Genetic Ablation of KRAS in Pancreas Cancer: When an Essential Oncogene Isn’t
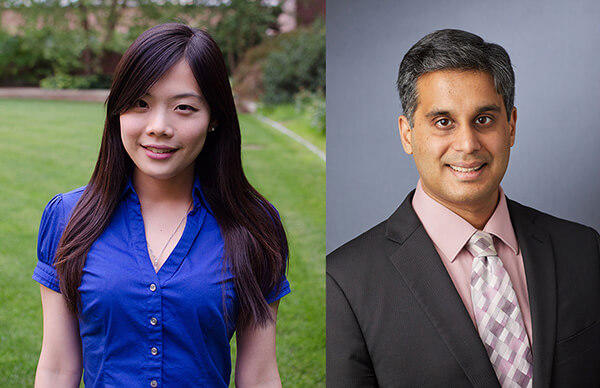
, by Pan-Yu Chen and Mandar Deepak Muzumdar
Pancreatic ductal adenocarcinoma (PDAC) is the third leading cause of cancer death in the United States, and more effective therapies are urgently needed. Genomic studies have identified KRAS mutations as a hallmark of PDAC, occurring in >90% of patient tumors. In contrast to its well-established role in tumor initiation in mouse genetic models1,2, the absolute requirement of oncogenic KRAS for PDAC maintenance in human patients has been a longstanding question in the field. Successful clinical deployment of novel KRAS-targeted therapies now in development requires a deeper understanding of whether PDAC cells exhibit KRAS oncogene addiction as well as resistance mechanisms that may arise when KRAS signaling output is inhibited.
Given the present limited availability of pharmacological inhibitors of KRAS protein, genetic tools have been widely employed to evaluate the requirement for persistent KRAS expression for PDAC maintenance. RNA interference (RNAi)-mediated knockdown of KRAS induced apoptosis in some human PDAC cell lines but not in others3–5. This variable apoptotic response led to the classification of some PDAC cells as “KRAS-dependent” and others as “KRAS-independent”4,5. These studies provided early evidence that persistent oncogenic KRAS expression may not be crucial for survival despite its role as a hallmark genetic feature of human PDAC. However, it was unclear whether the “KRAS-independent” phenotype was a consequence of residual KRAS protein expression sustaining cell proliferation and survival.
More recent evidence for PDAC cell survival in the absence of oncogenic Kras expression has emerged from studies of doxycycline-regulatable oncogenic Kras transgenic mouse models6–9. In these models, oncogenic Kras expression in the pancreas initiated tumorigenesis, while withdrawal of transgene expression resulted in tumor regression7–9. Interestingly, some PDAC tumor cells lacking Kras transgene expression survived and exhibited amplification and over-expression of YAP17,10, enhanced oxidative phosphorylation11, or autocrine IGF1 signaling9 as different mechanisms of escape from Kras dependence. While these studies provided important insights into the role of Kras in PDAC maintenance as well as possible bypass mechanisms following ablation of oncogenic Kras, withdrawal of transgene expression may have differential effects from the loss of endogenous oncogene expression.
To interrogate the essentiality of endogenous KRAS for PDAC maintenance, we utilized CRISPR/Cas to induce loss-of-function KRAS mutations in PDAC cell lines12. Although complete KRAS loss significantly impaired PDAC cell fitness in vitro and in vivo, endogenous KRAS was surprisingly dispensable in a subset (~50%) of primary and established human and mouse KRAS mutant PDAC cell lines. We further uncovered a selective vulnerability of nearly all KRAS knockout cells to PI3K inhibition, implicating PI3K blockade as a viable therapeutic strategy to circumvent resistance. Interestingly, PI3K transitioned to an upstream regulator of wild-type (H- and/or N-) RAS-MAPK signaling axis when oncogenic KRAS was inactivated, consistent with the default signaling pathway observed in KRAS wild-type PDAC cells and normal cells12,13.
Taken together, diverse genetic approaches have converged to support a universal role of persistent oncogenic KRAS expression in supporting PDAC cell proliferation and survival. These data provide strong evidence that PDAC cells are largely dependent on mutant KRAS for maximal fitness. Indeed, recent results using the siREN platform have confirmed nearly all human PDAC cell lines demonstrated a quantifiable effect of KRAS knockdown on proliferation, which contrasts with cell lines derived from KRAS mutant lung and colorectal tumors14. Nonetheless, a subset of PDAC cells is capable of escaping KRAS oncogene addiction through genetic and non-genetic mechanisms, suggesting that combined inhibition of both oncogenic KRAS output and potential resistance mechanisms is likely required to achieve durable therapeutic responses. This is consistent with the clinical experience with small molecule kinase inhibitors to date, in which long-term efficacy is almost invariably limited in advanced cancers as resistance to single agent therapies emerges.
