Imaging tests to diagnose breast cancer
- A diagnostic mammogram is an x-ray picture of the breast that checks for breast cancer. It is used after a lump or other symptom of the disease has been found. It is also used to follow up on breast changes found during a screening mammogram. A diagnostic mammogram often involves taking more detailed x-ray pictures of the breast from different angles to check the abnormal area more closely.
- Breast ultrasound is a procedure that uses high-energy sound waves to make pictures of the inside of the breast.
- Breast MRI uses a powerful magnet, radio waves, and a computer to take detailed pictures of areas inside the breast.
Biopsy for breast cancer
You may have a biopsy if imaging tests find a lump or other abnormal area in the breast. In a biopsy, a surgeon removes cells or tissue so a pathologist can study them under a microscope. A biopsy is the only sure way to diagnose breast cancer.
The following types of biopsies may be used to check for breast cancer:
- Fine-needle aspiration biopsy uses a thin needle to remove tissue or fluid.
- Core-needle biopsy uses a wider needle to remove tissue samples, sometimes called cores. A small metal clip may be placed in the biopsy area to mark the spot for any future procedures.
- Image-guided biopsy is sometimes used for fine-needle aspiration biopsies and often used for core-needle biopsies. In this type of biopsy, ultrasound, mammography, or MRI are used to guide the needle to the area where the tissue needs to be checked. It is often used when the abnormal area is deep inside the breast or when the doctor cannot feel a lump or mass. When mammography is used to guide the needle, the procedure may be called a stereotactic biopsy.
- Surgical biopsy is the use of surgery to remove some or all of a lump or abnormal area. There are two types of surgical biopsies:
- Incisional biopsy removes part of a lump or a sample of tissue.
- Excisional biopsy removes an entire lump. A small amount of healthy tissue around the lump may also be removed.
You will usually have a biopsy as an outpatient, meaning you will likely go home the same day as the procedure. Whether you will need anesthesia and how long it will take you to recover from a breast biopsy depend on whether it involves surgery. Nonsurgical biopsies (fine-needle or core biopsies) usually do not require anesthesia. Surgical biopsies are done with local or general anesthesia. Recovery takes longer after a surgical biopsy. Talk with your doctor about what to expect during and after your biopsy.
The pathologist will study the biopsy sample and provide the results of their analysis in a pathology report. If the pathologist finds that you have cancer, the pathology report will help you and your doctor understand your cancer and treatment options. The report will include information about:
- where in the breast the cancer started, such as the ducts or lobes
- the tumor grade
- whether the cancer has spread to nearby normal tissue (called invasive breast cancer)
Learn more about the kind of information that can be found in Pathology Reports.
If the biopsy shows breast cancer, the cells will be tested for biomarkers. Learn more about Tests for Breast Cancer Biomarkers.
Tests to stage breast cancer
If you are diagnosed with breast cancer, your doctor will perform more tests to find out if the cancer has spread and if so, how far. Sometimes the cancer is only in the breast. Or, it may have spread from the breast to the lymph nodes or other parts of the body. The process of learning how far the cancer has spread is called staging.
For breast cancer, stages are defined according to many factors, including extent of spread, results of biomarker tests, tumor grade, and, in some cases, multigene tests. It is important to know the stage of breast cancer to plan treatment.
The following tests and procedures may be used find out your breast cancer stage:
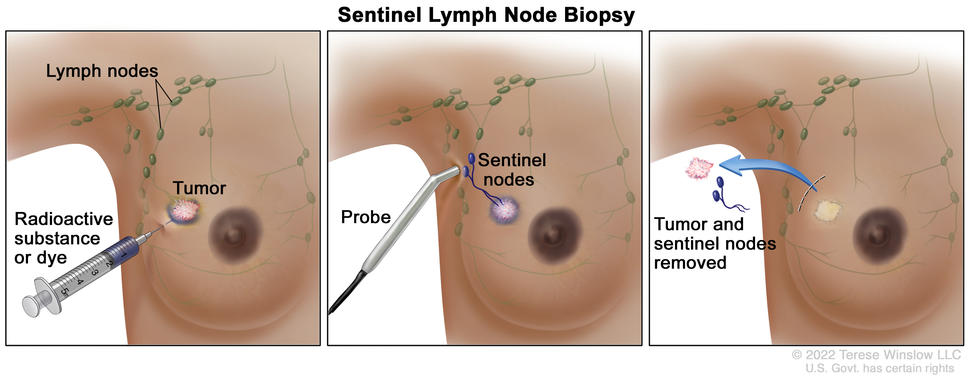
Sentinel lymph node biopsy
Breast cancer may spread to nearby lymph nodes, such as those in the underarm area. A sentinel lymph node biopsy can help doctors tell if cancer cells have spread beyond the breast. A sentinel lymph node is the first lymph node to which cancer cells are most likely to spread from the primary tumor. Sometimes, there can be more than one sentinel lymph node.
