Exercise
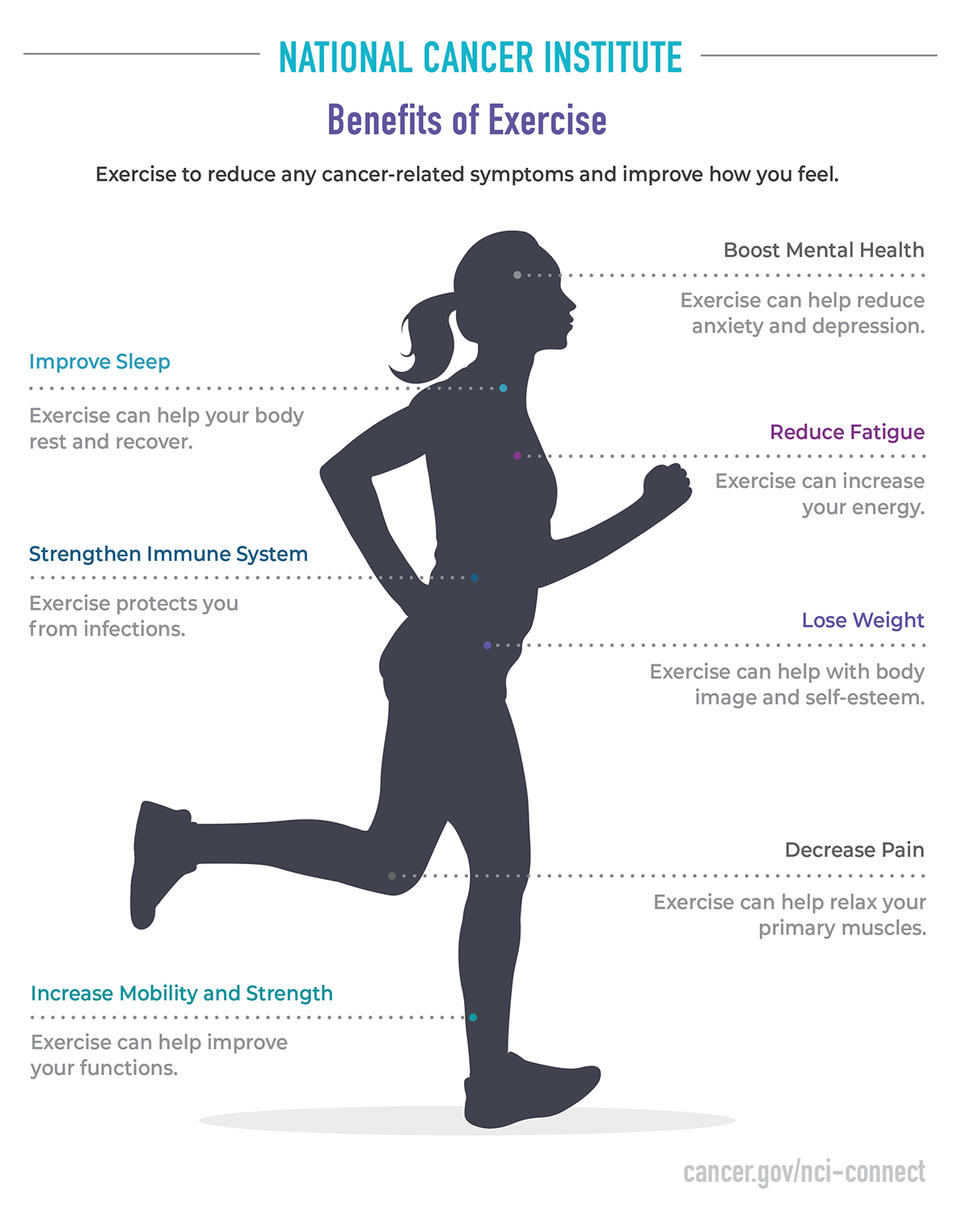
A brain or spine tumor and treatment side effects can cause changes to body functions, including your movement and balance. If you feel well enough and are able, exercise may reduce symptoms and improve the way you feel. But it’s important to seek the advice of your health care team prior to starting any exercises. Ask what type of exercises are recommended, the amount, and any necessary restrictions to keep you safe.
Exercise doesn’t have to be hard. It can be any activity that gets your body moving. It can be mild, moderate, or intense, depending on how you feel or where you are in your cancer journey. Below are examples of exercises that are considered mild, moderate, or intense.
- Mild exercises: Stretching, standing, arm or leg lifts, and gentle movements
- Moderate exercises: Walking, water aerobics, slow biking, dancing, light resistance training, and gardening
- Intense exercises: Running, swimming, aerobic dancing, heavy resistance training, and hiking uphill
Exercise can help reduce fatigue, anxiety, and depression. It can also improve your sleep. It’s important to listen to your body and understand what it tells you. Your doctor or physical therapist can help you determine what exercise is right for you. Exercise should be personalized based on how you feel and your unique needs, abilities, and interests. Ask your doctor about limitations, such as how much you can lift or which movements (like turning or squatting) might impact certain symptoms.
Overheating and rapid breathing can trigger seizures. If you have experienced seizures or are at risk, ask about recommendations and limitations. Do not exercise alone if you have previously had seizures or have physical limitations that put you at risk for falling or injury.
