Examples of Cancer Disparities
Although cancer incidence and mortality overall are declining in all population groups in the United States, some groups continue to be at increased risk of developing or dying from certain cancers.
Statistics from NCI’s Surveillance, Epidemiology, and End Results Program include information specific to racial and ethnic groups as well as populations defined by age, gender, and geography. Some key cancer incidence and mortality disparities in the United States include:
- Black/African American people have higher death rates than all other racial/ethnic groups for many, although not all, cancer types.
- Despite having slightly lower incidence rates of breast cancer than those of White women, Black/African American women are more likely than White women to die of the disease.
- The incidence rates of colorectal, lung, and cervical cancers are much higher in people who live in rural Appalachia than in those who live in urban areas in the region.
- Although deaths from prostate cancer have dropped substantially in recent decades among all men, Black/African American men are more than twice as likely as White men to die of prostate cancer and continue to have the highest prostate cancer mortality rates among all US racial/ethnic groups.
- People with more education are less likely to die prematurely (before the age of 65) from colorectal cancer than those with less education, regardless of race or ethnicity.
- Hispanic/Latino, Black/African American, and American Indian/Alaska Native women have higher incidence rates of cervical cancer than women of other racial/ethnic groups, with Black/African American women having the highest rates of death from the disease.
- American Indians/Alaska Natives have higher death rates from kidney cancer than any other racial/ethnic group.
- The rates of smoking and alcohol drinking, which increase cancer risk, are higher among lesbian, gay, and bisexual youths than among heterosexual youths.
- American Indians/Alaska Natives have the highest incidence and mortality rates of liver and intrahepatic bile duct cancer, followed by Hispanics/Latinos and Asians/Pacific Islanders.
Contributing Factors
Cancer disparities reflect the interplay among many factors, including social determinants of health, behavior, biology, and genetics—all of which can have profound effects on health, including cancer risk and outcomes.
Social Determinants of Health
The Department of Health and Human Services defines social determinants of health as the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect health, functioning, and quality of life.
Certain groups in the United States experience cancer disparities because they are more likely to encounter obstacles in getting health care.
For example, people with low incomes, low health literacy, or long travel distances to screening or treatment sites, or who lack health insurance, transportation to a medical facility, or paid medical leave are less likely to have recommended cancer screening tests and to be treated according to guidelines than those who don’t encounter these obstacles.
People who do not have reliable access to health care are also more likely to be diagnosed with late-stage cancer that might have been treated more effectively if it had been diagnosed at an earlier stage.
Some groups are disproportionately affected by cancer due to environmental conditions. People who live in communities that lack clean water or air may be exposed to cancer-causing substances.
The built environment can also influence behaviors that raise one’s risk of cancer. For example, people who live in neighborhoods that lack affordable healthy foods or safe areas for exercise are more likely to have poor diets, be physically inactive, and obese, all of which are risk factors for cancer.
Even people of higher socioeconomic status and those with health insurance may experience cancer disparities. The disparities these individuals experience may reflect the health impact of institutional racism and the chronic stress it causes, conscious or unconscious bias from health providers, mistrust of the health care system, or fatalistic attitudes about cancer.
In some cases, inherited factors or tumor biological factors may, either directly or by interacting with factors such as diet, chronic stress, or tobacco exposure, lead to cancer disparities.
For example, some evidence suggests that there are differences in the genetics, tumor biology, and immune environment of several cancers that arise in Black/African Americans compared with those that arise in people of other racial/ethnic groups. These differences may contribute to disparities in incidence, cancer growth rate, and response to treatment of these cancers.
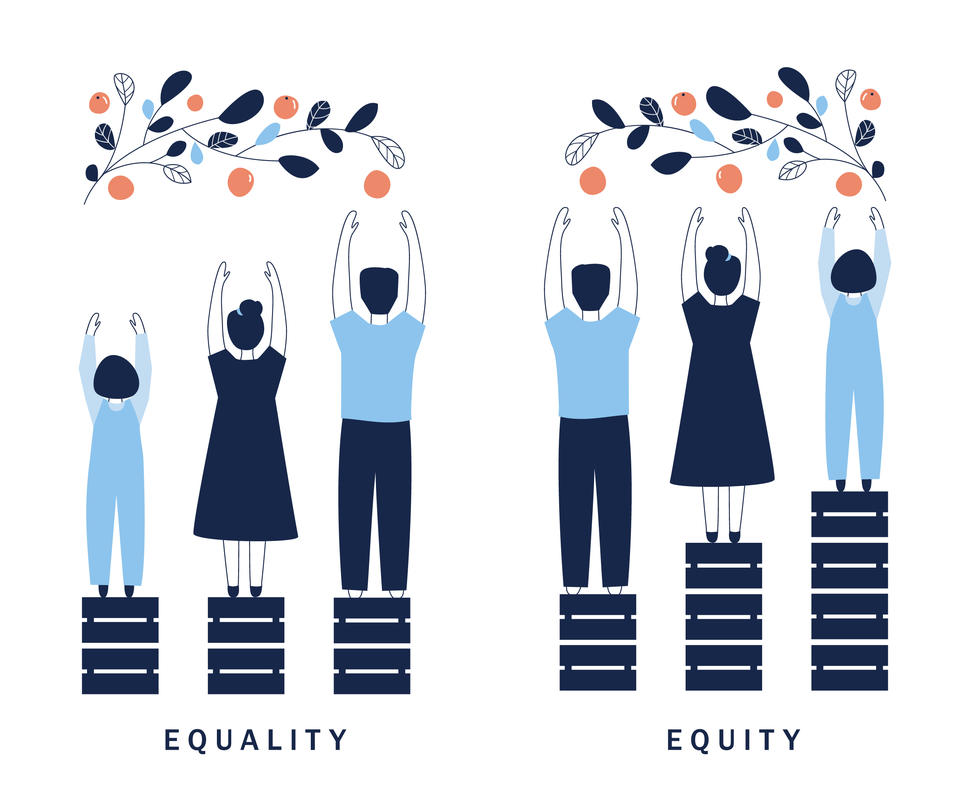
Health Equity
According to the Centers for Disease Control and Prevention, health equity is achieved when every person has the opportunity to attain his or her full health potential and no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances.
Cancer disparities may also be exacerbated by the lack of diversity in clinical research participation. Because of this lack of diversity, research results may not be applicable to all populations.
Because many different factors can influence cancer disparities, addressing them is not simple or straightforward. Reducing or eliminating some cancer disparities in the pursuit of health equity will require policy changes to overcome systemic social, racial, and institutional inequalities.
NCI-funded researchers are working to identify other ways to improve outcomes for groups disproportionately affected by cancer. Their research efforts range from designing and implementing culturally appropriate health interventions, to improving access to care and connecting underrepresented populations to clinical trials, to examining biological and genetic factors that may explain differences in rates of fast-growing cancers.