To locate the sentinel lymph node, a radioactive substance, a blue dye, or both will be injected near the tumor. The surgeon then uses a device to detect lymph nodes that contain the radioactive substance, or they look for lymph nodes that are stained with the blue dye. Once the surgeon locates the sentinel lymph node, they make a small incision in the skin and remove the node.
A pathologist then checks the sentinel node for cancer cells. If cancer is found, the surgeon may remove other lymph nodes, either during the same biopsy procedure or during a follow-up surgery. A sentinel lymph node biopsy is an outpatient procedure done under general anesthesia.
Imaging tests to stage breast cancer
The following imaging tests may be done to find out if breast cancer has spread:
A CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
A bone scan checks if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the areas of the bones with cancer and is detected by a scanner.
A PET scan (positron emission tomography scan) uses a small amount of radioactive sugar (also called radioactive glucose) that is injected into a vein. The PET scanner rotates around the body and makes pictures of where sugar is being used by the body. Cancer cells show up brighter in the pictures because they are more active and take up more sugar than normal cells do. When this procedure is done at the same time as a CT scan, it is called a PET-CT scan.
Biomarker tests for breast cancer
All breast cancers are tested for the presence of certain biomarkers, such as hormone receptors (estrogen receptors and progesterone receptors) and HER2. This information is needed to identify the stage of the breast cancer and to plan treatment. Learn more about these tests at Tests for Breast Cancer Biomarkers.
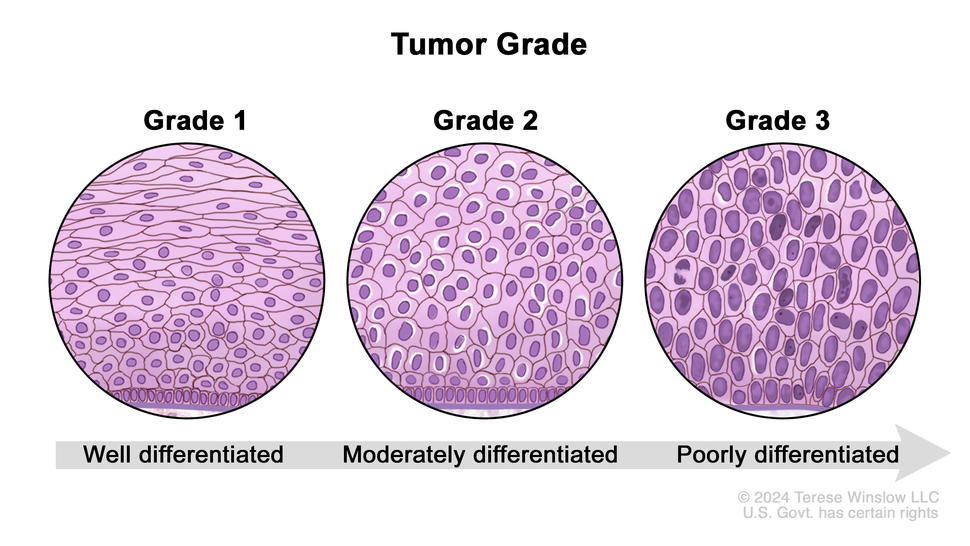
Breast cancer tumor grade
Tumor grade describes how abnormal the cancer cells and tissue look under a microscope and how quickly the cancer cells are likely to grow and spread. The pathologist assigns a score of 1 to 3 to the cells or tissue. A score of 1 means the cells and tumor tissue look the most normal and are less likely to spread. A score of 3 means the cells and tissue look the most abnormal and are more likely to grow fast and spread. Learn more about the breast cancer grading system at Breast Cancer Stages.
