Nausea and Vomiting
What Are Nausea and Vomiting?
Nausea is discomfort in your stomach and the unpleasant feeling that you might vomit. Vomiting is when you throw up what is inside your stomach. Nausea and vomiting are common and can be caused by a brain or spine tumor, pain, cancer treatment, or medications used to treat side effects.
Ways to Manage Nausea and Vomiting
There are many ways you can manage nausea and vomiting:
- Keep a daily log of your nausea and vomiting and what you are doing to manage these symptoms using the My STORITM app or a journal. Write down your nausea and vomiting symptoms so you can determine when you feel your best. Try to plan activities during the times you feel your best.
- Ask your health care provider what medication or supplements are appropriate for you to reduce your nausea or vomiting. These medications may be prescribed ‘as needed,’ so ask when and how to take this medication. Some medications for nausea and vomiting may make you feel sleepy.
- Explore self-care activities that can help you cope with and improve nausea and vomiting, including diet, exercise, and sleep:
- Ask your doctor about getting a referral to see a registered dietician to help you manage your nausea and vomiting.
- Eat a well-balanced diet to give yourself the key nutrients your body needs to strengthen your immune system and give you energy. When your nausea and vomiting stop, you can go back to your regular diet—but start slowly as your body may not be able to accept it.
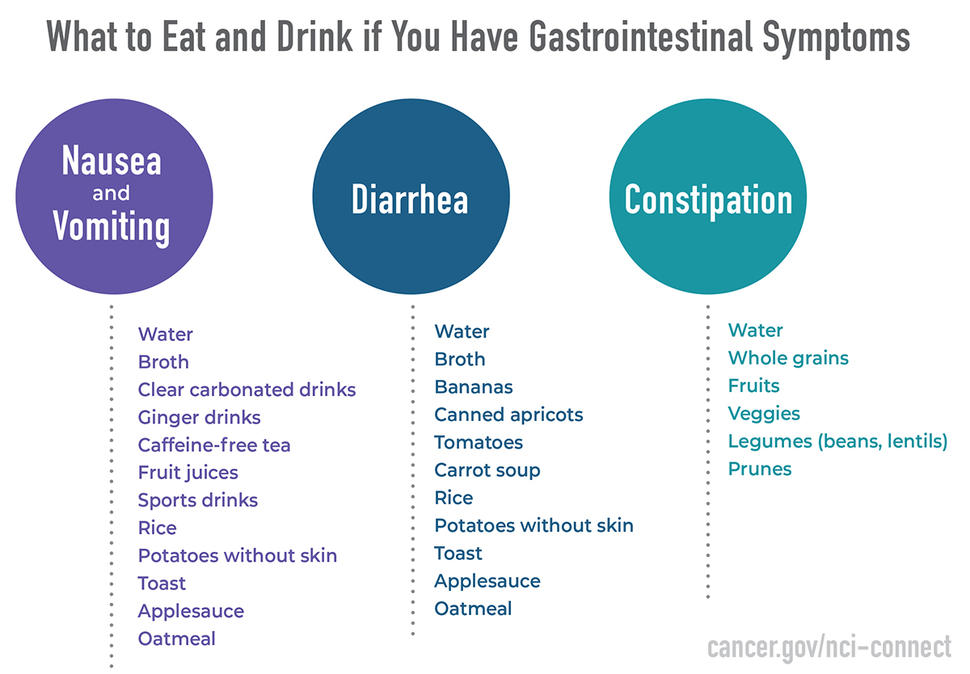
- Stay hydrated by drinking plenty of water or other liquids and take frequent, small sips throughout the day. You can try ginger drinks (ginger ale or ginger tea); broths; clear, carbonated beverages; caffeine-free tea; fruit juices (apple, cranberry, or grape); or sports drinks for minerals and electrolytes.
- Eat low-fiber foods, such as rice, potatoes without the skin, toast, applesauce, and oatmeal. Avoid foods that may upset your stomach, such as greasy or spicy foods. Try to eat six small meals throughout the day.
- Try to drink or eat a small amount of bland food (such as crackers) before trying to take medications, if you’re nauseated in the morning.
- Exercise may be difficult if you are experiencing nausea and vomiting. Avoid strenuous activity. Get up and move every few hours and ask for help if you feel dizzy or unsteady. Fresh air can help relieve nausea, so try going for a walk outside if you feel up to it.
- Try relaxation techniques, including breathing exercises, meditation, or tensing and relaxing your muscles.
- Try to reduce or manage your stress and anxiety through guided imagery, acupuncture, or therapy.
When to Report Nausea and Vomiting
Discuss any concerns with your doctor. Share the symptoms you’ve logged and your self-care activities.
- Ask your doctor when and how to report your symptoms.
- Report if your nausea and vomiting get worse, your symptoms are severe, or your symptoms do not improve with your self-care activities.
- Ask your doctor what you should do in case of an emergency, and when your nausea and vomiting should be reported immediately. Symptoms may include being unable to drink liquids or take your medications in a 24-hour period, or if your medication does not relieve your nausea or vomiting.
Diarrhea
What Is Diarrhea?
Diarrhea is when you have frequent or uncontrollable bowel movements that may be soft, loose, or watery. Diarrhea is a common symptom and can be caused by a brain tumor, cancer treatment, or medications used to treat side effects.
