oncol 132 (3): 690-7, 2014. [PUBMED Abstract]
- Hauke D, Reiter-Theil S, Hoster E, et al.: The role of relatives in decisions concerning life-prolonging treatment in patients with end-stage malignant disorders: informants, advocates or surrogate decision-makers? Ann Oncol 22 (12): 2667-2674, 2011. [PUBMED Abstract]
- Laryionava K, Hauke D, Heußner P, et al.: "Often Relatives are the Key […]" -Family Involvement in Treatment Decision Making in Patients with Advanced Cancer Near the End of Life. Oncologist 26 (5): e831-e837, 2021. [PUBMED Abstract]
- Spatuzzi R, Giulietti MV, Ricciuti M, et al.: Quality of life and burden in family caregivers of patients with advanced cancer in active treatment settings and hospice care: A comparative study. Death Stud 41 (5): 276-283, 2017 May-Jun. [PUBMED Abstract]
- Wright AA, Zhang B, Ray A, et al.: Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300 (14): 1665-73, 2008. [PUBMED Abstract]
- Wright AA, Keating NL, Ayanian JZ, et al.: Family Perspectives on Aggressive Cancer Care Near the End of Life. JAMA 315 (3): 284-92, 2016. [PUBMED Abstract]
- Wright AA, Keating NL, Balboni TA, et al.: Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. J Clin Oncol 28 (29): 4457-64, 2010. [PUBMED Abstract]
- Bükki J, Unterpaul T, Nübling G, et al.: Decision making at the end of life--cancer patients' and their caregivers' views on artificial nutrition and hydration. Support Care Cancer 22 (12): 3287-99, 2014. [PUBMED Abstract]
Interventions to Prevent, Reduce, or Ameliorate Caregiver Burden
Many types of interventions have been tested to address the needs of informal caregivers.[1-3] The interventions have focused on improving outcomes for the individual patient, caregiver, or patient-caregiver dyad.[1] The types of interventions and their goals include the following:
- Cognitive behavioral therapy (CBT): To use psychoeducational and social interventions to reduce caregiver burden and feelings of distress.
- Complementary and alternative medicine therapies: To reduce caregiver distress and burden through guided imagery, reflexology, reminiscence therapy, massage therapy, and healing touch.
- Family/couples therapy: To improve the functioning of the couple and family unit.
- Interpersonal therapy: To provide individual counseling to reduce the psychological consequences of caregiving burdens.
- Problem solving and skill building: To develop caregiving skills, including the ability to assess and manage patients’ symptoms, identify solutions to caregiving problems, and enhance caregivers’ ability to cope with cancer caregiving roles and responsibilities.
- Psychoeducational: To address the information needs of cancer caregivers, including information related to diagnosis, prognosis, coping, self-care, home care, impact on partners and family, and hospital care or follow-up and rehabilitation.[4]
- Subspecialty palliative care: To directly address caregivers’ concerns and improve their outcomes by improving patient outcomes.
- Supportive therapy: To address the emotional needs of informal caregivers.
The efficacy of these interventions has been mixed. Findings from a few meta-analyses have identified small to medium positive effects of psychosocial-educational interventions on caregivers and on patient-caregiver outcomes.[5-7] However, many studies are limited by small sample sizes and short assessments, and outcomes often vary depending on the study focus (patient vs. caregiver vs. patient-caregiver dyads).[1]
Meta-analyses
One meta-analysis of 29 randomized clinical trials published from 1983 to 2009 [6] identified the following three major types of interventions:
- Psychoeducational.
- Skill building/problem solving.
- Therapeutic counseling.
The authors used a conceptual framework to organize the outcome data, integrating stress and coping theory, CBT, and quality of life (QOL) frameworks. Overall, all three interventions showed small to moderate effects for improving the following outcomes:
- Caregiver burden (11 studies; overall effect size, Hedge's g [g] = 0.22).
- Caregivers’ ability to cope (10 studies; overall effect size, g = 0.47 within the first 3 months, which remained significant 3 to 6 months later [overall effect size, g = 0.20] and 6 months later [g = 0.35]).
- Self-efficacy (8 studies; overall effect size, g = 0.25, which remained significant at 3 to 6 months’ follow-up [g = 0.20] and beyond).
- Aspects of QOL, including physical functioning (7 studies; g = 0.22 at 3 to 6 months’ follow-up and g = 0.26 at 6 months’ follow-up), distress and anxiety (16 studies; g = 0.20 during the first 3 months), and marital/family relationships (10 studies; g = 0.20). There was no significant improvement in depression or social functioning.
