Combatting Stress and Promoting Wellness in Cancer Care
, by Rebecca Zacuto, Neuro-Oncology Branch Communications Fellow
Outcomes Program Manager Alvina Acquaye-Mallory answers questions about how health care providers, patients, and caregivers can cope with stress and burnout during their cancer care journey.
Burnout is a phenomenon characterized by repeated, prolonged stress. The complex demands on the current health care workforce—such as excessive workloads, administrative burdens, scheduling challenges, and lack of organizational support—are causing many health workers to experience burnout. Patients and their caregivers, too, may experience high stress levels as they manage similar demands and frustrations while coping with a rare cancer diagnosis. Addressing burnout in health workers, patients, and caregivers is key to ensuring that patients receive quality care.
In 2020, members of NCI Center for Cancer Research’s Neuro-Oncology Branch (NOB) Outcomes Program—including Senior Investigator and NCI-CONNECT Co-Lead Terri Armstrong, Ph.D., as well as Elizabeth Vera and Alvina Acquaye-Mallory—collaborated with other neuro-oncology researchers to better understand burnout among those caring for patients with brain tumors. Surveying members of the Society for Neuro-Oncology and the European Association of Neuro-Oncology, the team found that the majority experienced high levels of burnout, characterized mainly by individual factors, including emotional exhaustion and concerns over personal achievement.
Building on this work, the researchers recently published a new study demonstrating that the prevalence of burnout among young investigators in neuro-oncology is also high and is mainly characterized by overextension, warranting interventions at institutional and organizational levels. These results highlight the complexity of burnout and need for interventions that address person-centered approaches, in addition to organizational challenges.
Acquaye-Mallory, NOB Outcomes Program manager, has a particular interest in health and wellness, based on her training as a therapist. She supports research evaluating psychological support in patients, and provides health and wellness practices to neuro-oncology patients and providers. She sat down with us to discuss how providers, patients, and caregivers can manage their stress—and why it’s important to promote wellness in all areas of life.
Q: How is the NOB lessening stress for those working in neuro-oncology, patients, and caregivers?
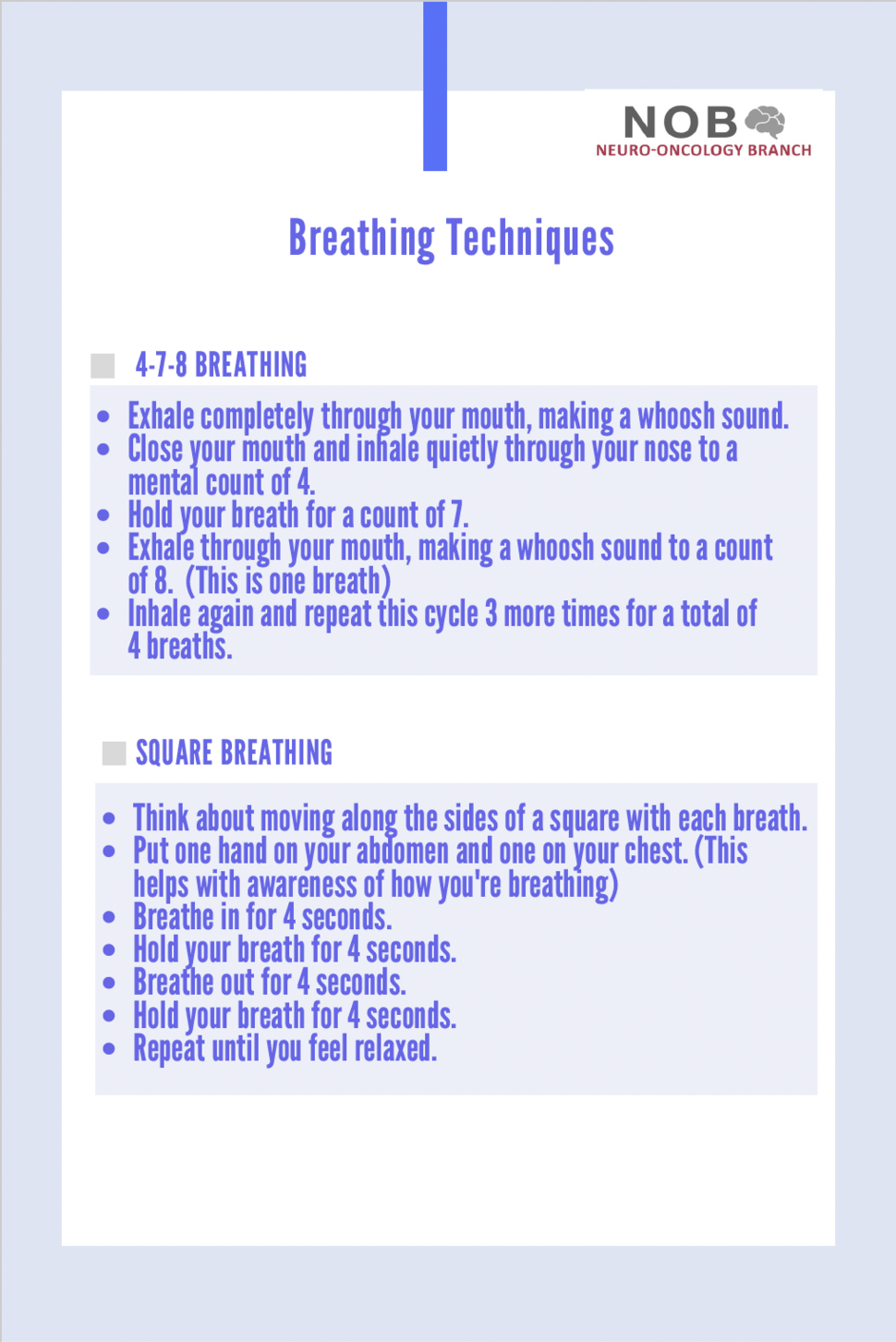
A: We recognize that travel and learning more about a tumor diagnosis can cause stress for both patients and caregivers. To provide support during these clinical visits, we put together “care bags” for patients and caregivers seen in the NOB’s Neuro-Oncology Clinic and the NCI-CONNECT Clinic. These bags contained brain-shaped stress balls, water bottles, lip balm, hand sanitizer. I also made a card with tips for breathing techniques to help de-stress, as well as how to check in with yourself and transition from clinical care or an appointment to home.
As with many healthcare systems, the way staff work has changed, with fewer large group gatherings and more virtual meetings. So, celebrating life events (even virtually) is a good way to create community. We host virtual Branch holiday parties, as well as monthly Branch-wide meetings in which staff are invited to share their good news. At these virtual gatherings, Branch Chief Mark Gilbert, M.D., inserts humor by sharing jokes and puns. We also include interactive activities, such as hosting Jeopardy games, which always gets people excited and makes virtual meetings more engaging for participants.