Diarrhea may include the following symptoms:
- Abdominal pain and cramping
- Abnormal increase in the quantity or frequency of stool
- Loose, watery stools three or more time a day
- Inability to control stools
- Signs of infection, including fever combined with dizziness
- Signs of dehydration, including thirst, weakness, heart palpitations, decreased urine output, sunken eyes, or dizziness
Ways to Manage Diarrhea
There are many ways you can cope with and manage diarrhea:
- Keep a daily log of your diarrhea and what you are doing to manage it using the My STORITM app or a journal.
- Gently wipe and clean your rectal area with mild soap and water or wet wipes after each stool.
- Apply a soothing topical agent to your rectum or take a warm bath to soothe skin irritation.
- Ask your health care provider about possible referrals to a registered dietician to help you manage diarrhea.
- Explore self-care activities that can help you cope with and improve diarrhea, including diet, exercise, and sleep:
- It may be difficult to exercise when you have diarrhea. If you’re spending time in bed, try to get up and walk around or do exercises on the side of the bed to increase blood flow and avoid stiffness.
- Scheduling uninterrupted bathroom time before bed or when you wake up may help with diarrhea. Also avoid drinks before bed. This can reduce the number of times you get up at night to go to the bathroom.
- Follow the diet your doctor recommends to reduce your diarrhea.
- Drink plenty of fluids to replace lost water (aim for at least 64 oz every day).
- Try to eat five or six small, frequent meals each day.
- Eat food and drink liquids that are high in sodium and potassium, such as broth, bananas, canned apricots, tomatoes, and soup (carrot soup sooths the bowels and increases appetite).
- Eat low-fiber foods, such as rice, potatoes without skin, toast, applesauce, and oatmeal.
- Avoid foods that can make diarrhea worse:
- Food or drinks containing alcohol or caffeine
- Dairy products (milk, cheese, and ice cream)
- Fatty, greasy, or spicy foods
- Drinks and foods containing fructose
- Fruits (apples, peaches, and pears)
- Cold food
- Diet drinks, sugarless gum, and candies containing artificial sweeteners
When to Report Diarrhea
Discuss any concerns with your doctor. Share the symptoms you’ve logged and your self-care activities.
- Ask your health care provider when and how to report your symptoms.
- Report if your diarrhea gets worse, is severe (e.g., increased frequency or inability to control), or does not improve with your self-care activities.
- Ask your doctor what you should do in case of an emergency and when your diarrhea should be reported immediately. Symptoms may include diarrhea that lasts more than 24 hours; dark yellow urine; absence of urine production; nausea and vomiting that accompanies diarrhea; dizziness; rectal bleeding; a temperature above 100.4 ̊F; swollen or painful abdomen; red, scaly, or broken rectal skin.
Constipation
What Is Constipation?
Constipation means it is difficult or painful to have a bowel movement. You may also feel bloated or uncomfortable. Constipation can be caused by a brain tumor, cancer treatment, or medications used to treat side effects.
Constipation may include the following symptoms:
- Less frequent bowel movements
- Dry or hard stools
- Abdominal pain or swelling
- Vomiting
- Anal pain or tenderness
- Inability to pass gas
Ways to Manage Constipation
There are many ways you can cope with and manage your constipation:
- Keep a daily log of your constipation and what you are doing to manage it using the My STORITM app or a journal.
- Try to have a bowel movement at the same time every day.
- Go the bathroom when you feel the urge.
- Schedule uninterrupted bathroom time before bed or when you wake up.
- Massage your abdomen to help stimulate the bowels.
- Explore self-care activities that can help you cope with and improve constipation, including diet, exercise, and sleep:
- Ask your doctor about getting a referral to see a registered dietician to help you manage constipation.
- Limit processed foods, which are pre-packaged and contain added sugars and fat.
- Eat high-fiber foods, such as whole grains, fruits, vegetables, and legumes (lentils, beans, and chickpeas). Prunes or prune juice before bed may help promote a bowel movement the next morning.
- Eat six small meals throughout the day.
- Avoid alcohol and sugary drinks. Drink plenty of water to stay hydrated (aim for eight cups a day). Drinking hot liquids 30 minutes before a bowel movement can help relieve constipation.
- Try to be active each day to prevent or relieve constipation during or after cancer treatment. Regular physical activity, including diaphragmatic abdominal exercise, can help to build abdominal muscles and aid constipation.
When to Report Constipation
Discuss any concerns with your doctor. Share the symptoms you’ve logged and your self-care activities.
- Ask your doctor when and how to report your symptoms.
- Report if your constipation gets worse, is severe (e.g., increased discomfort or inability to pass gas), or does not improve with your self-care activities.
- Ask your provider what you should do in case of an emergency and when your constipation should be reported immediately. Symptoms may include severe abdominal pain, cramping, swelling, vomiting, temperature above 100.4 ̊F, or black or bloody stool.
Other GI Symptoms
You may experience other GI symptoms in association with the more common symptoms listed above. If you have any of the symptoms below, talk to your doctor.
- Abdominal pain: pain or discomfort between your chest and hips, which includes your pancreas, stomach, intestines, liver, gallbladder, and other organs.
- Incontinence: the inability to control the flow of urine from your bladder or the escape of stool from the bowels.
- Dry mouth: an unusually dry mouth, which can be caused by dehydration or as a side effect from a medication.