A follow-up systematic review of the literature identified 49 intervention studies that addressed caregiver demands and burden.[3] Eight different types of interventions were noted, with most studies categorized as psychoeducational, problem solving, supportive therapy, and family and couples therapy. The authors noted only three studies that used CBT. However, all three studies using CBT noted significant improvement in psychological functioning in informal caregivers. Overall, programs that were structured, integrative, and goal oriented appeared to offer the greatest benefits.[3]
This initial work was expanded upon with a synthesis and meta-analyses of the effectiveness of CBT for improving psychological functioning in informal caregivers.[2] The authors identified a small statistical effect of CBT (g = 0.08). However, this effect disappeared when randomized controlled trials were reviewed alone. The authors suggested that the broad definition of CBT and variations in the definition of informal caregivers may have limited results.[2]
Two additional reviews focused on literature published up until 2016.[8,9] One group of investigators conducted a systematic review of 21 psychosocial interventions for improving QOL, depression, and anxiety in cancer caregivers.[8] This report and others have illustrated some noteworthy interventions used in multiple studies.
- Psychoeducational intervention: The FOCUS Program is an informational and support program that includes five core content areas: Family involvement, Optimistic attitude, Coping effectiveness, Uncertainty reduction, and Symptom management. This intervention has shown improvement in caregiver QOL in multiple randomized controlled trials.[10,11]
- Problem-solving intervention: COPE (Creativity, Optimism, Planning, Expert Information) is a problem-solving model, used by multiple investigators, that has shown improvement in caregiver QOL,[12,13] burden of patient symptoms, and caregiving task burden.[12] This program has also been used in combination with other cognitive behavioral trials with some success.[14]
- Psychoeducational and supportive therapy: CHESS (Comprehensive Health Enhancement Support System) is a web-based lung cancer information, communication, and coaching system for caregivers.[15] This program was tested in 285 informal caregivers of patients with advanced non-small cell lung cancer. Caregivers were randomly assigned to one of two groups. The comparison group received standard care plus a laptop computer with Internet access (if needed) and a list of lung cancer and palliative care websites. The treatment group received standard care plus a laptop computer and Internet access (if needed) and access to the CHESS lung cancer website, “Coping with Lung Cancer: A Network of Support.” Caregivers assigned to CHESS had small to moderate but significant effects in improved caregiver burden and negative mood. This study is a good example of using the Web to reach informal caregivers, who often cannot attend supportive training programs in person.
Individual Studies
A few individual landmark studies have examined interventions for informal caregivers of people with cancer.
Overview of study limitations and unresolved questions
A number of limitations in studies to date prevent any conclusions about choosing an optimal intervention. Salient limitations include the following:
- The variation in intervention delivery across studies, from in-person sessions to telephone, online, or web-based applications.
- The lack of consensus regarding the definition of informal caregivers and types of interventions, making comparisons across studies difficult.
- The potential lack of scalability of interventions studied in a limited number of sites, leaving the unanswered question of how to provide interventions to rural populations and those with transportation concerns.
- The frequent lack of a match between the primary outcome measure and the target of the intervention. For example, interventions focused on problem solving often failed to assess improvement in the capacity to solve problems but instead measured more distal outcomes such as psychological adjustment. Such studies raise questions about attributing intervention effects.
- The unrecognized variations in the levels of caregiver burden or distress among study participants. Researchers noted that informal caregivers who were most distressed were more likely to decline to enroll in a trial or, if enrolled, often failed to complete the intervention, which affected the evaluation. In addition, investigators have suggested that efficacy has varied because of low baseline levels of caregiver burden and distress or inadequate follow-up, resulting in the inability to identify changes in levels of distress.
These limitations can be addressed in future studies:
- Use consensus definitions for informal caregivers and interventional categories.[2]
- Identify more-vulnerable caregiving populations (e.g., socially isolated caregivers, rural residents, older people, members of lower socioeconomic groups, and people with the most complicated care and needs).[1]
- Incorporate risk stratification to target highly stressed informal caregivers and patients.[1] Future studies may focus on those most in need to adequately demonstrate intervention effectiveness.