Exercise Tips
- Find a physical or occupational therapist trained in neurological problems to help you create a weekly exercise plan. Ask them to:
- Plan exercises that can be done safely at home or nearby
- Include gentle stretching in your exercise plan
- Start slowly and don’t push yourself too hard. You may not be able to exercise at the same level as you did before your diagnosis. Consider adjusting your exercise schedule in response. You could try:
- Twenty minutes of mild to moderate exercise three to five times per week
- Five to ten minutes of exercise two to three times a day
- Try using a fitness app to log your activity
- Watch exercise videos from the internet
- Find an exercise partner who will hold you accountable and help keep you safe
- Set goals and reward yourself
Write down your exercises, the time, and any side effects you experience. Share this information with your doctor. The My STORITM app can help you keep track of your symptoms and self-care activities.
You may be able to start exercising at any point during your cancer journey, even if you’ve never exercised before. The amount and the intensity should be based on your comfort and what your doctor recommends. You may find it helpful to continue exercises you learned from physical or occupational therapy—or you may want to find new ones to try.
Any amount of exercise or movement each day is better than none. You may start by walking around your room or getting up and down from a chair. You can slowly add to the type and amount of exercise as your health permits. Exercise can help keep you strong and make you feel good.
Resources
Sleep
Having a brain or spine tumor and undergoing treatments can cause sleep disturbances. Sleep is important for physical and mental health, as well as overall quality of life. Lack of adequate sleep can affect your immune system and, if chronic, increase your risk of heart disease, anxiety, and depression. Sleep allows your body to rest, recover, and reset for the next day.
Sleep Tips
- Stick to a sleep schedule so you go to bed and wake up around the same time every day
- Go to bed when you feel sleepy to help you fall and stay asleep
- Create a bedtime routine that helps you decompress from your day and ease into sleep
- Practice relaxation techniques before bed, such as meditation, breathing exercises, and guided imagery
- Do not use electronic devices 20 to 30 minutes before bed.
- Keep your room dark by using blackout curtains and covering bright electronics
- Limit caffeine intake during the day to less than four cups and avoid caffeinated drinks before bed
- Exercise more than three hours before bed to allow time for your body to wind down
- Train your body to know that your bed is only for sleeping by limiting the time you spend on your phone, on your laptop, or watching TV in bed
- If you don’t fall asleep within 20 minutes, try reading a book or getting out of bed and returning when you feel sleepy
Write down your naps and the amount of time you sleep at night—or track this information on the My STORITM app. Share this information with your doctor.
Talk with your doctor or care team if you always have difficulty sleeping or if you’re sleeping more than normal. Being tired more often is a common side effect of any cancer treatment. Excessive tiredness, however, needs to be addressed. Your health care team can plan a sleep disorder assessment, provide other therapies, or adjust your medications.
Resources
Nutrition
Treatment side effects may affect your ability to eat a well-balanced diet. You may have nausea, vomiting, and decreased appetite. If you’re on steroids to control brain tumor swelling, you may crave unhealthy snacks, gain weight, and have high blood sugar. But a healthy and balanced diet is still important. It can give you the key nutrients your body needs to strengthen your immune system, give you energy, and help you stay a healthy weight.
Nutrition Tips
- Limit processed foods (pre-packaged foods that contain added sugars and fats)
- Eat plenty of fruits and vegetables
- Avoid sugary drinks
- Avoid alcohol as it can make your symptoms worse
- Drink plenty of water to stay hydrated (use this formula to calculate how many ounces you should drink a day)
- Eat six small meals daily to keep your metabolism working, stave off hunger, and control your blood sugar
- Keep a food log to track your intake of healthy foods
- Pack small, healthy snacks to avoid eating unhealthy foods when you’re on the go
- Prepare meals in bulk over the weekend so you have healthy options during a busy week
- Allow yourself a weekly or monthly “cheat day”
Write down your diet, including what you eat and drink, the time of your meals, and any side effects you experience. Share this information with your doctor.
Try to follow the diet your doctor recommends. Remember, foods that contain little to no nutrients often contain sugar, fat, and artificial ingredients. You will feel better both physically and emotionally when you eat healthy foods.
Resources
Symptom Management
A brain or spine tumor and treatment can cause a variety of symptoms. Common symptoms include headaches, nausea with or without vomiting, constipation, fatigue, increased sleep, weakness on one side of the body, and difficulty walking and balancing.
Brain tumors can also cause seizures and spine tumors can cause pain. You may have other unique symptoms based on your tumor size, location, and how fast it grows.
Symptom Management Tips
- Make taking care of yourself a priority, especially when you don't feel well.
- Keep a log of any symptoms you experience using the My STORITM app or in a journal. Note when and how often they occur, and what may make them better or worse.
- Talk with your doctor about your symptoms.
- Take any prescribed medicines for your symptoms as directed. Talk with your doctor if you miss a dose and avoid abruptly stopping medications. Tell your doctor if they help or not.
- Some medications are prescribed “as needed.” Ask for clear instructions about when to take these medications and what to expect in terms of improvement and potential side effects.
- Tell your physical or occupational therapist how you feel during and after your sessions.
- Ask for help when you need it.
Write down your medication doses, the time you take them, how you feel after you take them, and any medication-related side effects. Ask if there are prescribed medications, over-the-counter medications, or supplements you should take to manage these side effects. Share this information with your doctor.
Talk to your doctor about any new or worsening symptoms. There may be medicines or other therapies that can help. Taking care of yourself and your symptoms can go a long way in helping you feel and function at your best.
Resources
Alvina's Quick Tip:
Daily Reminders
When life seems challenging, NCI-CONNECT Health and Wellness Counselor Alvina Acquaye-Mallory says daily reminders can help you stay positive. Watch the video