Targeted Therapies, Tooth Extraction, and Metastasis
, by Jim Hartley
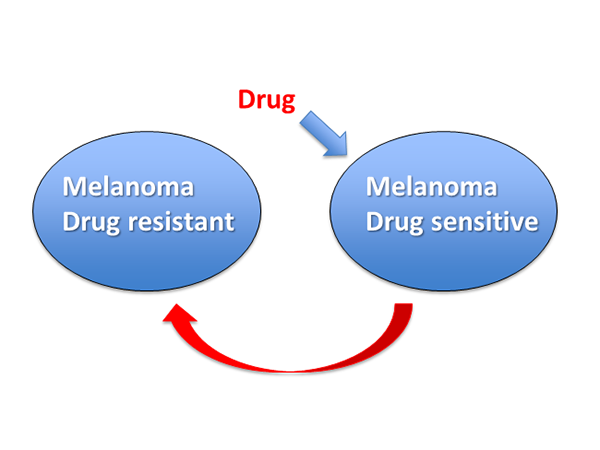
Oncogenic mutations in RAS pathway genes such as BRAF and NRAS play a significant role in melanoma, and patients with the BRAFV600E mutation often show impressive responses to targeted therapies. Usually, however, such responses are short-lived due to the rise of resistant clones. Obenauf, Rosen, Massague, and colleagues have extended earlier work in a breast cancer model (Kim, et al., Cell 139, 1315, 2009, PMID 20064377) and recently published an intriguing study of the mechanisms and dynamics of drug resistance arising in the context of dying, drug-sensitive melanoma cells (Obenauf, et al., Nature 520, 368, 2015, PMID 25807485). Their principal finding was that sensitive tumor cells treated with drug promote the proliferation of drug-resistant cells lurking in the background of heterogeneous tumors, and attract drug-resistant cells to recolonize solid tumors in mice.
The authors started by selecting a line of A375 cells (which according to the ATCC are homozygous mutant in both BRAF and CDKN2A), A375R, for resistance to vemurafenib. Tumors in mice formed by drug-sensitive A375 cells were colonised by injected, luciferase-labeled drug-resistant A375R cells much more extensively when the mice were treated with vemurafenib than with vehicle. Similarly, A375R cells grew more rapidly in vitro when co-cultured with sensitive A375 cells in the presence of drug, or when A375R cells were treated with conditioned medium from sensitive cells treated with drug. Finally, culture medium from sensitive cells treated with low levels (0.1 µM) of vemurafenib partially protected sensitive cells from lethal levels (3 µM) of the drug and decreased apoptosis caused by the drug. The authors concluded that treatment of sensitive cells with drug induced expression of a "therapy-induced secretome", TIS, which stimulated the proliferation of and attracted resistant cells and also protected sensitive cells in trans.
Unfortunately the TIS proved to be complex. Over 5000 genes in drug-treated sensitive cells were differentially expressed, including more than 400 with predicted extracellular locations. Crossing identified transcription factors with binding sites on differentially-regulated genes identified down-regulation of the transcription factor FRA1 as being correlated with the TIS of three types of tumor cells treated with three drugs (vemurafenib, crizotinib, and erlotinib), and inhibition of FRA1 expression with shRNA mimicked drug treatment. Analysis of mRNAs in resistant cells harvested from a regressing mouse tumor indicated activation of several pathways, and featured especially the PI3K / AKT pathway. Most noteworthy was the observation that combined therapy with vemurafenib and AKT or PI3K/mTOR drugs inhibited proliferation of resistant cells in mixed sensitive + resistant tumors, but had no effect on tumors comprising only resistant cells.
In a separate review of Obenauf, et al., Rene Bernards (Cell Res 25, 763, 2015, PMID 25895608) connected the therapy-induced secretome to wound healing responses after cancer surgery, and noted the "well-documented" observation of local recurrence of cancer at the site of tooth extraction. The abstract from that reference (Hirshberg, et al., J Oral Maxillofac Surg 51, 1334, 1993, PMID 8229413) reads in part: "Review of the literature revealed 55 cases where tooth extraction preceded the discovery of metastases. The lung and breast were the most common sources of the metastasis, and the mandibular premolar area was the most common site. A soft tissue mass extruding from a recent extraction wound, and accompanied by pain, were the main symptoms in most patients. The mean time from discovery of the metastasis to death was 3.8 months. Tooth extraction appears to serve as a promoting factor in the metastatic process."
Thus the modern phenomenon of resistance to targeted cancer therapies may share features with evolutionarily ancient and fundamental biological responses to tissue damage. Drugging one without impairing the other may be a delicate process.