Alcohol and Cancer Risk
What is alcohol?
Alcohol is the common term for ethanol or ethyl alcohol, a chemical substance found in alcoholic beverages such as beer, hard cider, malt liquor, wines, and distilled spirits (liquor). Alcohol is produced by the fermentation of sugars and starches by yeast. Alcohol is also found in some medicines, mouthwashes, and household products (including vanilla extract and other flavorings). This fact sheet focuses on cancer risks associated with the consumption of alcoholic beverages.
According to the National Institute on Alcohol Abuse and Alcoholism, a standard alcoholic drink in the United States contains 14.0 grams (0.6 ounces) of pure alcohol. Generally, this amount of pure alcohol is found in:
- 12 ounces of beer
- 8–10 ounces of malt liquor
- 5 ounces of wine
- 1.5 ounces, or a "shot," of 80-proof distilled spirits (liquor)
These amounts are used by public health experts in developing health guidelines about alcohol consumption and to provide a way for people to compare the amounts of alcohol they consume. However, they may not reflect the typical serving sizes people may encounter in daily life.
According to the federal government’s Dietary Guidelines for Americans, 2020–2025, individuals who do not drink alcohol should not start drinking for any reason. The Dietary Guidelines also recommends that people who drink alcohol do so in moderation by limiting consumption to 2 drinks or less in a day for men and 1 drink or less in a day for women. Heavy alcohol drinking is defined as having 4 or more drinks on any day or 8 or more drinks per week for women and 5 or more drinks on any day or 15 or more drinks per week for men.
What is the evidence that alcohol drinking can cause cancer?
There is a strong scientific consensus that alcohol drinking can cause several types of cancer (1, 2). In its Report on Carcinogens, the National Toxicology Program of the US Department of Health and Human Services lists consumption of alcoholic beverages as a known human carcinogen.
The evidence indicates that the more alcohol a person drinks—particularly the more alcohol a person drinks regularly over time—the higher his or her risk of developing an alcohol-associated cancer. Even those who have no more than one drink per day and binge drinkers (those who consume 4 or more drinks for women and 5 or more drinks for men in one sitting) have a modestly increased risk of some cancers (3–7). Based on data from 2009, an estimated 3.5% of cancer deaths in the United States (about 19,500 deaths) were alcohol related (8).
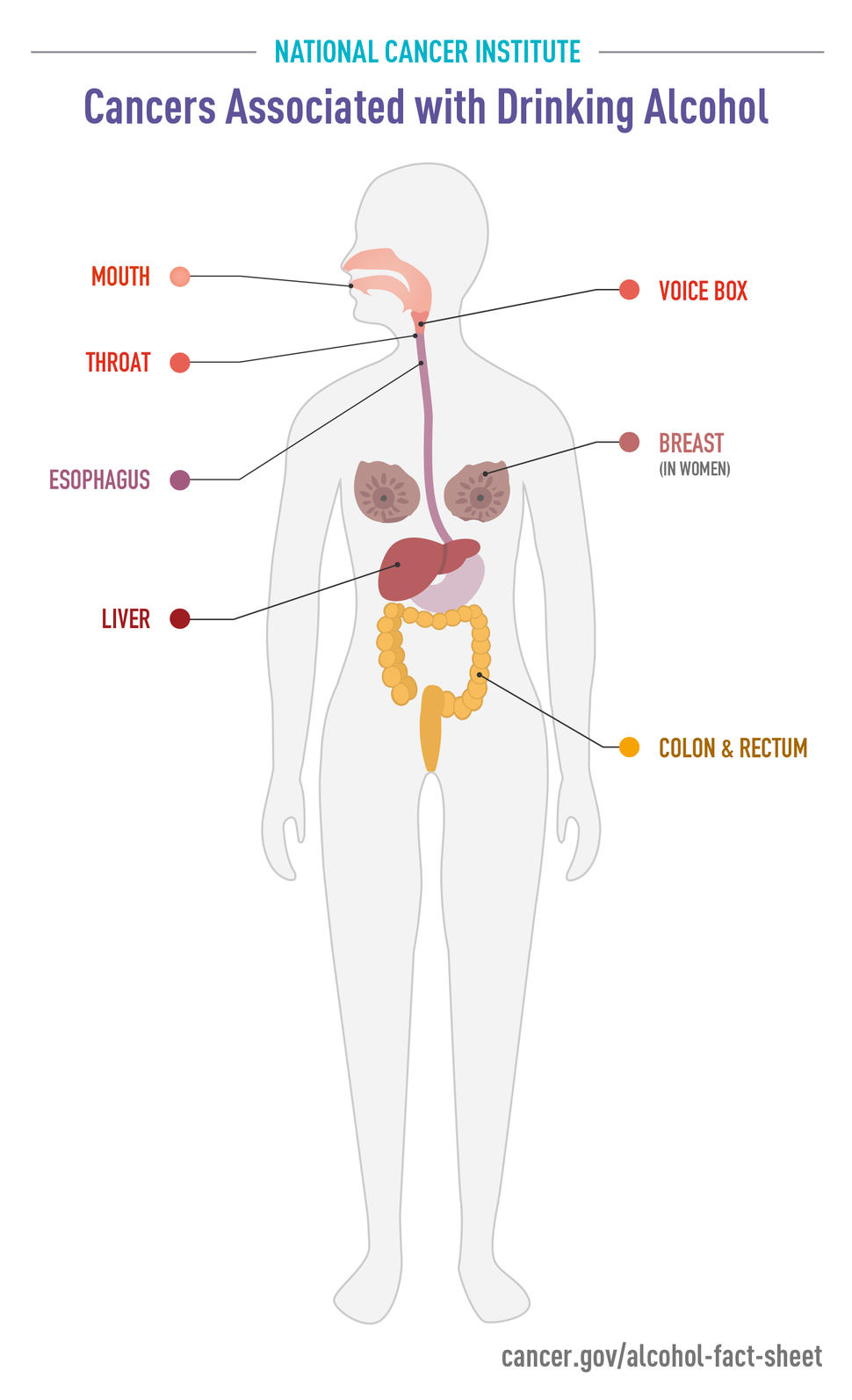
Clear patterns have emerged between alcohol consumption and the development of the following types of cancer:
- Head and neck cancer: Moderate to heavy alcohol consumption is associated with higher risks of certain head and neck cancers. Moderate drinkers have 1.8-fold higher risks of oral cavity (excluding the lips) and pharynx (throat) cancers and 1.4-fold higher risks of larynx (voice box) cancers than non-drinkers, and heavy drinkers have 5-fold higher risks of oral cavity and pharynx cancers and 2.6-fold higher risks of larynx cancers (4, 9). Moreover, the risks of these cancers are substantially higher among persons who consume this amount of alcohol and also use tobacco (10).
- Esophageal cancer: Alcohol consumption at any level is associated with an increased risk of a type of esophageal cancer called esophageal squamous cell carcinoma. The risks, compared with no alcohol consumption, range from 1.3-fold higher for light drinking to nearly 5-fold higher for heavy drinking (4, 9). In addition, people who inherit a deficiency in an enzyme that metabolizes alcohol have been found to have substantially increased risks of esophageal squamous cell carcinoma if they consume alcohol (11).
- Liver cancer: Heavy alcohol consumption is associated with approximately 2-fold increased risks of two types of liver cancer (hepatocellular carcinoma and intrahepatic cholangiocarcinoma) (4, 9, 12, 13).
- Breast cancer: Epidemiologic studies have consistently found an increased risk of breast cancer with increasing alcohol intake. Pooled data from 118 individual studies indicates that light drinkers have a slightly increased (1.04-fold higher) risk of breast cancer, compared with nondrinkers. The risk increase is greater in moderate drinkers (1.23-fold higher) and heavy drinkers (1.6-fold higher) (4, 9). An analysis of prospective data for 88,000 women participating in two US cohort studies concluded that for women who have never smoked, light to moderate drinking was associated with a 1.13-fold increased risk of alcohol-related cancers (mostly breast cancer) (5).
- Colorectal cancer: Moderate to heavy alcohol consumption is associated with 1.2- to 1.5-fold increased risks of cancers of the colon and rectum compared with no alcohol consumption (4, 9, 14).
Numerous studies have examined whether there is an association between alcohol consumption and the risk of other cancers. For cancers of the ovary, prostate, stomach, uterus, and bladder, either no association with alcohol use has been found or the evidence for an association is inconsistent. However, evidence is accumulating that alcohol consumption is associated with increased risks of melanoma and of prostate and pancreatic cancers (4, 15).
