Colorectal Cancer Prevention (PDQ®)–Patient Version
What Is Prevention?
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
To prevent new cancers from starting, scientists look at risk factors and protective factors. Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk, but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied, including:
- changing lifestyle or eating habits
- avoiding things known to cause cancer
- taking medicines to treat a precancerous condition or to keep cancer from starting
General Information About Colorectal Cancer
Key Points
- Colorectal cancer is a disease in which malignant (cancer) cells form in the tissues of the colon or the rectum.
- Colorectal cancer is the second leading cause of death from cancer in the United States.
Colorectal cancer is a disease in which malignant (cancer) cells form in the tissues of the colon or the rectum.
The colon is part of the body's digestive system. The digestive system removes and
processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and
water) from foods and helps pass waste material out of the body. The digestive
system is made up of the mouth, throat, esophagus,
stomach, and the
small and large intestines. The colon (large bowel) is the first part of the large intestine and is about 5 feet long. Together, the rectum and anal canal make up the last part of the large intestine and are 6 to 8 inches long. The anal canal ends at the
anus (the opening of the large intestine to
the outside of the body). 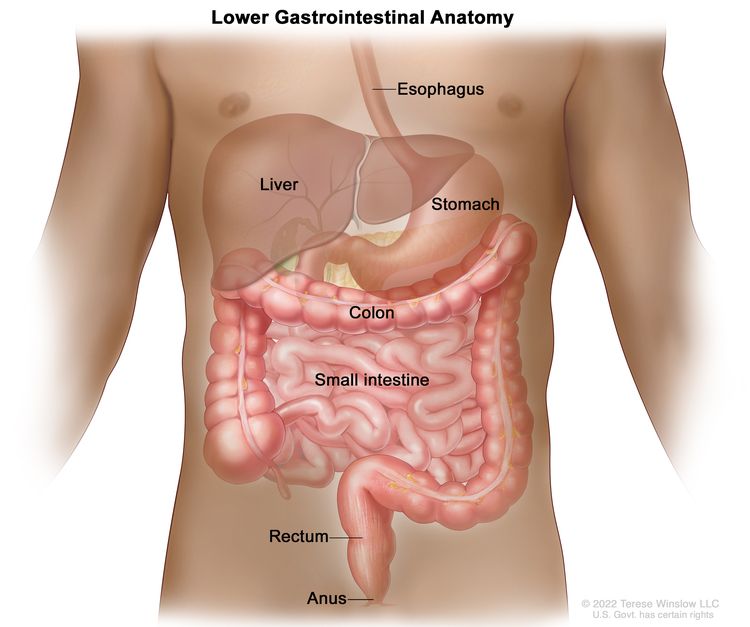
Cancer that begins in the colon is called colon cancer, and cancer that begins in the rectum is called rectal cancer. Cancer that affects either of these organs may also be called colorectal cancer.
Other PDQ summaries containing information related to colorectal cancer include:
- Colorectal Cancer Screening
- Colon Cancer Treatment
- Rectal Cancer Treatment
- Genetics of Colorectal Cancer (written for health professionals)
Colorectal cancer is the second leading cause of death from cancer in the United States.
Colorectal cancer is the third most common cancer worldwide and the second leading cause of cancer death in the United States when numbers for men and women are combined. Between 2012 and 2021, the number of new colorectal cancer cases in the United States decreased. This decline was largely driven by falling rates in adults aged 65 and older, who continue to have the highest overall rates of colorectal cancer. The drop in older adults may be due in part to increased colorectal cancer screening, which can detect and remove precancerous growths before they develop into cancer. However, trends vary by age group. Among adults younger than 50, the number of new cases of colorectal cancer rose by about 2.4% per year, the largest increase among all age groups. In people aged 50 to 64, the number of new cases increased slightly per year.
Since 1970, the death rate from colorectal cancer has declined in men and women. However, new cases and deaths from colorectal cancer remain higher among Black people than other racial groups. Studies show that Black people are not more likely than others to have precancerous growths.
Finding and treating colorectal cancer early may prevent death from colorectal cancer. Screening tests may be used to help find colorectal cancer.
Colorectal Cancer Prevention
Key Points
- Avoiding risk factors and increasing protective factors may help prevent cancer.
- The following risk factors increase the risk of colorectal cancer:
- Age
- Family history of colorectal cancer
- Personal history
- Inherited risk
- Alcohol
- Cigarette smoking
- Race
- Obesity
- The following protective factors decrease the risk of colorectal cancer:
- Physical activity
- Aspirin
- Combination hormone replacement therapy
- Polyp removal
- It is not clear if the following affect the risk of colorectal cancer:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) other than aspirin
- Calcium
- Diet
- The following factors do not affect the risk of colorectal cancer:
- Hormone replacement therapy with estrogen only
- Statins
- Cancer prevention clinical trials are used to study ways to prevent cancer.
- New ways to prevent colorectal cancer are being studied in clinical trials.
Avoiding risk factors and increasing protective factors may help prevent cancer.
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight, and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
The following risk factors increase the risk of colorectal cancer:
Age
The risk of colorectal cancer increases after age 50. Most cases of colorectal cancer are diagnosed after age 50.
Family history of colorectal cancer
Having a parent, brother, sister, or child with colorectal cancer doubles a person's risk of colorectal cancer.
Personal history
Having a personal history of the following conditions increases the risk of colorectal cancer:
- previous colorectal cancer
- high-risk adenomas (colorectal polyps that are 1 centimeter or larger in size or that have cells that look abnormal under a microscope)
- ovarian cancer
- inflammatory bowel disease (such as ulcerative colitis or Crohn disease)
Inherited risk
The risk of colorectal cancer is increased when certain gene changes linked to familial adenomatous polyposis (FAP) or hereditary nonpolyposis colon cancer (HNPCC or Lynch Syndrome) are inherited.