- Incorporate technology not only to improve interventions but also to improve access to interventional support.[1]
Overview of results of selected studies
The following two tables contain brief descriptions of noteworthy reports to aid in understanding potential interventions and benefits. Table 1 organizes studies by type of intervention and highlights positive and negative studies. As outlined in the previous section, however, methodological limitations prevent comparisons or conclusions.[1]
| Intervention Type | Positive Results | Negative Results |
|---|---|---|
| IC = informal caregiver; N/A = not applicable; QOL = quality of life. | ||
| Psychoeducation | Improved knowledge and/or ability to provide care [16-22] | Unimproved mood (anxiety and distress) [23] |
| Improved psychological functioning (depression, anxiety, stress) and reduced caregiver burden [15,24-27] | No significant improvement in caregiver burden [28] | |
| Improved patient-reported functional support and marital satisfaction [24] | Unimproved QOL [29] | |
| Improved coping and mental health, decreased depressive symptoms, and lower risk of maladaptive coping [30] | N/A | |
| Problem solving/skill building | Improved problem solving [31-36] | No decrease in IC depressive symptoms [37,38] |
| Improved IC confidence,[32] self-efficacy [36,37,39] | No improvement in IC coping or help seeking [40] | |
| Improved psychological functioning (decreased IC depressive symptoms,[33] anxiety,[35] distress,[36] and negative affect [34]) | ||
| Decreased patient depressive symptoms [33] | ||
| Improved health outcomes (fatigue) [36] | ||
| Improved QOL [35] | ||
| Supportive therapy | Improved IC perception of support/knowledge [41] | No significant improvement in IC psychological functioning (depression, anxiety) [37,42] |
| Unimproved IC QOL [37,43] | ||
| Family/couples therapy | Improved marital functioning/relationships [44,45] | Unimproved state anxiety or traumatic stress or distress [46] |
| Less IC-reported negative appraisals of caregiving [10,47] | ||
| Improved communication skills [47] | ||
| Improved psychological functioning (distress, depression, anxiety in ICs, patients) [45,48,49] | ||
| Improved QOL [11,50] | ||
| Cognitive behavioral therapy | Improved psychological functioning (reductions in distress, depressive symptoms) [51-53] | N/A |
| Decreased burden of cancer symptoms [12] | ||
| Improved self-efficacy [54] | ||
| Improved QOL [12] | ||
| Interpersonal therapy | Improved psychological functioning (decreased depression, anxiety) [55,56] | N/A |
| Improved QOL [56,57] | ||
| Integrative, alternative, and complementary therapy | Massage: improvements in IC depression, anxiety, fatigue [58] | N/A |
| Strength training: improvements in mental health but approaching statistical significance [59] | ||
| Mindfulness-based stress reduction: | ||
| – Reduced caregiver burden but no significant reduction in psychological distress for patients and partners [60] | ||
| – Significant improvement in patient psychological functioning (decreased stress, anxiety) and reduction but no statistical improvement in IC psychological functioning and QOL [61] | ||
Table 2 highlights some of the investigational studies that support the effectiveness of psychoeducational, problem-solving, and CBT interventions in which most of the work has been conducted. In addition, the table displays the outcomes (resources and coping) that were improved in each of these studies.
| Intervention Type/References | Outcomes: Improved Resources and/or Coping | |||||
|---|---|---|---|---|---|---|
| QOL = quality of life. | ||||||
| Psychoeducation | Knowledge of care/role | Problem solving | Self-efficacy | Psychological functioning | Symptoms | QOL |
| – Ferrell et al., 1995 [16] | X | |||||
| – Horowitz et al., 1996 [25] | X | X | ||||
| – DuBenske et al., 2014 [15] | X | |||||
| – Northouse et al., 2013 [11] | X | X | ||||
| – Northouse et al., 2014 [50] | X | X | X | |||
| – Badr et al., 2015 [26] | X | |||||
| Problem solving | Knowledge of care/role | Problem solving | Self-efficacy | Psychological functioning | Symptoms | QOL |
| – Sahler et al., 2002 [34] | X | X | X | |||
| – Nezu et al., 2003 [33] | X | X | X | |||
| – Cameron et al., 2004 [32] | X | X | X | |||
| – Bevans et al., 2010 [31] | X | X | ||||
| – Demiris et al., 2012 [35] | X | X | X | |||
| – Bevans et al., 2014 [36] | X | X | X | X | ||
| Cognitive behavioral therapy | Knowledge of care/role | Problem solving | Self-efficacy | Psychological functioning | Symptoms | QOL |
| – Keefe et al., 2005 [54] | X | |||||
| – Carter, 2006 [51] | X | |||||
| – Cohen et al., 2006 [52] | X | |||||
| – Given et al., 2006 [53] | X | X | ||||
| – McMillan et al., 2006 [12] | X | X | ||||
References
