Statistical Report Highlights Key Trends in Adolescents and Young Adults with Brain Tumors
, by Raleigh McElvery, Neuro-Oncology Branch Scientific Communications Editor
The new analyses reveal critical information that will help providers and researchers understand the unique needs of these patients.
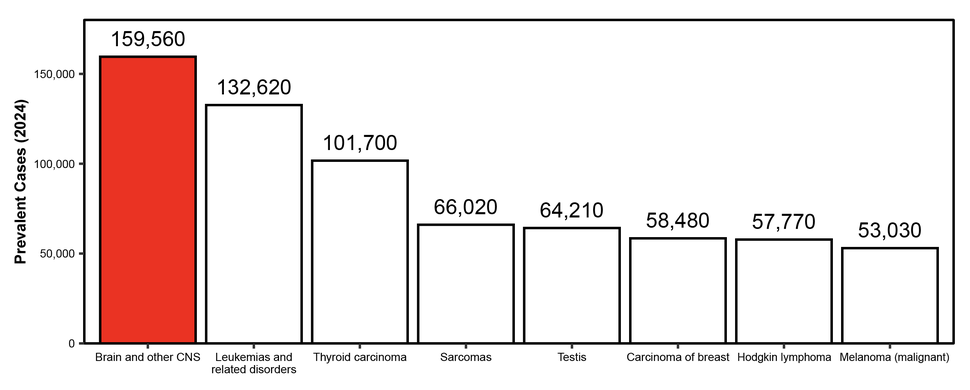
In the United States, there are roughly 110 million adolescents and young adults (AYAs) between the ages of 15 and 39 years old. Of those, about 208,620 are living with a primary brain or spinal cord tumor. Despite being relatively rare, these tumors, also known as central nervous system (CNS) tumors, are the most prevalent cancer in this age range. They are also the second leading cause of cancer-related death in AYAs—and the leading cause of death for those between 15 and 24 years old.
While cancer survival overall has been improving, the same is not true for the AYA population. Moreover, AYAs often go through a difficult adjustment between pediatric and adult cancer care. In fact, their tumors have unique molecular features that can be distinct from both pediatric and adult CNS tumors. This poses challenges for clinicians and makes it difficult to ensure accurate reporting, diagnosis, and treatment.
AYAs are also at a transitional period in their lives. Some are still experiencing developmental changes and asserting independence from parents, while others are earning degrees, working their first job, or starting a family. These factors all contribute to an AYA’s ability to adhere to treatment, attend appointments, and afford medical care. AYAs may also require specialized services, such as sex education, mental health counseling, vocational rehabilitation, family planning support, and work or school accommodations. As a result, it’s more important than ever to consider the unique needs of this group—and the barriers to care they face.
To understand how CNS tumors impact the AYA population, NCI-CONNECT (Comprehensive Oncology Network Evaluating Rare CNS Tumors), the Central Brain Tumor Registry of the United States (CBTRUS), and the American Brain Tumor Association (ABTA) have partnered on a new statistical report. The report, published in Neuro-Oncology, is a follow-on to a 2016 publication and explores statistical trends in AYAs with primary CNS tumors in the United States between 2016 and 2020. It is the first statistical report to analyze this unique population while incorporating current tumor classifications based on recent molecular data.
“We know far less about the burden of CNS tumors in AYAs compared to the pediatric and adult populations,” explains Quinn Ostrom, Ph.D., the study’s co-senior author, co-principal investigator at CBTRUS, and an assistant professor of neurosurgery at the Duke University School of Medicine. “Many AYAs who are diagnosed at a young age live for quite a long time—so not only is this a larger population than people may realize, but they also have unique needs. I hope this statistical report shows that there’s room for improvement. We can—and must—do better.”
A Unique Population with Unique Needs
Dr. Ostrom and her colleagues analyzed data from the largest datasets available for characterizing brain tumor incidence, prevalence, and survival in the United States, collected by CBTRUS, NCI, and the Centers for Disease Control and Prevention.
The researchers found that an average of 12,848 AYAs in the United States were diagnosed with a CNS tumor each year. About one quarter of those were malignant (cancerous), while the others were non-malignant (non-cancerous). Over 90 percent survived for at least five years.
“With more than 200,000 AYAs living with a primary brain or spine tumor, it’s critical for this community to have access to survivorship programs tailored to their specific needs,” says Nicole Willmarth, Ph.D., study co-author and the ABTA’s chief mission officer.
“As an advocacy organization, the ABTA offers customized information and resources to support the AYA community throughout various stages of their treatment journeys,” she explains. “As we gain a better understanding of the disease and the unique impact upon the lives of the AYA community, we will expand our resources to ensure optimal care and support for this age group. Our report is a first step toward that end goal.”
AYAs may also require specialized care depending on their age. The researchers found that the likelihood that an AYA will be diagnosed with a CNS tumor increases with age—and was highest for those between 35 and 39 years old.