Alcohol
Drinking 3 or more alcoholic beverages per day increases the risk of colorectal cancer. Drinking alcohol is also linked to the risk of forming large colorectal adenomas (benign tumors).
Cigarette smoking
Cigarette smoking is linked to an increased risk of colorectal cancer and death from colorectal cancer.
Smoking cigarettes is also linked to an increased risk of forming colorectal adenomas. Cigarette smokers who have had surgery to remove colorectal adenomas are at an increased risk for the adenomas to recur (come back).
Race
Black individuals have an increased risk of colorectal cancer and death from colorectal cancer compared to other races.
Obesity
Obesity is linked to an increased risk of colorectal cancer and death from colorectal cancer.
The following protective factors decrease the risk of colorectal cancer:
Physical activity
A lifestyle that includes regular physical activity is linked to a decreased risk of colorectal cancer.
Aspirin
Studies have shown that taking aspirin daily for at least two years lowers the risk of colorectal cancer and the risk of death from colorectal cancer. The decrease in risk begins 10 to 20 years after patients start taking aspirin.
The possible harms of aspirin use (100 mg or less) daily or every other day include an increased risk of stroke and bleeding in the stomach and intestines. These risks may be greater among the elderly, men, and those with conditions linked to a higher-than-normal risk of bleeding.
Combination hormone replacement therapy
Studies have shown that combination hormone replacement therapy (HRT) that includes both estrogen and progestin lowers the risk of invasive colorectal cancer in postmenopausal women.
However, in women who take combination HRT and do develop colorectal cancer, the cancer is more likely to be advanced when it is diagnosed and the risk of dying from colorectal cancer is not decreased.
The possible harms of combination HRT include an increased risk of:
- breast cancer
- heart disease
- blood clots
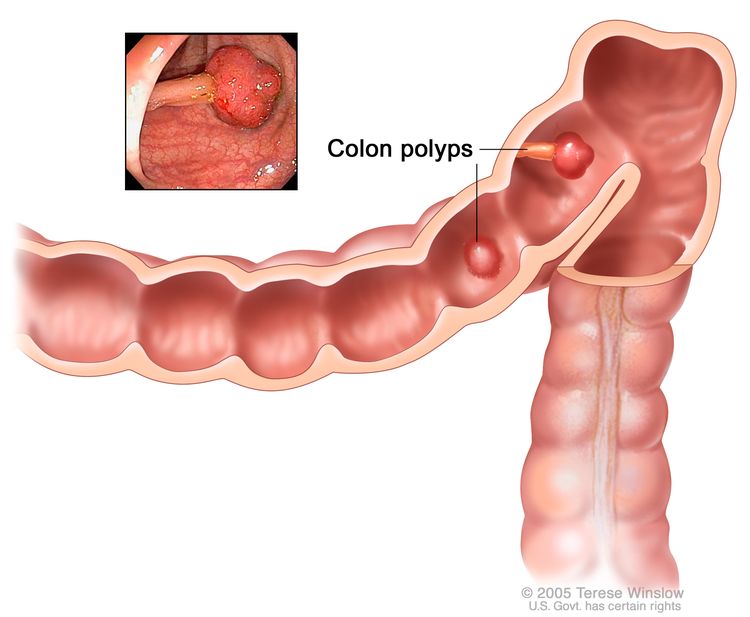
Polyp removal
Most colorectal polyps are adenomas, which may develop into cancer. Removing colorectal polyps that are larger than 1 centimeter (pea-sized) may lower the risk of colorectal cancer. It is not known if removing smaller polyps lowers the risk of colorectal cancer.
The possible harms of polyp removal during colonoscopy or sigmoidoscopy include a tear in the wall of the colon and bleeding.
It is not clear if the following affect the risk of colorectal cancer:
Nonsteroidal anti-inflammatory drugs (NSAIDs) other than aspirin
It is not known if the use of nonsteroidal anti-inflammatory drugs or NSAIDs (such as sulindac, celecoxib, naproxen, and ibuprofen) lowers the risk of colorectal cancer.
Studies have shown that taking the nonsteroidal anti-inflammatory drug celecoxib reduces the risk of colorectal adenomas (benign tumors) coming back after they have been removed. It is not clear if this results in a lower risk of colorectal cancer.
Taking sulindac or celecoxib has been shown to reduce the number and size of polyps that form in the colon and rectum of people with familial adenomatous polyposis (FAP). It is not clear if this results in a lower risk of colorectal cancer.
The possible harms of NSAIDs include:
- kidney problems
- bleeding in the stomach, intestines, or brain
- heart problems such as heart attack and congestive heart failure
Calcium
It is not known if taking calcium supplements lowers the risk of colorectal cancer.
Diet
It is not known if a diet low in fat and meat and high in fiber, fruits, and vegetables lowers the risk of colorectal cancer.
Some studies have shown that a diet high in fat, proteins, calories, and meat increases the risk of colorectal cancer, but other studies have not.
The following factors do not affect the risk of colorectal cancer:
Hormone replacement therapy with estrogen only
Hormone replacement therapy with estrogen only does not lower the risk of having invasive colorectal cancer or the risk of dying from colorectal cancer.
Statins
Studies have shown that taking statins (drugs that lower cholesterol) does not increase or decrease the risk of colorectal cancer.
Cancer prevention clinical trials are used to study ways to prevent cancer.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials include healthy people who may or may not have an increased risk of cancer. Other prevention trials include people who have had cancer and are trying to prevent recurrence or a second cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines, vitamins, minerals, or food supplements.
New ways to prevent colorectal cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about colorectal cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Colorectal Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/colorectal/patient/colorectal-prevention-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389376]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.