- Kent EE, Rowland JH, Northouse L, et al.: Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer 122 (13): 1987-95, 2016. [PUBMED Abstract]
- O'Toole MS, Zachariae R, Renna ME, et al.: Cognitive behavioral therapies for informal caregivers of patients with cancer and cancer survivors: a systematic review and meta-analysis. Psychooncology 26 (4): 428-437, 2017. [PUBMED Abstract]
- Applebaum AJ, Breitbart W: Care for the cancer caregiver: a systematic review. Palliat Support Care 11 (3): 231-52, 2013. [PUBMED Abstract]
- Adams E, Boulton M, Watson E: The information needs of partners and family members of cancer patients: a systematic literature review. Patient Educ Couns 77 (2): 179-86, 2009. [PUBMED Abstract]
- Badr H, Krebs P: A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psychooncology 22 (8): 1688-704, 2013. [PUBMED Abstract]
- Northouse LL, Katapodi MC, Song L, et al.: Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA Cancer J Clin 60 (5): 317-39, 2010 Sep-Oct. [PUBMED Abstract]
- Griffin JM, Meis LA, MacDonald R, et al.: Effectiveness of family and caregiver interventions on patient outcomes in adults with cancer: a systematic review. J Gen Intern Med 29 (9): 1274-82, 2014. [PUBMED Abstract]
- Fu F, Zhao H, Tong F, et al.: A Systematic Review of Psychosocial Interventions to Cancer Caregivers. Front Psychol 8: 834, 2017. [PUBMED Abstract]
- Frambes D, Given B, Lehto R, et al.: Informal Caregivers of Cancer Patients: Review of Interventions, Care Activities, and Outcomes. West J Nurs Res 40 (7): 1069-1097, 2018. [PUBMED Abstract]
- Northouse L, Kershaw T, Mood D, et al.: Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psychooncology 14 (6): 478-91, 2005. [PUBMED Abstract]
- Northouse LL, Mood DW, Schafenacker A, et al.: Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology 22 (3): 555-63, 2013. [PUBMED Abstract]
- McMillan SC, Small BJ, Weitzner M, et al.: Impact of coping skills intervention with family caregivers of hospice patients with cancer: a randomized clinical trial. Cancer 106 (1): 214-22, 2006. [PUBMED Abstract]
- Meyers FJ, Carducci M, Loscalzo MJ, et al.: Effects of a problem-solving intervention (COPE) on quality of life for patients with advanced cancer on clinical trials and their caregivers: simultaneous care educational intervention (SCEI): linking palliation and clinical trials. J Palliat Med 14 (4): 465-73, 2011. [PUBMED Abstract]
- Dionne-Odom JN, Azuero A, Lyons KD, et al.: Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients With Advanced Cancer: Outcomes From the ENABLE III Randomized Controlled Trial. J Clin Oncol 33 (13): 1446-52, 2015. [PUBMED Abstract]
- DuBenske LL, Gustafson DH, Namkoong K, et al.: CHESS improves cancer caregivers' burden and mood: results of an eHealth RCT. Health Psychol 33 (10): 1261-72, 2014. [PUBMED Abstract]
- Ferrell BR, Grant M, Chan J, et al.: The impact of cancer pain education on family caregivers of elderly patients. Oncol Nurs Forum 22 (8): 1211-8, 1995. [PUBMED Abstract]
- Hudson P, Quinn K, Kristjanson L, et al.: Evaluation of a psycho-educational group programme for family caregivers in home-based palliative care. Palliat Med 22 (3): 270-80, 2008. [PUBMED Abstract]
- Derdiarian AK: Effects of information on recently diagnosed cancer patients' and spouses' satisfaction with care. Cancer Nurs 12 (5): 285-92, 1989. [PUBMED Abstract]
- Pasacreta JV, Barg F, Nuamah I, et al.: Participant characteristics before and 4 months after attendance at a family caregiver cancer education program. Cancer Nurs 23 (4): 295-303, 2000. [PUBMED Abstract]
- Grahn G, Danielson M: Coping with the cancer experience. II. Evaluating an education and support programme for cancer patients and their significant others. Eur J Cancer Care (Engl) 5 (3): 182-7, 1996. [PUBMED Abstract]
- Tsianakas V, Robert G, Richardson A, et al.: Enhancing the experience of carers in the chemotherapy outpatient setting: an exploratory randomised controlled trial to test impact, acceptability and feasibility of a complex intervention co-designed by carers and staff. Support Care Cancer 23 (10): 3069-80, 2015. [PUBMED Abstract]
- Valeberg BT, Kolstad E, Småstuen MC, et al.: The PRO-SELF pain control program improves family caregivers' knowledge of cancer pain management. Cancer Nurs 36 (6): 429-35, 2013 Nov-Dec. [PUBMED Abstract]
- Cartledge Hoff A, Haaga DA: Effects of an education program on radiation oncology patients and families. J Psychosoc Oncol 23 (4): 61-79, 2005. [PUBMED Abstract]
- Bultz BD, Speca M, Brasher PM, et al.: A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psychooncology 9 (4): 303-13, 2000 Jul-Aug. [PUBMED Abstract]
- Horowitz S, Passik SD, Malkin MG: “In sickness and in health”: a group intervention for spouses caring for patients with brain tumors. Journal of Psychosocial Oncology 14 (2): 43-56, 1996.
