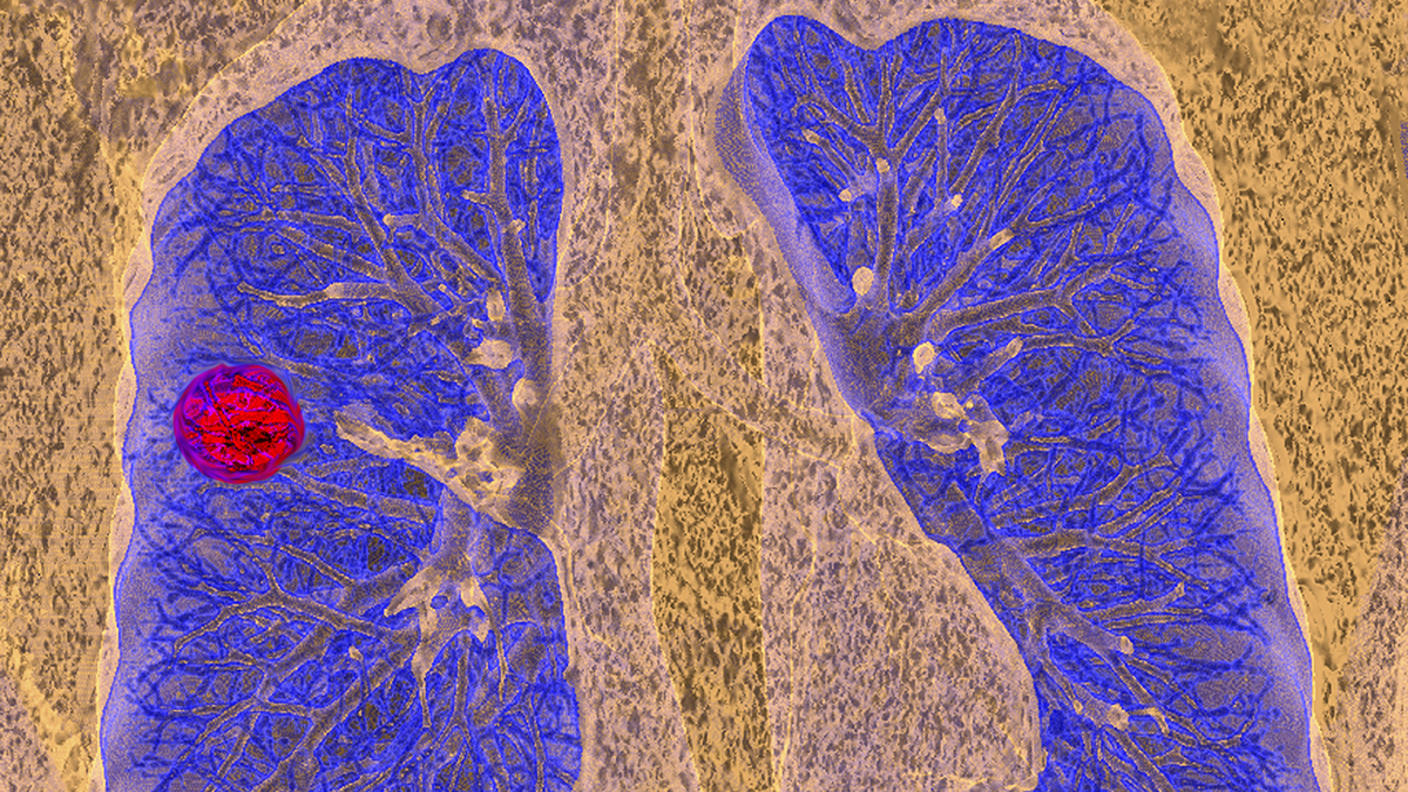
Cancer Screening
Checking for cancer (or for abnormal cells that may become cancer) in people who have no symptoms is called screening. Several screening tests have been shown to detect cancer early and to reduce the chance of dying from that cancer.
Resources
-
 Cancer Screening Overview (PDQ®)
Cancer Screening Overview (PDQ®)Cancer screening means looking for cancer before symptoms appear, when cancer may be easier to treat. Learn about different screening tests and the possible benefits and harms of using them.
-
 Screening Tests
Screening TestsLearn about cancer screening and the types of tests used to find cancer.
-
 Screening Research
Screening ResearchFind research articles on cancer screening, which may include news stories, clinical trials, blog posts, and descriptions of active studies.