An Introduction to Proteogenomics Part 2: Wielding the Proteomic Tools
, by Anna Roberts-Pilgrim, Ph.D.
In our last post, we outlined why proteins and their modifications are crucial components in finding effective ways to treat cancer and how proteogenomics can help us get closer to that answer. In this post we are going to dive into more detail about how proteogenomics is done and what information we have gleaned so far.
Mass Spectrometry: How High-Throughput Proteomics is Done
Let’s briefly start with how we examine proteins. For decades, antibody-based methods have been used to detect and quantify protein presence and localization through immunohistochemistry, western blots, or ELISAs. However, due to poor-quality or incorrect use of antibodies, these studies have been fraught with variable specificity, often lack sensitivity, and results in semi-quantitative analyses at best.
Enter the modern mass spectrometer—one of the more promising antibody-independent tools in protein research. In an effort to standardize and develop proteomic techniques using MS, NCI formed the Office of Cancer Clinical Proteomics Research (OCCPR) in 2006.
MS uses a combination of ionization and electro-magnetic fields to separate peptides by their mass-to-charge ratios and analyze their fingerprints. Each fingerprint has the potential to tell us not only what proteins are present, but also which posttranslational modifications (PTMs) and their quantities. High quality antibodies can also be coupled with MS in order to target specific proteins.
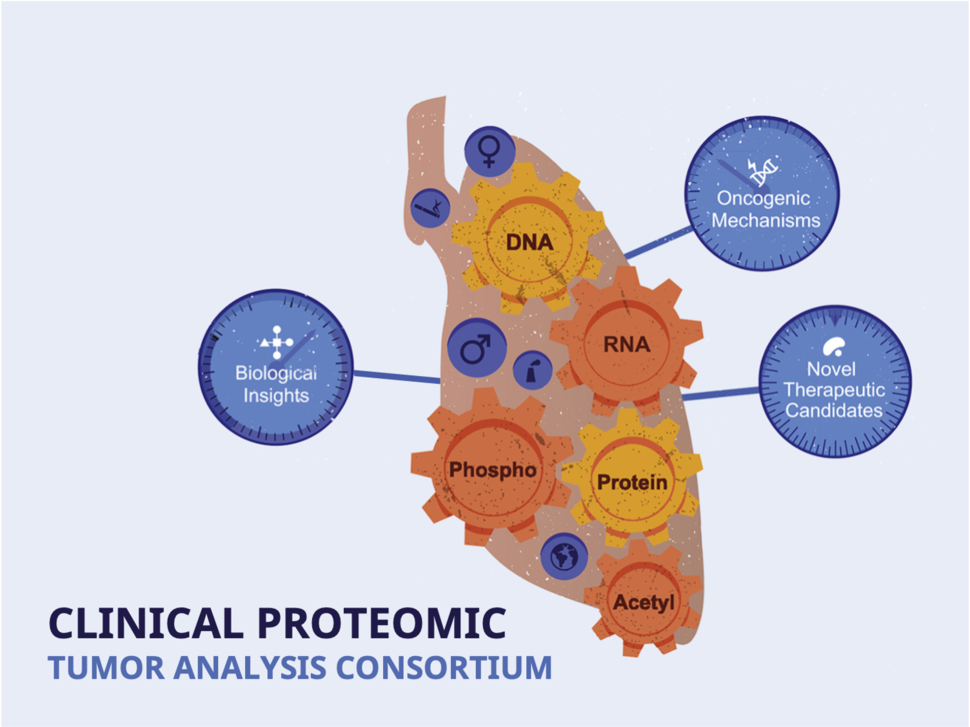
The team of scientific experts at OCCPR were tasked with standardizing MS for reliable, comprehensive analysis of proteins. With the formation of the Clinical Proteomic Tumor Analysis Consortium (CPTAC), and later the International Cancer Proteomic Consortium (ICPC), OCCPR has been able to deploy these standards in new tumor characterization research projects and utilize them to discover newfound tumor biology.
What Have We Learned So Far?
As mentioned in part 1 of this series, proteogenomics layers proteomic data with genomic and transcriptomic data—acting as a powerful tool OCCPR uses to enhance our understanding of human cancer. Each tumor study examines 100–200 treatment naïve tumors and normal adjacent tissues to scrutinize tumor progression, defense against the body’s immune system, and perhaps most importantly, vulnerabilities which may potentially be exploited for diagnostic and therapeutic use. In addition to proteomic and phosphoproteomic profiles of each tumor, the studies often integrate complementary large-scale techniques, such as glycomics, ubiquitylomics, acetylomics, methylomics, lipidomics, etc.
To date, the CPTAC program has examined colorectal, kidney, endometrial, breast, ovarian, lung adenocarcinoma, lung squamous cell carcinoma, pancreatic, head and neck squamous, glioblastoma and pediatric brain cancers. Additionally, the ICPC has examined liver, gastric, oral squamous and lung adenocarcinoma cancers to date. All these findings rely on the use of proteomics and proteogenomics. Let’s dig in and discover more of what these studies have found.
Additional Insights into Tumor Subtypes
Our knowledge of tumor biology and progression has grown throughout the decades, but tumor response to therapy is still largely unpredictable and poorly understood. The identification of several novel genomic and proteomic tumor subtypes through CPTAC and ICPC studies have helped shed light on drug efficacy, drug targets, survival, and recurrence.
By proteomically examining factors such as cell cycle, micro-environment, and known genomic targets, the CPTAC pediatric brain cancer study (in press), done in collaboration with the Childhood Brain Tumor Network (CBTN), stratified a subset of clustering craniopharyngioma tumors into two distinct subtypes. One subgroup showed strikingly similar proteomic and phosphoproteomic characteristics with pediatric low-grade gliomas (LGGs) harboring BRAFV600E mutations, and further identified an upregulation of key MEK/ERK/AKT kinases within the tumor micro-environment.
