Symposium to Advance Neuro-Oncology Survivorship Care
, by Kristin Odom, NCI-CONNECT Communications Editor
Neuro-oncology providers, researchers, advocates, patients, and care partners gathered virtually to learn and discuss the challenges experienced by people living with brain and spine tumors and develop survivorship care guidelines.
People living with brain and spine tumors and their care partners face unique challenges. To increase awareness about these challenges and better understand their experiences as cancer survivors, neuro-oncology health care providers, researchers, patient advocates, patients and care partners met virtually on June 20-21, 2021, at the NCI-CONNECT Survivorship Care in Neuro-Oncology Symposium.
The symposium included speakers and attendees from various disciplines. Their goal was to define survivorship, recognize funding and research needs, navigate survivorship care, deliver quality care, and understand survivorship in neuro-oncology.
“The symposium provided a forum for thoughtful discussion of challenges and possible solutions in survivorship, with the intent to develop guidelines that will inform survivorship clinical care and research in brain and spine tumors,” says Heather Leeper, M.D., symposium co-chair alongside Terri Armstrong, Ph.D., deputy chief of the NCI Center for Cancer Research's Neuro-Oncology Branch (NOB), and Mark Gilbert, M.D., NOB chief.
Survivorship Care and Research Challenges and Solutions
The symposium started with a special message from NCI neuro-oncology health care professionals and NCI-CONNECT advocacy partners. They highlighted how everyone’s journey is unique and so is survivorship. They are working together to plant hope for the brain and spine tumor community.
After Drs. Armstrong and Leeper shared the goals of the symposium, Drs. Gilbert and Armstrong presented on the NCI-CONNECT program, which aims to improve care and treatments for people living with rare central nervous system tumors. Notably, NCI-CONNECT has three new remote observational survivorship clinical studies to better understand the patient experience and improve care.
Patient and caregiver experiences were an impactful component to the symposium. Ken, a 17-year rare cancer survivor, shared that, at age 32, he was diagnosed with medulloblastoma while serving as a lawyer in the United States Navy. He subsequently had surgery, chemotherapy, and radiation, and endures long-term effects, such as not being able to drive and having speech impairments. Barbara shared her experience caring for her husband who was diagnosed with glioblastoma in 2014 and passed away in December 2020. He had standard of care treatment at NIH and was stable for three-and-a-half years. He then had a recurrence, surgery, and participated in a clinical trial.
Emily Tonorezos, M.D., the director of the NCI Office of Cancer Survivorship (OCS), started the educational lectures by defining survivorship. She emphasized that a person is considered a cancer survivor from the time of their diagnosis through the balance of his or her life. Survivors can be those living with cancer and those free of cancer. She provided information about funded studies in neuro-oncology survivorship to address patient and caregiver needs. Dr. Tonorezos shared the services OCS provides, including supporting survivorship research to examine and address the physical, psychological, social, and economic effects of cancer and its treatment.
Dr. Leeper then spoke about navigating survivorship in neuro-oncology and the importance of patient-centered care—focusing on the patient and their experience rather than their disease. Patient-centered care can help manage symptoms such as pain, depression, and anxiety, and fosters discussions about prognosis, treatment goals, suffering, and advance directive.
Deborah Mayer, Ph.D., advanced practice oncology nurse and director of cancer survivorship at The University of North Carolina at Chapel Hill, described the gaps in long-term survivorship research and how the lives of brain tumor patients and their loves ones are disrupted. They navigate the new reality of life and compensate by adjusting goals and expectations, educating friends and family, accepting support from others, and socially reintegrating throughout their journey of living with a brain tumor.
“This helps patients, and their loved ones pick up the pieces of their lives and put their lives back together again in whatever new way works the best for them,” Dr. Mayer shared.
Dr. Armstrong spoke about the challenges for advancing neuro-oncology survivorship. “Brain and spine tumors are rare so many health care providers only see a handful of these patients in their career,” she shared. Survival can be variable, but many patients have disease and treatment-related symptoms that can impact how they feel and function. In addition, patients will continue with surveillance for the rest of their lives.
Dr. Armstrong shared findings from the Natural History Study at NIH, which is following over 900 patients to learn the impact a brain or spine tumor can have on a person’s life. This can include neurologic and cognitive symptoms, functional limitations, and psychosocial changes.
Following the educational lectures, the presenters were asked questions from moderators Dr. Gilbert and David Arons, chief executive officer of the National Brain Tumor Society. The discussion included how to incorporate outcomes surveys in all clinical trials, include survivorship as standard care, create survivorship guidelines, and make guidelines feasible for everyone’s practice.
Then, patient and caregiver JC and Luanne shared their story. JC was diagnosed with an anaplastic astrocytoma in 1997. He had surgery, radiation, and participated in a clinical trial. Luanne has been his care partner and biggest advocate. They shared their emotional experience with a life-changing diagnosis, what they have learned, and how they have chosen to live intentionally.