Multigene tests to predict risk of recurrence
Multigene tests, also called genomic tests, are lab tests that look at the activity of genes in your breast cancer cells. These tests may help predict the chances that cancer will spread to other parts of the body or come back. And they can help you and your doctor make decisions about treatment.
The tests listed below are often done on a sample of the tumor that was removed during the biopsy or surgery. Most people won’t need another procedure for these tests.
There are many types of multigene tests. Examples of tests you might have include:
- Oncotype DX looks at the activity of 21 genes in people with early-stage breast cancer that is ER positive, HER2 negative, and has not spread to the lymph nodes or has spread to no more than three lymph nodes. The test helps predict whether breast cancer will spread to other parts of the body. If the risk of the cancer spreading is high, you may have chemotherapy to lower that risk.
- MammaPrint looks at the activity of 70 genes in the breast cancer tissue of people with early-stage breast cancer that has not spread to the lymph nodes or has spread to no more than three lymph nodes. The test helps predict whether breast cancer will spread to other parts of the body or come back after treatment. If the test shows that the risk of the cancer spreading or returning is high, you may have chemotherapy to lower that risk.
- Breast Cancer Index looks at the activity of 11 genes in the breast cancer tissue of people with early-stage, HR-positive breast cancer that has not spread to the lymph nodes or has spread to no more than three lymph nodes. The test helps predict the risk that your breast cancer will come back within 5 to 10 years after diagnosis. If the test shows that the risk of the cancer coming back is high, you may receive 5 more years of hormone therapy to help lower that risk.
Other types of multigene tests are available. Ask your doctor if multigene tests might be right for you and how the results might affect your treatment plan.
Genetic counseling and testing
Your doctor might suggest genetic testing as part of diagnosing your breast cancer. Genetic testing can be done on a sample of your blood, saliva, or from a swab of inside your cheek. Genetic test results show if you were born with a change in the BRCA1, BRCA2, or another breast cancer risk gene. Knowing if you have a specific genetic change may help your doctor suggest the best treatment for your cancer. These gene changes are sometimes called mutations or pathogenic variants.
Genetic counseling before genetic testing can help you understand your chances of having a gene change that caused your breast cancer and whether genetic testing is needed. For example, genetic testing might be advised if you:
- have a known family history of a change in BRCA1, BRCA2, or another breast cancer risk gene
- were diagnosed with breast cancer before age 50
- were diagnosed with two or more primary breast cancers (in the same breast or in both breasts)
- have triple-negative breast cancer
- have lobular breast cancer with a family history of diffuse gastric cancer
- have a family history of breast cancer or certain other cancers, such as pancreatic cancer, prostate cancer, or ovarian cancer
- have male breast cancer
- are of Ashkenazi Jewish descent
Genetic counselors can also help you cope with your genetic testing results, including how to discuss the results with family members. They can advise you about whether other members of your family should receive genetic testing to find out if they are at risk of breast cancer or other cancers. Learn more about BRCA gene changes and cancer risk and genetic testing for inherited cancer risk.
Waiting for test results
Waiting for cancer test results can be stressful. Ask your doctor when the results will be ready and how you will be notified so you know how long it will be before you hear back. If you don’t hear back within the expected time, it’s okay to follow up with your doctor.
Sometimes test results are released to your online patient portal before you’ve met with your doctor. Although it can be difficult to wait to look at the test results until you are able to review them with your doctor, doing so can help avoid confusion about what the results mean.
If you need help dealing with the stress of waiting for test results, reach out to your care team. A social worker can offer support and resources to help you. Whatever the results, your doctor can help you understand next steps.
Getting a second opinion
You may want a second opinion to confirm your breast cancer diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans before giving advice. The doctor who gives the second opinion may agree with your first doctor, suggest changes or another approach, or provide more information about your cancer.
To learn more about choosing a doctor and getting a second opinion, visit Finding Cancer Care. You can contact NCI’s Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital or getting a second opinion. For questions you might want to ask at your doctor visits, visit Questions to Ask Your Doctor About Cancer.