Challenging Experiences in Expanding Opportunities: The Burkitt Lymphoma Genome Sequencing Project in Brazil
, by Stella Maris Pereira Sobrinho Rodrigues, Ana Raquel Viana de Godoy, and Jeffrey M. Bethony
Burkitt Lymphoma (BL) is an aggressive B-cell lymphoma involving dysregulation of the MYC oncogene by chromosomal translocations. It is most common in children but also affects adults and occurs in sporadic, endemic, and HIV-associated forms. The Epstein-Barr virus-associated BL (eBL) endemic subtype is the most common pediatric cancer in equatorial Africa but also occurs in other parts of the world (e.g. the rainforest of Brazil).
The National Cancer Institute (NCI) established a collaboration with the Foundation for Burkitt Lymphoma Research to develop a genomic databank for BL. One goal of the Burkitt Lymphoma Genome Sequencing Project (BLGSP) is to conduct comprehensive molecular characterization of BL by sequencing DNA and RNA from a large BL cohort–including endemic, HIV-associated, sporadic, pediatric, and adult cases–in order to define the genetic and phenotypic features that drive these cancers. These data will be analyzed and published; the goals are to develop new therapeutic strategies that can be deployed worldwide.
BL in Brazil is characterized by geographically distinct clinical and pathologic features1. In central and southern Brazil, adult BL cases occur with similar diagnosis as in the United States and western Europe. In the northeastern and Amazonian regions of Brazil, eBL-associated infections overlap with either Plasmodium falciparum or Plasmodium vivax malaria similar to cases in equatorial Africa. Intensive chemotherapy is effective, but the associated toxicity requires supportive care that is not readily available in resource-poor regions.
Clinical Research in Brazil: The Ethical Approval for the BLGSP was Among the First to Use a New Federal Regulation Process
NCI’s Office of Cancer Genomics (OCG) identified, after extensive search, the Hospital das Clinicas da Universidade Federal de Minas Gerais (HdC-UFMG) as a potential tissue source site in Brazil and became a member of the project working group (WG). The regulatory process was initiated in November 2013, and all necessary documents (e.g. protocol, informed consent form, etc.) were submitted to the local Institutional Review Board (IRB). Ethical approval was obtained in March 2014; however, the challenge arose because the BLGSP is an internationally-sponsored project involving sample storage and shipping outside of Brazil, and a national IRB approval for biobanking and biorepository (CONEP) was requested. This was a newly developed process, and therefore required extensive (two year) to- and from- exchange to ensure that all required materials were provided in the right format. The approval was obtained in July 2016.
Brazil BLGSP Tissue Source Sites (TSS)
Once we had the approval in hand, Dr. Frederico Melo (a pathologist), the principal investigator (PI), and staff evaluated the availability of cases at the HdC-UFMG in the spring of 2017. It was decided that to ensure the accrual of the promised number of cases, a partnership with the Instituto Nacional do Cancer (INCA), with PI Dr. Fabio Leal, was established.
Standard Operating Procedures (SOPs)
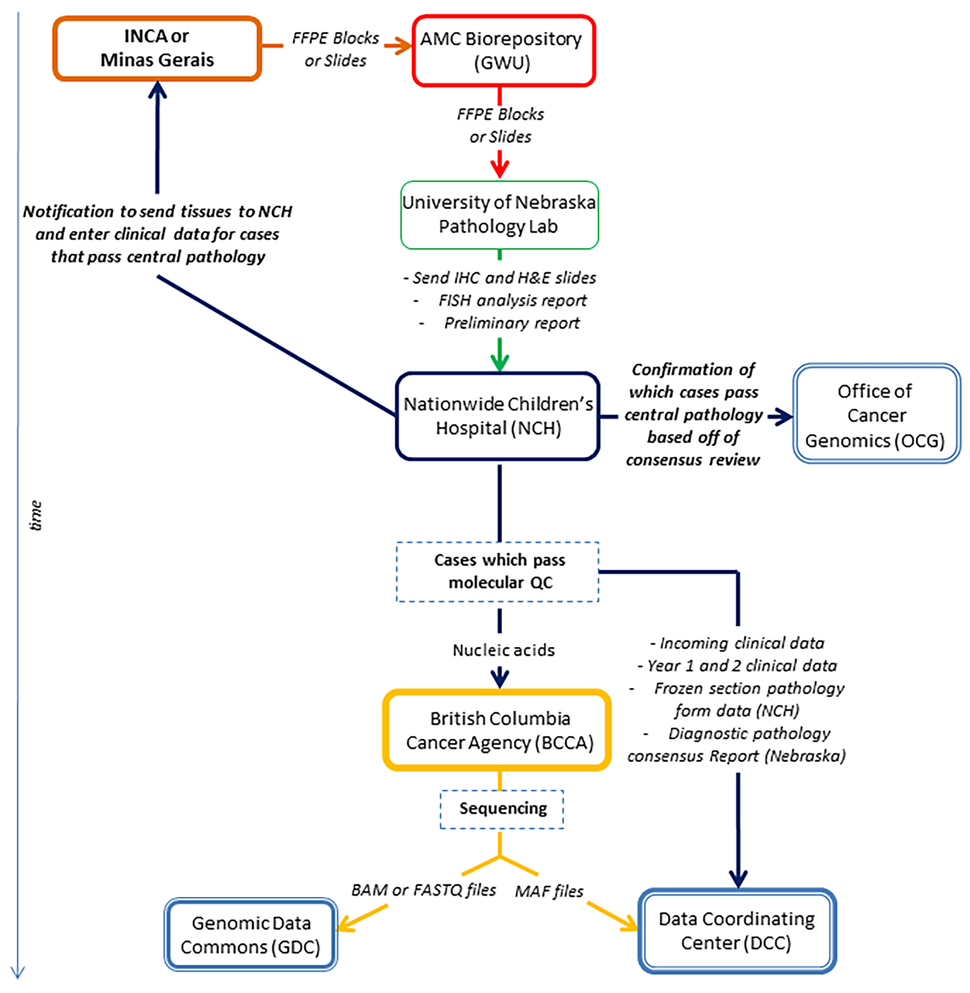