- Badr H, Smith CB, Goldstein NE, et al.: Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer 121 (1): 150-8, 2015. [PUBMED Abstract]
- Laudenslager ML, Simoneau TL, Kilbourn K, et al.: A randomized control trial of a psychosocial intervention for caregivers of allogeneic hematopoietic stem cell transplant patients: effects on distress. Bone Marrow Transplant 50 (8): 1110-8, 2015. [PUBMED Abstract]
- O'Hara RE, Hull JG, Lyons KD, et al.: Impact on caregiver burden of a patient-focused palliative care intervention for patients with advanced cancer. Palliat Support Care 8 (4): 395-404, 2010. [PUBMED Abstract]
- Perz J, Ussher JM; Australian Cancer and Sexuality Study Team: A randomized trial of a minimal intervention for sexual concerns after cancer: a comparison of self-help and professionally delivered modalities. BMC Cancer 15: 629, 2015. [PUBMED Abstract]
- Koehler M, Hoppe S, Kropf S, et al.: Randomized Trial of a Supportive Psychotherapy for Parents of Adolescents and Young Adults With Hematologic Malignancies. J Natl Compr Canc Netw 20 (13): , 2022. [PUBMED Abstract]
- Bevans M, Castro K, Prince P, et al.: An individualized dyadic problem-solving education intervention for patients and family caregivers during allogeneic hematopoietic stem cell transplantation: a feasibility study. Cancer Nurs 33 (2): E24-32, 2010 Mar-Apr. [PUBMED Abstract]
- Cameron JI, Shin JL, Williams D, et al.: A brief problem-solving intervention for family caregivers to individuals with advanced cancer. J Psychosom Res 57 (2): 137-43, 2004. [PUBMED Abstract]
- Nezu AM, Nezu CM, Felgoise SH, et al.: Project Genesis: assessing the efficacy of problem-solving therapy for distressed adult cancer patients. J Consult Clin Psychol 71 (6): 1036-48, 2003. [PUBMED Abstract]
- Sahler OJ, Varni JW, Fairclough DL, et al.: Problem-solving skills training for mothers of children with newly diagnosed cancer: a randomized trial. J Dev Behav Pediatr 23 (2): 77-86, 2002. [PUBMED Abstract]
- Demiris G, Parker Oliver D, Wittenberg-Lyles E, et al.: A noninferiority trial of a problem-solving intervention for hospice caregivers: in person versus videophone. J Palliat Med 15 (6): 653-60, 2012. [PUBMED Abstract]
- Bevans M, Wehrlen L, Castro K, et al.: A problem-solving education intervention in caregivers and patients during allogeneic hematopoietic stem cell transplantation. J Health Psychol 19 (5): 602-17, 2014. [PUBMED Abstract]
- Hendrix C, Tepfer S, Forest S, et al.: Transitional Care Partners: a hospital-to-home support for older adults and their caregivers. J Am Assoc Nurse Pract 25 (8): 407-14, 2013. [PUBMED Abstract]
- Kurtz ME, Kurtz JC, Given CW, et al.: A randomized, controlled trial of a patient/caregiver symptom control intervention: effects on depressive symptomatology of caregivers of cancer patients. J Pain Symptom Manage 30 (2): 112-22, 2005. [PUBMED Abstract]
- Hendrix CC, Bailey DE, Steinhauser KE, et al.: Effects of enhanced caregiver training program on cancer caregiver's self-efficacy, preparedness, and psychological well-being. Support Care Cancer 24 (1): 327-36, 2016. [PUBMED Abstract]
- Toseland RW, Blanchard CG, McCallion P: A problem solving intervention for caregivers of cancer patients. Soc Sci Med 40 (4): 517-28, 1995. [PUBMED Abstract]
- Milberg A, Rydstrand K, Helander L, et al.: Participants' experiences of a support group intervention for family members during ongoing palliative home care. J Palliat Care 21 (4): 277-84, 2005. [PUBMED Abstract]
- Kozachik SL, Given CW, Given BA, et al.: Improving depressive symptoms among caregivers of patients with cancer: results of a randomized clinical trial. Oncol Nurs Forum 28 (7): 1149-57, 2001. [PUBMED Abstract]
- Walsh K, Jones L, Tookman A, et al.: Reducing emotional distress in people caring for patients receiving specialist palliative care. Randomised trial. Br J Psychiatry 190: 142-7, 2007. [PUBMED Abstract]
- Baucom DH, Porter LS, Kirby JS, et al.: A couple-based intervention for female breast cancer. Psychooncology 18 (3): 276-83, 2009. [PUBMED Abstract]
- McLean LM, Jones JM, Rydall AC, et al.: A couples intervention for patients facing advanced cancer and their spouse caregivers: outcomes of a pilot study. Psychooncology 17 (11): 1152-6, 2008. [PUBMED Abstract]
- Stehl ML, Kazak AE, Alderfer MA, et al.: Conducting a randomized clinical trial of an psychological intervention for parents/caregivers of children with cancer shortly after diagnosis. J Pediatr Psychol 34 (8): 803-16, 2009. [PUBMED Abstract]
- Northouse LL, Mood DW, Schafenacker A, et al.: Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer 110 (12): 2809-18, 2007. [PUBMED Abstract]
- Kissane DW, McKenzie M, Bloch S, et al.: Family focused grief therapy: a randomized, controlled trial in palliative care and bereavement. Am J Psychiatry 163 (7): 1208-18, 2006. [PUBMED Abstract]
- Scott JL, Halford WK, Ward BG: United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol 72 (6): 1122-35, 2004. [PUBMED Abstract]
- Northouse L, Schafenacker A, Barr KL, et al.: A tailored Web-based psychoeducational intervention for cancer patients and their family caregivers. Cancer Nurs 37 (5): 321-30, 2014 Sep-Oct. [PUBMED Abstract]
- Carter PA: A brief behavioral sleep intervention for family caregivers of persons with cancer. Cancer Nurs 29 (2): 95-103, 2006 Mar-Apr. [PUBMED Abstract]