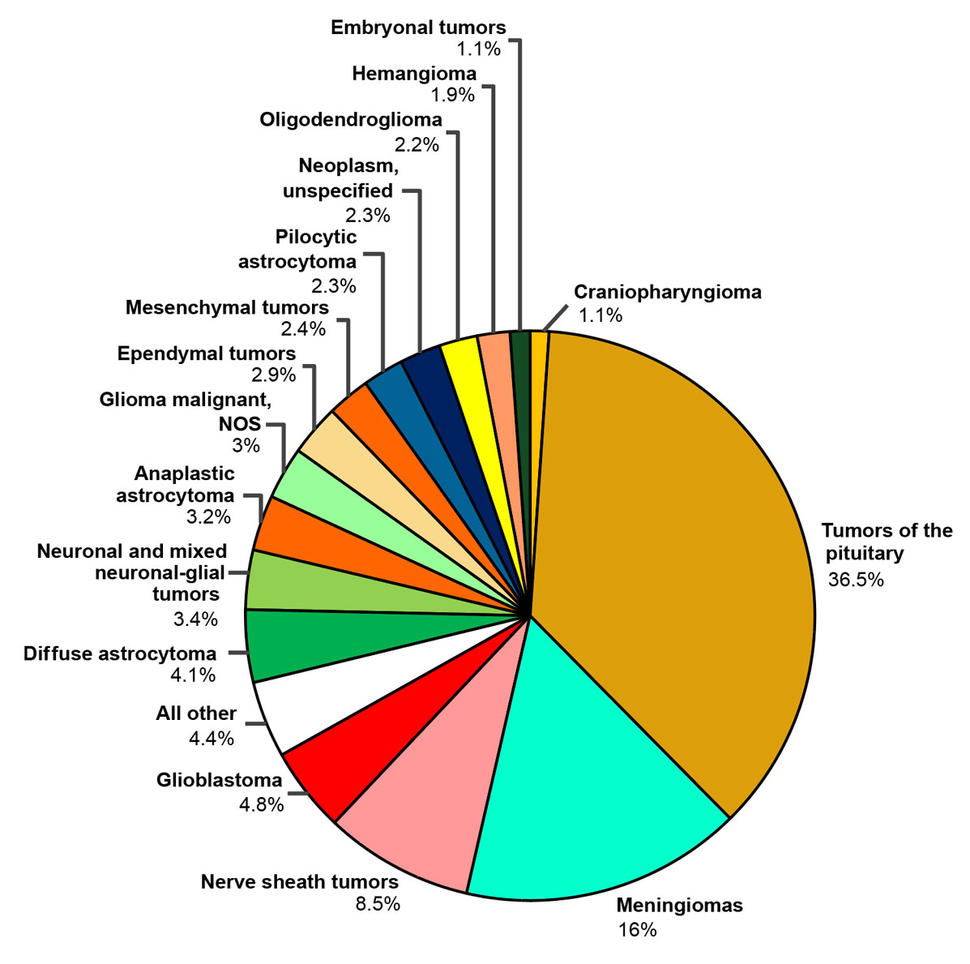
Brain tumor location also varies by age. Younger AYAs typically develop tumors in CNS areas that form early in development, such as the cerebellum and brainstem. These tumors become less common with age, while tumors of the meninges, the four lobes of the brain, and pituitary gland become more frequent. In fact, non-malignant pituitary tumors were the most common CNS tumor in the AYA population overall, especially for those under 30. The most common malignant tumors were adult-type diffuse gliomas—particularly lower grade gliomas, such as astrocytomas and oligodendrogliomas. Adults over age 40 are more likely to develop higher grade gliomas, especially glioblastomas. That’s why most research focuses on these tumors.
“When most people think about brain tumors, they picture glioblastomas or metastasis from breast or lung cancer,” says Marta Penas-Prado, M.D., study co-author and senior clinician for NCI-CONNECT. “But, as we showed, AYAs of different ages tend to get vastly different CNS tumors, which can make them feel isolated and alone. As clinicians, we need to help them understand their particular tumors, as well as how to navigate the unique life circumstances that this age group experiences.”
Assessing Risk Factors
Within the AYA population, the incidence of CNS tumors varied by demographic and by tumor type. The researchers found that female AYAs were more likely to develop these tumors than males. This is likely because certain tumor types, such as pituitary adenomas, have a higher frequency in AYAs and are generally more common in females of this age group. However, males were more likely to be diagnosed with malignant CNS tumors.
Incidence of CNS tumors was also highest in non-Hispanic American Indian/Alaska Native individuals, although malignant tumors were more frequent in non-Hispanic white individuals. However, due to limited data, Dr. Ostrom cautions that it’s difficult to disentangle increased risk in these populations from other factors, such as differences in health care access and data collection issues. For example, people who live in rural areas may need to travel farther for care, which could delay diagnosis and treatment. Those with limited or no health insurance may also be less willing to seek treatment if it’s expensive.
The data in the report were collected by hospitals and other medical facilities, and then transferred to state and national registries that shared the data with CBTRUS. As a result, the researchers were unable to ask patients about their insurance coverage, life circumstances, and other information that might reveal potential risk factors.
In general, not much is known about the risk factors for developing CNS tumors. So far, the only well-established environmental risk factor is exposure to therapeutic doses of ionizing radiation to the head and neck. However, this type of exposure is rare and likely doesn’t account for a large proportion of brain tumor cases. Some studies have also pinpointed certain genetic factors, syndromes, and environmental exposures. However, the brain tumor population is so small that it’s difficult to detect significant associations. According to Dr. Ostrom, there is also a lack of research focused on risk factors in the AYA population specifically.
Looking toward the Future
Since the initial 2016 statistical report, more molecular data and information on non-malignant CNS tumors has become available, Dr. Ostrom says. “We’re doing a much better job of counting people,” she explains, “which will help us determine the scale of targeted services this population requires.”
Her team estimates that 13,350 AYAs in the United States will be diagnosed with CNS tumors during 2024. They anticipate that most of those cases will involve non-malignant tumors of the sellar region, which is by the base of the skull and includes the pituitary gland. However, about a quarter of the CNS tumors diagnosed in AYAs this year will be malignant.
In the coming years, the researchers hope there will be more clinical trials for the AYA CNS tumor population. Coupled with the statistical trends in this new report, additional research will help provide more accurate diagnoses, better treatment, specialized care, and hope to AYAs living with this cancer.