The symposium continued with a panel discussion on survivorship research in neuro-oncology. The panel focused on the importance of early integration and palliative care, symptom management and assessment in general patient care and clinical trials, identifying risks for people with high symptom burden, and incorporating that into their care. Experts recommended utilizing networks to collaborate and find funding to support survivorship research. Experts also suggested sharing survivorship resources with patients and their care partners through specialists, community providers, and the general oncology community.
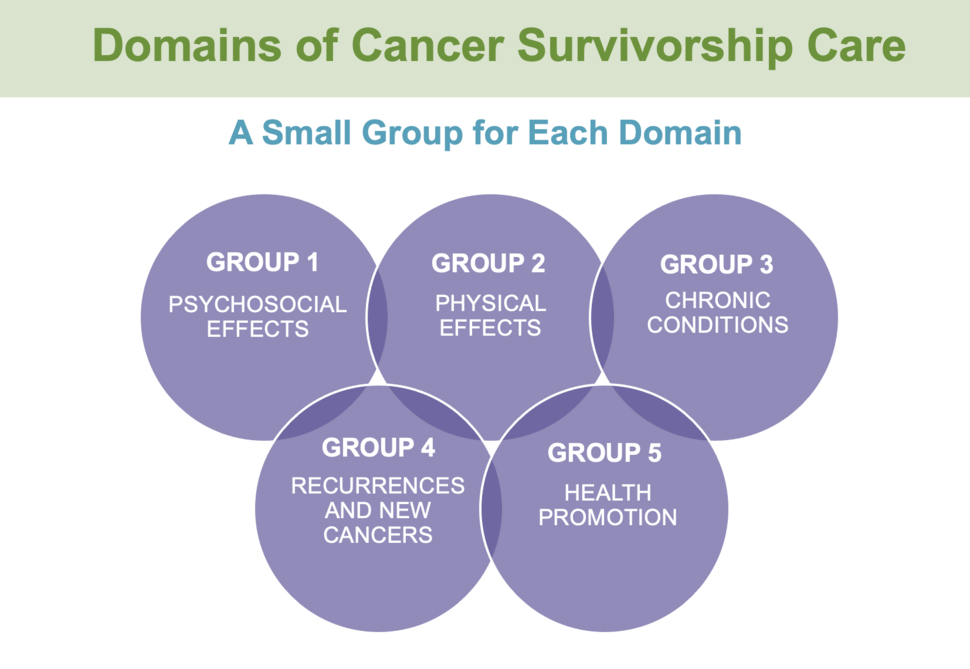
A second panel discussion focused on perspectives in neuro-oncology. The thought-provoking panel discussion focused on the importance of studying patient-centered outcomes in survivorship issues across the domains of cancer survivorship care (see figure), and collaborative disease-centered studies looking at biological mechanisms, disease outcomes, and patient reported outcomes. They recommended working in partnership with various disciplines to share common language with patients and their care partners.
"The symposium represents an opportunity for providers, patients, and advocates to all gather and discuss important aspects of survivorship care identified in oncology, and the unique needs of those with central nervous system tumors,” says Dr. Armstrong. “NCI-CONNECT and the NOB are committed to supporting these conversations and efforts to improve outcomes for those living with these devastating diagnoses.”
Survivorship Care Guidelines for the Medical Community
The second day of the symposium focused discussing specific topics in survivorship care. Breaking into small working groups enabled participants to identify opportunities to develop care guidelines that will inform clinical care and research focused on the gaps in brain and spine tumor survivorship.
To set the stage for group discussion, Brittany shared that she was diagnosed with an astrocytoma in 2019, two weeks after she had her second son. She shared the complications she experiences to help others understand what it is like living with a rare central nervous system tumor. Then, Dallas and his wife Janice shared what they have experienced through his 18-year journey with an ependymoma. Janice calls herself a co-survivor, and they shared their hope for research.
Bio-behavioral Specialist Alvina Acquaye of the NOB shared responses from a survey about survivorship care conducted prior to the symposium. Participants answered the survey to share what survivorship means to them, the top issues and challenges they face, and recommendations for improving survivorship in neuro-oncology.
The five working groups focused on the domains of cancer survivorship care:
- Chronic Conditions, led by Dr. Gilbert
- Recurrences and New Cancers, led by Marta Penas-Prado, M.D., of NCI
- Psychosocial Effects, led by Dr. Leeper
- Physical Effects, led by Dr. Armstrong
- Health Promotions, led by Dr. Tonorezos
The groups shared their findings, and symposium leaders Drs. Armstrong, Leeper, and Gilbert provided recommendations for next steps, including continued working groups based on the opportunities identified in care and research.
“This was a terrific symposium highlighting the importance of survivorship and the great opportunity for collaboration to improve patient outcomes,” says Dr. Gilbert. “The energy and enthusiasm of the participants will hopefully be translated into transformative actions.”