- Cohen M, Kuten A: Cognitive-behavior group intervention for relatives of cancer patients: a controlled study. J Psychosom Res 61 (2): 187-96, 2006. [PUBMED Abstract]
- Given B, Given CW, Sikorskii A, et al.: The impact of providing symptom management assistance on caregiver reaction: results of a randomized trial. J Pain Symptom Manage 32 (5): 433-43, 2006. [PUBMED Abstract]
- Keefe FJ, Ahles TA, Sutton L, et al.: Partner-guided cancer pain management at the end of life: a preliminary study. J Pain Symptom Manage 29 (3): 263-72, 2005. [PUBMED Abstract]
- Badger T, Segrin C, Dorros SM, et al.: Depression and anxiety in women with breast cancer and their partners. Nurs Res 56 (1): 44-53, 2007 Jan-Feb. [PUBMED Abstract]
- Badger TA, Segrin C, Hepworth JT, et al.: Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psychooncology 22 (5): 1035-42, 2013. [PUBMED Abstract]
- Badger T, Segrin C, Pasvogel A, et al.: The effect of psychosocial interventions delivered by telephone and videophone on quality of life in early-stage breast cancer survivors and their supportive partners. J Telemed Telecare 19 (5): 260-5, 2013. [PUBMED Abstract]
- Rexilius SJ, Mundt C, Erickson Megel M, et al.: Therapeutic effects of massage therapy and handling touch on caregivers of patients undergoing autologous hematopoietic stem cell transplant. Oncol Nurs Forum 29 (3): E35-44, 2002. [PUBMED Abstract]
- Winters-Stone KM, Lyons KS, Dobek J, et al.: Benefits of partnered strength training for prostate cancer survivors and spouses: results from a randomized controlled trial of the Exercising Together project. J Cancer Surviv 10 (4): 633-44, 2016. [PUBMED Abstract]
- van den Hurk DG, Schellekens MP, Molema J, et al.: Mindfulness-Based Stress Reduction for lung cancer patients and their partners: Results of a mixed methods pilot study. Palliat Med 29 (7): 652-60, 2015. [PUBMED Abstract]
- Lengacher CA, Kip KE, Barta M, et al.: A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs 30 (3): 170-85, 2012. [PUBMED Abstract]
Interventions for Caregivers During the Cancer Trajectory
Subspecialty Palliative Care
As previously described in this summary, the mental and physical health and coping of patients and caregivers are interdependent. Several trials of subspecialty palliative care interventions have specifically targeted and measured caregiver outcomes. For more information, see the sections on Secondary Appraisal: Resources for Informal Caregivers, The Needs of Caregivers During the Cancer Trajectory, and The Psychological Consequences of Caregiving.
- Educate, Nurture, Advise Before Life Ends (ENABLE): First developed for patients with advanced cancer,[1] in 2015 this intervention was expanded to include informal caregivers and improve selected outcomes. The ENABLE III intervention included three weekly structured telephone coaching sessions, monthly follow-up, and a bereavement call. It was delivered along with the COPE (Creativity, Optimism, Planning, Expert Information) problem-solving program. [2] It was tested in 122 informal caregivers, with 61 receiving early intervention and 61 receiving delayed intervention (3 months later). Informal caregivers who received early intervention had better outcomes than caregivers who received delayed intervention. These outcomes included lower depression scores at 3 months and lower depression and stress burden in terminal analyses of decedents’ caregivers.[3]
- Early integrated palliative care in advanced-stage lung and gastrointestinal cancer: Patients and caregivers randomly assigned to the intervention arm were scheduled to meet monthly with either a subspecialty palliative care physician or an advanced-practice provider.[4] One hundred thirty-seven caregivers were assigned to early palliative care and 138 to usual care. Caregivers were invited but not required to attend. The median number of visits attended by a caregiver (not necessarily the enrolled caregiver) was 10, with a range of 1 to 51. The Hospital Anxiety and Depression Scale was administered at weeks 12 and 24. Caregivers assigned to the palliative care arm had fewer symptoms of depression at 12 weeks but not at 24 weeks. There were no differences in anxiety scores.
- Early palliative care for patients with advanced cancer: Ninety-four caregivers were randomly assigned to the intervention, which included palliative care office visits (which were not mandatory for the caregiver) and nurse phone contact the week after each monthly visit. Home visits were available. The median number of visits attended was two, with a range of zero to eight; 85% of caregivers attended at least one visit. Caregivers in the palliative care arm were more satisfied with care than caregivers in the usual-care arm, but there was no improvement in caregiver quality of life (QOL).[5]
- Palliative care and hematopoietic stem cell transplant: A trial of the effect of inpatient subspecialty palliative care visits during hospitalization for stem cell transplant demonstrated that caregivers of intervention patients experienced a smaller increase in depression than caregivers of control patients. But there were no differences in QOL or anxiety.[6] The intervention did not specifically focus on caregivers. Instead, the focus was on the patient’s physical and psychological symptoms.