The genetic models described here have been invaluable not only for revealing variable dependence of PDAC cells on KRAS but also for predicting resistance to KRAS inhibition. Due to potential target-independent effects of RNAi and CRISPR/Cas (e.g. off-target knockdown or mutagenesis, altered microRNA regulation resulting from changes in target RNA levels), the validity of these studies awaits confirmation with pharmacological inhibitors. In addition, several questions regarding KRAS oncogene dependency remain unresolved:
- The variability in the degree of anti-tumor responses to genetic ablation of KRAS suggests that biomarkers predicting the sensitivity of individual patient tumors to KRAS inhibition are sorely needed for effective therapeutic translation. Early work demonstrated that high KRAS protein levels and mesenchymal-like gene-expression profiles could be predictive of decreased sensitivity to KRAS knockdown4,5, which was later confirmed with CRISPR/Cas-based KRAS ablation12.Together, these data indicate that human tumors harboring gene expression profiles consistent with the quasi-mesenchymal5, basal15, and squamous16 subtypes, which largely overlap12, are likely to be the least sensitive to KRAS inhibition. While expansion of unbiased sequence-based approaches may make screening for these subtypes more readily available, specific biomarkers amenable to immunohistochemical analysis, which are currently lacking, would greatly facilitate clinical adoption of new KRAS therapeutics.
- Given the diversity of resistance mechanisms observed in PDAC cells subjected to KRAS inactivation7,9,10,12, additional predictive biomarkers for the efficacy of combination therapies to preemptively circumvent resistance would be invaluable. Interestingly, nearly all PDAC cells surviving KRAS knockout appear susceptible to PI3K inhibition, likely due to the fact that PI3K regulates both key cancer maintenance pathways, MAPK and AKT, when oncogenic KRAS is lost. However, administering adequate doses of both MAPK and PI3K inhibitors proved challenging in clinical trials due to adverse effects. Thus, it is unclear whether non-selective KRAS inhibitors in combination with PI3K inhibitors would be tolerated. New approaches to develop allele-specific KRAS inhibitors17,18 may alleviate some toxicity concerns. Unfortunately, while the allele-specific inhibitors for the G12C mutant variant are the most mature, KRAS G12C mutations are infrequently observed in PDAC (2-3%). As a result, allele-specific approaches targeting the much more prevalent codon 12 mutations (G12D, G12V, and G12R)19 are critical.
- Since a subset of PDAC cells survive despite loss of oncogenic KRAS expression, the potential that KRAS inhibitors may alter the fitness of these surviving cells must be considered. Adaptive responses have been observed following treatment of cancer cell lines with targeted inhibitors20,21, supporting the merit of including drug holidays in treatment regimens. Indeed, we have recently demonstrated that Kras mutant PDAC cells exhibit adaptive and reversible resistance to Kras knockdown22. Importantly, PDAC cells subjected to KRAS knockout unmasked the expression of metastasis-related genes and displayed gene expression signatures associated with circulating tumor cells (CTC) from a Kras mutant mouse model of PDAC23 and the quasi-mesenchymal, basal, and squamous human tumor subtypes associated with worse prognosis12. Furthermore, expression of oncogenic KRAS in various cell and animal models appears to repress genes associated with CTCs12. Collectively, these data suggest that KRAS may regulate a balance between proliferation and metastasis, as observed with Runx3 expression in the KPC mouse model24. Since PDAC metastases appear to be driven by epigenetic rather than genetic factors25–27, KRAS signaling output may be a key factor. Thus inhibiting KRAS, while offering a potent anti-proliferative effect, may also promote a more metastatic phenotype. This further emphasizes the importance of predicting resistance mechanisms and using combination therapies at the start of treatment to circumvent resistance.
Despite these gaps in knowledge, advances in genetic and pharmacological tools to manipulate KRAS function in PDAC cells have provided the opportunity to study KRAS dependency in great detail. Moreover, lessons learned from studies in PDAC could inform approaches to targeting KRAS in other cancers. As KRAS is the most frequently mutated oncogene and activating mutations of KRAS are observed at high frequency in the three leading causes of cancer death (lung, colon, and pancreas), successful clinical development of pharmacological KRAS inhibitors and predictive knowledge of dependency, response, and resistance will be instrumental in improving cancer care.
The authors
Pan-Yu Chen is a postdoc in Kevin Shannon’s laboratory at the University of California, San Francisco. Mandar Deepak Muzumdar is Assistant Professor of Genetics and a member of the Cancer Biology Institute at the Yale University School of Medicine. Dr. Chen and Dr. Muzumdar trained with Tyler Jacks at the Koch Institute for Integrative Cancer Research at the Massachusetts Institute of Technology.