How Studying the Natural History of Rare Cancers Improves Care
, by Brittany Cordeiro, NCI-CONNECT Program Manager
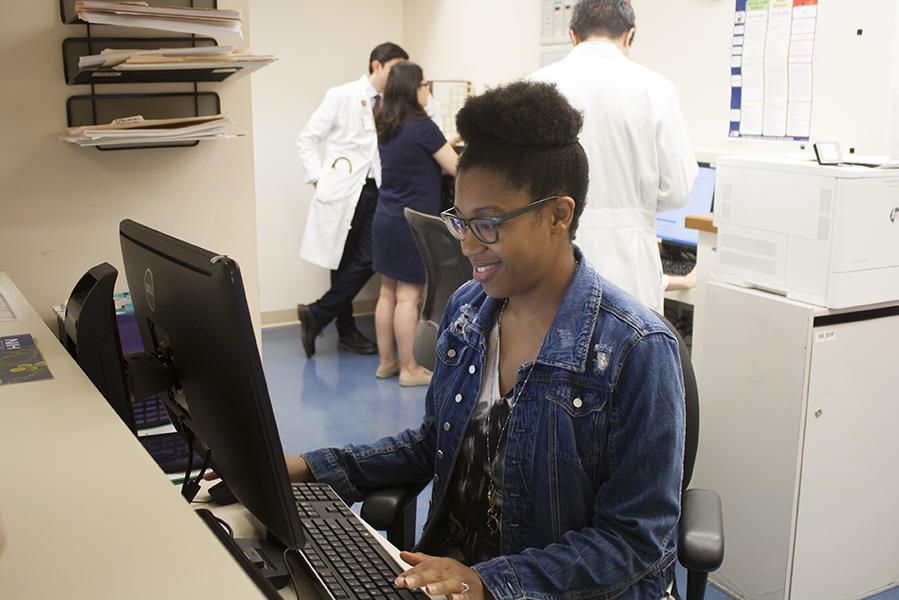
Research Nurse Sonja Crandon shares her work, the goals of the Natural History Study, and how it could reveal new areas of research while helping people with brain and spine tumors.
After watching her aunt battle leukemia, Sonja Crandon knew she wanted to help people with cancer. She became a registered nurse in 2001, but ultimately it was her intrigue in the disease process that led her to be a research nurse at NIH. There, she helped to launch a study that follows patients with primary central nervous system (CNS) tumors through the disease trajectory to describe the natural history of the disease.
The study aims to understand why people develop tumors, their experience living with these tumors, and how health care providers can help make the experience better. The study is not a treatment trial, but it connects patients with doctors who can help them manage their disease and provide treatment options. It also gathers information from the patient on their experience with the disease through the use of patient-reported outcomes.
“The study is focused on gathering information from people whether they are newly diagnosed or long-term survivors. This information is what helps us learn about brain and spine tumors and make new discoveries for future research,” says Crandon, a research nurse specialist in the NCI Center for Cancer Research's Neuro-Oncology Branch.
Crandon received her Bachelor of Science in nursing from Coppin State University in Baltimore, Maryland. After graduating, she interned at NIH as a medical surgery nurse. In 2007, she joined the Developmental Therapeutics Branch at NIH as a research nurse. In 2011, she left for an outside oncology group and returned to NIH in 2015 to work in the Pediatric Oncology Branch.
“My love for research—being able to carefully study a problem from different perspectives and find a solution—brought me back to NIH again as a research nurse,” Crandon shares. While in pediatrics, Crandon started collaborating with the neuro-oncology team to develop the Natural History Study. Shortly after the study launched, Crandon officially moved to the Neuro-Oncology Branch in 2016.
Much of the success of the Natural History Study can be attributed to Crandon. She not only serves to help patients understand the study and how to participate in it, but also coordinates all aspects of the study to ensure it runs efficiently and captures meaningful data. There are a remarkable 830 patients enrolled on the study to date.
What the Study Involves
Crandon works directly with the neuro-oncology patient care coordinators to identify the people with brain and spine tumors who are eligible for the Natural History Study prior to their first visit to NIH.
Doctors must refer patients to NIH for evaluation or a second opinion. The patient care coordinators gather the necessary information and documentation from these outside care providers. This includes basic personal and medical information and history of disease. Crandon reviews the information and then reaches out to the patient.
“I usually schedule about 10 minutes to talk with the patient over the phone. I briefly explain how NIH works, the basics of the study, and then go through the study consent process,” Crandon explains. It is important for people with brain and spine tumors to understand that the study is not a treatment trial, but it follows them from the moment they enroll onward through any treatments and survivorship.
The first component of the study is requesting that the patient send a tumor tissue sample for testing. The tissue is a critical element to confirm the person has a diagnosis of a rare brain or spine tumor. An NIH neuropathologist conducts additional molecular testing to determine if there's a clinical trial the person can participate in.
A patient would then be scheduled for an appointment at the NCI-CONNECT Clinic in the NIH Clinical Center. The appointment is an evaluation or baseline visit that includes physical and neurological exams, blood tests, and scans. Prior to that visit, the patient is asked to complete a series of patient-reported outcome (PRO) questionnaires to describe their symptoms, mood, general health status, and perceived cognitive symptoms. This information is reviewed by the doctor and is used along with the evaluation of the tumor and clinical exam to make recommendations related to treatment and clinical care. These are also completed at subsequent visits or remotely at least once a year, to understand the impact of the disease and treatment on how the person feels and functions.
Another questionnaire is about health and symptoms and is referred to as the Outcomes and Risk Assessment. “The questionnaire assesses quality of life and personal cancer risk based on early childhood experiences to the present moment, including diagnosis and treatment history,” Crandon says. The questionnaire is completed only once with the goal to understand why patients may be at risk for particular primary brain and spine tumors.
While the study aims to learn more about brain and spine tumors to further research, it also connects patients to doctors with experience treating brain and spine tumors.
We have a knowledgeable health care team that works very collaboratively with referring doctors. For instance, we can share molecular data that help provide insight—which helps guide potential treatment options.
Future Impact
What Crandon enjoys most about being a research nurse—next to problem-solving and collecting important information to advance our knowledge of these tumors—is getting to know patients. “I get to interact with patients to help support them and ease any anxiety they are feeling about the study. Sometimes it takes a lot of conversation and smiles,” Crandon says.
She adds that she encourages patients to ask questions and be candid. The information patients share is essential to help researchers understand risk factors and disease development. “We have to study the people that have these brain and spine tumors to develop solutions,” Crandon says. “Patient participation is the key, and we are grateful for their selflessness to help future patients and treatment advances.”