We maximize interactions during in-person events as well. Last spring we threw a farewell party to say goodbye to our trainees who were moving on to the next stage of their careers. This activity included food and outdoor kite flying. We’ve also organized events to provide encouragement to staff in the clinic, such as pet therapy events. Lieutenant Commander (LCDR) Abigail—the canine mascot of the U.S. Public Health Service—visited our clinic staff to provide both education and support. Staff members got to pet Abigail, give her treats, and learn about the health benefits of the human-animal bond.
Creating these small moments is important. It allows people to take a break and find some joy in the little things at work, which can help manage emotional exhaustion.
Q: Why is stress a significant issue for health care providers?
A: Health care providers balance a lot, including caring for patients who have a variety of needs and are at various stages of their treatment journeys. For example, some patients may need help interpreting test results, while others may need help coping with specific symptoms. Providers may feel like they never know exactly what they will encounter each day in clinic, making each day different and challenging.
Encouraging health care providers to take time to recognize their stress in the moment can help them manage it, especially when dealing with uncertainty and constant repetition. Preparing for appointments and providing attention and care to patients makes providers feel like they are “on” the whole day. Theses reminders about self-care are essential to provide the best care for patients.
Q: What are some techniques to help providers manage their stress?
A: It’s always important to check in with yourself, especially after seeing a patient or attending a meeting. If you’re fine, move on to the next task. If you are feeling flustered or irritable, ask yourself what you may need. Get some water or food, walk around, or listen to music before starting your next task. Also, stretching your body and moving around can help if you are feeling tense.
One of the easiest de-stressing techniques is diaphragmatic breathing, also called deep breathing or belly breathing. It involves taking slow, controlled breaths. This type of breathing allows you to take a moment for yourself and calm down your mind and body. It can be especially helpful in moments when you feel anxious or overwhelmed.
These practices are easy to do, they don’t take long, and they can help you manage your emotional “temperature,” which is just understanding how you’re feeling in the moment.
Q: What are some tips to help patients and caregivers manage stress?
A: Breathing, de-stressing exercises, and checking in with yourself are all helpful for patients and caregivers, too. Our NCI-CONNECT website has helpful communication tips for caregivers and patients. Sharing with your partner how things are going, checking in with them, or even seeing a therapist together can be helpful. Communication is key, whether you’ve just started your treatment journey or been on it for a while.
If you are not ready to talk about certain things, journaling can be a great first step. It allows you to work through your feelings and think through ways to manage your emotions. Taking care of how you feel is key, and—in all areas of life—creating small moments of connection goes a long way.