This new information suggests MEK and mTOR inhibitors may be effective in this subset of pediatric patients—potentially a new treatment avenue in a tumor which has had no major therapeutic developments in the past 50 years! This finding is currently being explored further for clinical trial testing.
Also revealed in this study are a novel set of prognostic biomarkers for high-grade glioma (HGG) tumors that do not have mutations in the H3K27M gene—the common biomarker used for diagnosis, and further stratification of HGG tumors that may warrant differing therapeutic approaches.
The ICPC lung adenocarcinoma (LUAD) study proteomically identified a novel ‘late-like’ tumor subtype in early stage, non-smoking Taiwanese patients with EGFR L858R mutations. These tumors are aggressive, displaying shorter survival outcomes and higher tendencies to develop malignant pleural effusion and metastasis. Researchers also identified significant increases in MMP11 protein levels as a promising early-stage LUAD biomarker candidate, which would give clinicians an early indication of high-risk patients for aggressive treatment options.
Characterizing Immune Microenvironments and Predicting Response to Immunotherapy
The tumor immune micro-environment harbors evidence of how a tumor protects itself against the body’s immune system and further how a tumor might respond to immunotherapy. CPTAC and ICPC studies examine the tumors’ epithelial, endothelial, dendritic, T cells, and B Cells, along with other immune components and have already uncovered some amazing insights into tumor behavior.
Four major tumor immune subtypes were identified through proteogenomic characterization in the CPTAC clear cell renal cell carcinoma (ccRCC) study. These subtypes (CD8+ inflamed, CD8- inflamed, VEGF immune desert, and metabolic immune desert) are predicted to respond disparately to immune checkpoint and anti-VEGF therapies.
Notably, CD8+ inflamed tumors, marked with a high degree of CD8+ T cell infiltration and increased expression of immune evasion markers, may be ideal candidates for immune checkpoint therapy while CD8- inflamed tumors, characterized by an innate immune signature, may be non-responsive to the same therapy.
CPTAC’s LUAD study revealed exclusively through proteomic data, several potential tumor immunosuppressive mechanisms and therapeutic targets involving STK11 mutations, thereby suggesting relevant targets beyond the conventional PD1 and PD-L1 markers.
Further, the LUAD study sheds light on a confounding observation in a subset of immune ‘hot’ tumors, where immune cells have seemingly identified and infiltrated tumor tissue but failed to attack the tumor. These tumors had elevated protein levels of immune evasion markers IDO1 and CTLA4, effectively hiding the tumor from its host. Inhibition of these markers may be further explored for suppressing this tumor subtype in LUAD patients.
Different Paths to Altered Pathways and Protein Expression
Next, let’s examine how proteogenomic studies can help elucidate tumor behavior by examining deviations to the central dogma pipeline discussed in part 1. Driver mutations often lead to altered proteome and phosphoproteome pathways, as well as changes in other PTMs such as glycosylation, acetylation, methylation, lipidation, and ubiquitinylation. In some cases, altered proteins may be identified in the absence of putative driving mutations, providing an opportunity for targeted therapy that would otherwise be overlooked.
In the CPTAC high-grade serous carcinoma (HGSC) study, researchers identified a ‘proliferation-induced replication stress’ mechanism which accelerates cancer progression and causes chromosomal instability, a feature associated with ovarian cancer. This mechanism prompts a cellular stress response by stimulating tumor cells to continually multiply at an increased rate. The stress was shown to be associated with an increase in CDK-RB and AURKA protein phosphorylation—two proliferation-associated pathways that have existing, FDA-approved targeted drug therapeutics, but presently not approved for use with HGSC.
Strong associations between decreased CD8 T-cell infiltration and increased glycolysis in microsatellite instability-high (MSI-H) tumors were identified in the CPTAC colorectal tumor study. These findings suggest glycolysis as a potential alternate target for immune checkpoint blockade-resistant MSI-H tumors. Proteomic and phosphoproteomic data also identified candidate tumor antigens for cancer vaccine development.
Data, Software, Assays and Antibodies: Springboards for the Community
But wait! There’s more! Each CPTAC and ICPC study generates an enormous amount of raw proteogenomic data, as well as an initial analysis of each tumor’s biology—all made publicly available through NCI’s Proteomic Data Commons, Genomic Data Commons, the Cancer Imaging Archive and through open-access articles. The OCCPR also develops freely available MS assays that are characterized according to CPTAC guidelines, antibodies that are rigorously validated (including targeted-MS antibodies for use in various MS applications), and software for proteomic and proteogenomic analysis.
All of these studies provide mere starting points for further exploration. For example, novel targets proposed in CPTAC studies need to be validated and their potential therapies need to be identified and tested before we can even start to consider their impact on patients. Fueling hypothesis-driven studies that exploit the data to find novel means of diagnosis or therapeutics by the scientific community is the ultimate goal for CPTAC. We depend on you (the reader) to explore our smorgasbord of theories and insights and take them to the next level.
Translating Proteogenomic Findings into Clinical Applications
OCCPR has established standards in proteomic rigor and reproducibility, applied these standards to large-scale cancer characterization studies, and most recently, expanded to translational studies. The Proteogenomic Translational Research Centers (CPTAC-PTRCs) are the clinically driven arms of our program that focus on turning CPTAC findings into clinically-relevant output. Currently, CPTAC-PTRCs are testing targets and potential therapeutics identified in the acute myeloid leukemia, breast cancer and ovarian cancer studies on patient-derived samples. By working in collaboration with clinical researchers, CPTAC-PTRCs are uniquely positioned to answer clinical questions about understanding drug responses and resistance to therapies.