Palliative Care and End of Life
A systematic review highlighted the results of 14 studies of patients receiving end-of-life care. The review showed that cognitive behavioral therapy was conducted the most (n = 6) and demonstrated the most positive outcomes, including increased self-efficacy, improved psychological functioning, increased hope, and improved QOL across the various studies.[7]
References
- Bakitas M, Lyons KD, Hegel MT, et al.: Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 302 (7): 741-9, 2009. [PUBMED Abstract]
- McMillan SC, Small BJ, Weitzner M, et al.: Impact of coping skills intervention with family caregivers of hospice patients with cancer: a randomized clinical trial. Cancer 106 (1): 214-22, 2006. [PUBMED Abstract]
- Dionne-Odom JN, Azuero A, Lyons KD, et al.: Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients With Advanced Cancer: Outcomes From the ENABLE III Randomized Controlled Trial. J Clin Oncol 33 (13): 1446-52, 2015. [PUBMED Abstract]
- El-Jawahri A, Greer JA, Pirl WF, et al.: Effects of Early Integrated Palliative Care on Caregivers of Patients with Lung and Gastrointestinal Cancer: A Randomized Clinical Trial. Oncologist 22 (12): 1528-1534, 2017. [PUBMED Abstract]
- McDonald J, Swami N, Hannon B, et al.: Impact of early palliative care on caregivers of patients with advanced cancer: cluster randomised trial. Ann Oncol 28 (1): 163-168, 2017. [PUBMED Abstract]
- El-Jawahri A, LeBlanc T, VanDusen H, et al.: Effect of Inpatient Palliative Care on Quality of Life 2 Weeks After Hematopoietic Stem Cell Transplantation: A Randomized Clinical Trial. JAMA 316 (20): 2094-2103, 2016. [PUBMED Abstract]
- Chi NC, Demiris G, Lewis FM, et al.: Behavioral and Educational Interventions to Support Family Caregivers in End-of-Life Care: A Systematic Review. Am J Hosp Palliat Care 33 (9): 894-908, 2016. [PUBMED Abstract]
Parents as Caregivers
The diagnosis of childhood cancer represents the start of a period of substantial distress for parents. These parents report shock, emotional pain, difficulty coping with the necessary procedures performed on their child, rumination, and high levels of information seeking accompanied by a sense of lack of control.[1-3] One study evaluated 119 mothers and 52 fathers of children undergoing cancer treatment. The study found that all but one participant reported traumatic stress symptoms such as intrusive thoughts, physiological arousal, and avoidance.[4] In another study, parents of children undergoing treatment (n = 175) were compared with parents of children who had completed treatment (n = 238). Parents reported symptoms of traumatic stress (such as intrusion and arousal) more frequently during the acute phase of treatment than after treatment. Certain demographic factors may play a role in the degree to which parents experience significant stress that impairs function. Mothers were more likely than fathers to report higher levels of stress, and parents with fewer years of formal education and lower socioeconomic status were more likely to experience traumatic stress at any time.[5]
Patterns of parental stress in families of children treated for cancer differ from those in families of children treated for other diseases. In one large study of 675 parents, parents of children with cancer reported significantly higher levels of distress—as indicated by anxiety, physical and psychological distress, depression, and loneliness—than did parents of children with diabetes. Distress levels of the two groups of parents matched in measures of uncertainty, loss of control, self-esteem, disease-related fear, and sleep disturbances. Distress levels for parents of children with cancer decreased in intensity with longer time since diagnosis.[6]
At the same time they are dealing with increased distress, parents of children with cancer report wanting to remain strong and optimistic for their children.[7] One study found no differences in multiple measures of family distress and psychological functioning between families of children with cancer and families with healthy children.[8]
Several factors appear to predict long-term parental adjustment. Better short- and long-term adjustment is experienced by parents who:[9-11]
- Are employed.
- Have social support from family, friends, and health care team members.
- Experience lower levels of parenting stress.
- View their children’s quality of life positively.
- Have positive expectations for treatment outcome.
Factors associated with poorer parental adjustment include:[12,13]
- Low parental expectations for positive outcomes.
- Feelings of helplessness, uncertainty, and anxiety.
- Low levels of social support.
- Negative interactions with health care team members.
- Negative assessment of the child’s quality of life.