The BLGSP utilizes SOPs to enhance the ability to integrate results for tissues obtained across multiple collection sites. The TSS are required to collect and store the tissues, perform site-capable pathology analysis to determine the BL diagnosis, and provide the BLGSP-required clinical data. Based on the SOPs, an overview flowchart was developed by the TSS coordinator in Brazil to understand the process. A challenge for the TSS in Brazil was to develop mechanisms and strategies to identify retrospective samples which was successfully overcome at both sites. Below we describe what was done at HdC-UFMG.
The BL case biobank of retrospective samples is located at the Anatomy and Pathology Unit at UFMG. The Unit has a large bank of samples and diagnostic reports for patients diagnosed from 2005 to 2017. The PI and staff first developed preliminary inclusion criteria to be: (i) patients diagnosed with BL confirmed through laboratory results (i.e. histopathological and immunochemistry exams); (ii) patients with “possible BL” (i.e. B-cell lymphoma in germinal center where turnover cells Ki67 >95% are searched); and (iii) patients with other types of lymphoma (e.g. B-cell with low turnover, T-cell, gray zone, anaplastic large cell, mucosa-associated lymphoid tissue, mantle cell).
The identification process starts with reading the clinical reports, selecting the patients with a positive diagnosis for lymphoma, and identifying the sample in the biobank. Clinical report forms for each case are available as paper copies, and cases which match the inclusion criteria are selected. Then, the patient ID code, formalin-fixed paraffin-embedded (FFPE) tissue block number, and the slice number are recorded. This information is vital to facilitate initial contact with the patient and obtain informed consent to get permission to use their tumor and normal samples in the study. Finally, the samples, which were selected by the Anatomy and Pathology Unit staff, are confirmed to match the BLGSP SOPs by the PI.
To date at both sites, 26 cases of BL in Brazil have been submitted to BLGSP, of which seven cases have both tumor and germline paired-samples. Currently, eight cases have passed diagnostic pathology review, three did not pass, and 15 are still being analyzed.
Next Steps
Challenges of the Brazil TSS have been the identification of prospective BL cases, which require logistical steps and complex operational procedures carried out by clinical staff and a study team involved at the hospital. The TSS have now improved the identification process for the retrospective BL cases from the past 12 years through expanding the search of diagnostic reports and FFPE blocks stored in the Anatomy and Pathology Unit at HdC-UFMG. The TSS are learning about the technical issues with molecular characterization data, and they can continue to use what they have learned today, from identifying the retrospective cases, to improve the collection process of prospective BL cases. Additionally, young investigators in the research community will use the molecular characterization data from BL patients identified through BLGSP to better understand the molecular alterations of BL in Brazil. This breakthrough has steered the TSS teams to improve the operational procedures in Brazil that have led to the current success of the BLGSP.
References
- Queiroga EM, Gualco G, Weiss LM, Dittmer DP, Araujo I, Klumb CEN, Harrington Jr WJ, Bacchi CE. Burkitt lymphoma in Brazil is characterized by geographically distinct clinicopathologic features. American Journal of Clinical Pathology. 2008 Dec;130(6):946-956. (PMID: 19019773)