New treatment option for young women with hormone-sensitive breast cancer
- Posted:
240-760-6600
A drug used for treating breast cancer, known as exemestane, is more effective than a common breast cancer prevention drug, tamoxifen, in preventing breast cancer recurrence in young women who also receive post-surgical treatment to suppress ovarian function. The findings from this trial were in women who had a form of early breast cancer that was sensitive to hormonal treatment.
The study was conducted by the International Breast Cancer Study Group (IBSCG), in partnership with the Breast International Group (BIG) and the North American Breast Cancer Group, and funded by the U.S. National Cancer Institute (NCI), IBSCG, and the pharmaceutical companies Pfizer and Ipsen. The combined results of the TEXT (Tamoxifen and Exemestane Trial) and SOFT (Suppression of Ovarian Function Trial) were presented today at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago (late breaking abstract #1) and published online in the New England Journal of Medicine.
Treatment with exemestane plus ovarian function suppression reduced the risk of any invasive cancer by 28 percent, and reduced the risk of invasive breast cancer recurrence by 34 percent, compared to treatment with tamoxifen plus ovarian function suppression. At five years from study entry, 92.8 percent of women remained free from breast cancer after treatment with exemestane plus ovarian function suppression; 88.8 percent were breast cancer-free after receiving tamoxifen plus ovarian function suppression.
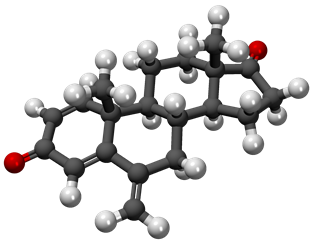
Treatment with an aromatase inhibitor, such as exemestane, has previously been demonstrated to benefit postmenopausal breast cancer patients compared to treatment with tamoxifen. Aromatase inhibitors prevent the formation of estradiol, a female hormone, by interfering with an aromatase enzyme. Both trials were conducted to determine whether this benefit could be extended to premenopausal women by combining exemestane with ovarian function suppression. Hormone-sensitive breast cancer, defined as estrogen and/or progesterone receptor-positive breast cancer, represents 79 percent of breast cancers diagnosed in women under age 50 in the United States.
The TEXT and SOFT trials were phase III, randomized clinical trials that enrolled 2,672 and 3,066 premenopausal women with hormone receptor-positive early breast cancer, respectively, between November 2003 and April 2011. Over 500 medical institutions from 27 countries enrolled women in the trials. In the two trials, 4,690 women were randomly assigned to 5 years of adjuvant, or post-surgical, treatment with exemestane plus ovarian function suppression or assigned to tamoxifen plus ovarian function suppression. SOFT included a third treatment assignment, tamoxifen alone, which will be analyzed in late 2014. The women may also have received chemotherapy as part of adjuvant treatment.
The two trials were designed to be complementary. They were conducted over the same time period, in the same general population, and have the two treatments in common. Combining them brought the results to doctors and patients sooner than if they were presented separately.
Ovarian function suppression has been used for decades as a breast cancer treatment for premenopausal women, though whether it adds benefit when combined with other treatments was still uncertain. In these trials ovarian function suppression was combined with either tamoxifen or exemestane. In premenopausal women use of an aromatase inhibitor such as exemestane requires suppression of estrogen produced by the ovaries. In TEXT and SOFT, ovarian function suppression was achieved by use of monthly injections of the GnRH agonist triptorelin, surgical removal of both ovaries, or radiation therapy to the ovaries.
“These results provide a new treatment option for young women with hormone-sensitive breast cancer. The trials demonstrate that an aromatase inhibitor, previously recommended only for postmenopausal women, is also effective for premenopausal women when combined with ovarian function suppression,” said study co-chair Olivia Pagani, M.D., Breast Unit Clinical Director at the Oncology Institute of Southern Switzerland in Bellinzona, Switzerland. “As a physician who routinely recommends ovarian function suppression as adjuvant therapy for some young patients, these results will change my practice. I will combine ovarian function suppression with an aromatase inhibitor rather than with tamoxifen.”
Support from NCI enabled American and Canadian participation in the TEXT and SOFT trials through the North American Breast Cancer Group (NABCG). NABCG contributed one-third of all patient enrollments in the TEXT and SOFT trials, whereas two-thirds enrolled from cooperative oncology groups affiliated with the Breast International Group (BIG) network. Led by Alliance (formerly CALGB), North American involvement accelerated trial recruitment, permitting earlier reporting of findings and faster access to these practice-changing results.
In addition to assessing the effectiveness of the treatments at reducing recurrence, patient-reported quality of life assessments were collected throughout the five years as well as physician-reported side effects. “As clinicians we should be reassured that, in the two treatments studied, the patient-reported quality of life results were similar overall, as was the frequency of severe side effects,” said study co-chair Barbara Walley, M.D., Medical Oncologist at the Tom Baker Cancer Centre in Calgary, Canada and executive member of the Breast Disease Site Committee, National Cancer Institute of Canada-Clinical Trials Group. “The side effects reported in this premenopausal population are similar to those in postmenopausal women in which tamoxifen and aromatase inhibitors are widely prescribed.” Follow-up of the young women participating in the trials continues to assess long-term prognosis, tolerability, and side effects.
“These results underscore the importance of international research collaboration in improving patient outcomes in North America and beyond, such as for the young women in this study,” said Richard Gelber, Ph.D., professor, Harvard Medical School and director, IBCSG Statistical Center, Dana-Farber Cancer Institute, Boston. “This partnership between NCI and IBCSG represents a successful model for future clinical research advances.”
###
Reference: Pagani O, et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. NEJM early online. June 1, 2014. ASCO late breaking abstract #1. TEXT: Clinicaltrials.govNCT00066703. SOFT: Clinicaltrials.govNCT00066690.
NCI leads the National Cancer Program and the NIH effort to dramatically reduce the prevalence of cancer and improve the lives of cancer patients and their families, through research into prevention and cancer biology, the development of new interventions, and the training and mentoring of new researchers. For more information about cancer, please visit the NCI Web site at http://www.cancer.gov or call NCI's Cancer Information Service at 1-800-4-CANCER (1-800-422-6237).
NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit http://www.nih.gov.
The International Breast Cancer Study Group (IBCSG) is a Swiss nonprofit cooperative breast cancer research organization that has conducted clinical research in adjuvant endocrine therapy and chemotherapy, timing and duration of adjuvant therapies, and quality of life for over 35 years.