Race [14] and parent gender [15] may affect the intensity of the effect of these factors on parental functioning. In rare circumstances, the stress of coping with pain, adverse side effects, lack of control or understanding of information or outcomes, and conflicts with health care professionals may lead parents to drop out of cancer treatment for their children.[16]
Most studies suggest that over time, maternal affective distress and perceived stress decline, but the perceived burden of caring for a child with cancer remains stable, as do positive characteristics such as parental control, nurturance, and responsiveness.[14] This pattern may be related to the high levels of social support provided at the time of diagnosis. Over all phases of cancer treatment, the level of support gradually declines, while the perceived quality of support remains stable.[15] In general, parents are seen as resilient,[12][Level of evidence: II] but parental loneliness and continued uncertainty may last far beyond the treatment phase if there are ongoing late effects of treatment for the child.[17][Level of evidence: II] A few studies have found that a substantial number of parents (30%–36%) of long-term cancer survivors may experience intense, long-term, stress-related symptoms that fall below the threshold for a diagnosis of post-traumatic stress disorder (PTSD) but that are nevertheless a significant problem for these parents.[18,19][Level of evidence: II] Symptoms were severe enough that in 20% of families, at least one parent met the criteria for a diagnosis of PTSD.[19]
References
- McGrath P: Treatment for childhood acute lymphoblastic leukaemia: the fathers' perspective. Aust Health Rev 24 (2): 135-42, 2001. [PUBMED Abstract]
- Levi RB, Marsick R, Drotar D, et al.: Diagnosis, disclosure, and informed consent: learning from parents of children with cancer. J Pediatr Hematol Oncol 22 (1): 3-12, 2000 Jan-Feb. [PUBMED Abstract]
- Goldbeck L: Parental coping with the diagnosis of childhood cancer: gender effects, dissimilarity within couples, and quality of life. Psychooncology 10 (4): 325-35, 2001 Jul-Aug. [PUBMED Abstract]
- Kazak AE, Boeving CA, Alderfer MA, et al.: Posttraumatic stress symptoms during treatment in parents of children with cancer. J Clin Oncol 23 (30): 7405-10, 2005. [PUBMED Abstract]
- Norberg AL, Lindblad F, Boman KK: Parental traumatic stress during and after paediatric cancer treatment. Acta Oncol 44 (4): 382-8, 2005. [PUBMED Abstract]
- Boman KK, Viksten J, Kogner P, et al.: Serious illness in childhood: the different threats of cancer and diabetes from a parent perspective. J Pediatr 145 (3): 373-9, 2004. [PUBMED Abstract]
- Young B, Dixon-Woods M, Windridge KC, et al.: Managing communication with young people who have a potentially life threatening chronic illness: qualitative study of patients and parents. BMJ 326 (7384): 305, 2003. [PUBMED Abstract]
- Noll RB, Gartstein MA, Hawkins A, et al.: Comparing parental distress for families with children who have cancer and matched comparison families without children with cancer. Fam Syst Med 13 (1): 11-27, 1995.
- Rourke MT, Stuber ML, Hobbie WL, et al.: Posttraumatic stress disorder: understanding the psychosocial impact of surviving childhood cancer into young adulthood. J Pediatr Oncol Nurs 16 (3): 126-35, 1999. [PUBMED Abstract]
- Kazak AE, Barakat LP: Brief report: parenting stress and quality of life during treatment for childhood leukemia predicts child and parent adjustment after treatment ends. J Pediatr Psychol 22 (5): 749-58, 1997. [PUBMED Abstract]
- Grootenhuis MA, Last BF: Predictors of parental emotional adjustment to childhood cancer. Psychooncology 6 (2): 115-28, 1997. [PUBMED Abstract]
- Dockerty JD, Williams SM, McGee R, et al.: Impact of childhood cancer on the mental health of parents. Med Pediatr Oncol 35 (5): 475-83, 2000. [PUBMED Abstract]
- Santacroce S: Uncertainty, anxiety, and symptoms of posttraumatic stress in parents of children recently diagnosed with cancer. J Pediatr Oncol Nurs 19 (3): 104-11, 2002 May-Jun. [PUBMED Abstract]
- Steele RG, Long A, Reddy KA, et al.: Changes in maternal distress and child-rearing strategies across treatment for pediatric cancer. J Pediatr Psychol 28 (7): 447-52, 2003 Oct-Nov. [PUBMED Abstract]
- Hoekstra-Weebers JE, Jaspers JP, Kamps WA, et al.: Psychological adaptation and social support of parents of pediatric cancer patients: a prospective longitudinal study. J Pediatr Psychol 26 (4): 225-35, 2001. [PUBMED Abstract]
- Yeh CH, Lin CF, Tsai JL, et al.: Determinants of parental decisions on 'drop out' from cancer treatment for childhood cancer patients. J Adv Nurs 30 (1): 193-9, 1999. [PUBMED Abstract]
- Van Dongen-Melman JE, Pruyn JF, De Groot A, et al.: Late psychosocial consequences for parents of children who survived cancer. J Pediatr Psychol 20 (5): 567-86, 1995. [PUBMED Abstract]
- Brown RT, Madan-Swain A, Lambert R: Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. J Trauma Stress 16 (4): 309-18, 2003. [PUBMED Abstract]
- Kazak AE, Alderfer M, Rourke MT, et al.: Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol 29 (3): 211-9, 2004 Apr-May. [PUBMED Abstract]
Latest Updates to This Summary (05/06/2025)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Editorial changes were made to this summary.
This summary is written and maintained by the PDQ Supportive and Palliative Care Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about challenges and helpful interventions for caregivers of cancer patients. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Supportive and Palliative Care Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Informal Caregivers in Cancer are:
- Larry D. Cripe, MD (Indiana University School of Medicine)
- Edward B. Perry, MD (VA Connecticut Healthcare System)
- Maria Petzel, RD, CSO, LD, CNSC, FAND (University of TX MD Anderson Cancer Center)
- Rachel A. Pozzar, PhD, RN (Dana-Farber Cancer Institute)
- Diane Von Ah, PhD, RN, FAAN (The Ohio State University)
- Amy Wachholtz, PhD, MDiv, MS, ABPP (University of Colorado)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Supportive and Palliative Care Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Supportive and Palliative Care Editorial Board. PDQ Informal Caregivers in Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/about-cancer/coping/family-friends/family-caregivers-hp-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389284]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
The information in these summaries should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.