Alcohol consumption has also been associated with decreased risks of kidney cancers (16–18) and non-Hodgkin lymphoma (19, 20) in multiple studies. However, any potential benefits of alcohol consumption for reducing the risks of some cancers are likely outweighed by the harms of alcohol consumption. In fact, a recent study that included data from more than 1,000 alcohol studies and data sources, as well as death and disability records from 195 countries and territories from 1990 to 2016, concluded that the optimal number of drinks to consume per day to minimize the overall risk to health is zero (21). That study did not include data on kidney cancer or non-Hodgkin lymphoma.
Alcohol consumption may also be associated with an increased risk of second primary cancers. For example, a meta-analysis of data from 19 studies showed that among patients with cancer of the upper aerodigestive tract (UADT)—which includes the oral cavity, pharynx, larynx, and esophagus—for every 10 grams of alcohol consumed per day before the first UADT cancer diagnosis there was a 1.09-fold higher risk of a second primary UADT cancer (22). It is less clear whether alcohol consumption increases the risk of second primary cancers at other sites, such as the breast (23–25).
How does alcohol affect the risk of cancer?
Researchers have hypothesized multiple ways that alcohol may increase the risk of cancer, including
- metabolizing (breaking down) ethanol in alcoholic drinks to acetaldehyde, which is a toxic chemical and a probable human carcinogen; acetaldehyde can damage both DNA (the genetic material that makes up genes) and proteins
- generating reactive oxygen species (chemically reactive molecules that contain oxygen), which can damage DNA, proteins, and lipids (fats) in the body through a process called oxidation
- impairing the body’s ability to break down and absorb a variety of nutrients that may be associated with cancer risk, including vitamin A; nutrients in the vitamin B complex, such as folate; vitamin C; vitamin D; vitamin E; and carotenoids
- increasing blood levels of estrogen, a sex hormone linked to the risk of breast cancer
Alcoholic beverages may also contain a variety of carcinogenic contaminants that are introduced during fermentation and production, such as nitrosamines, asbestos fibers, phenols, and hydrocarbons.
The mechanisms by which alcohol consumption may decrease the risks of some cancers are not understood and may be indirect.
How does the combination of alcohol and tobacco affect cancer risk?
Epidemiologic research shows that people who use both alcohol and tobacco have much greater risks of developing cancers of the oral cavity, pharynx (throat), larynx, and esophagus than people who use either alcohol or tobacco alone. In fact, for oral and pharyngeal cancers, the risks associated with using both alcohol and tobacco are multiplicative; that is, they are greater than would be expected from adding the individual risks associated with alcohol and tobacco together (10, 26).
Can people's genes affect their risk of alcohol-related cancers?
A person’s risk of alcohol-related cancers is influenced by their genes, specifically the genes that encode enzymes involved in metabolizing (breaking down) alcohol (27).
For example, one way the body metabolizes alcohol is through the activity of an enzyme called alcohol dehydrogenase, or ADH, which converts ethanol into the carcinogenic metabolite acetaldehyde, mainly in the liver. Recent evidence suggests that acetaldehyde production also occurs in the oral cavity and may be influenced by factors such as the oral microbiome (28, 29).
Many individuals of East Asian descent carry a version of the gene for ADH that codes for a "superactive" form of the enzyme. This superactive ADH enzyme speeds the conversion of alcohol (ethanol) to toxic acetaldehyde. Among people of Japanese descent, those who have this form of ADH have a higher risk of pancreatic cancer than those with the more common form of ADH (30).
Another enzyme, called aldehyde dehydrogenase 2 (ALDH2), metabolizes toxic acetaldehyde to nontoxic substances. Some people, particularly those of East Asian descent, carry a variant of the gene for ALDH2 that encodes a defective form of the enzyme. In people who produce the defective enzyme, acetaldehyde builds up when they drink alcohol. The accumulation of acetaldehyde has such unpleasant effects (including facial flushing and heart palpitations) that most people who have inherited the ALDH2 variant are unable to consume large amounts of alcohol and therefore have a low risk of developing alcohol-related cancers.
However, some individuals with the defective form of ALDH2 can become tolerant to the unpleasant effects of acetaldehyde and consume large amounts of alcohol. Epidemiologic studies have shown that such individuals have a higher risk of alcohol-related esophageal cancer, as well as of head and neck cancers, than individuals with the fully active enzyme who drink comparable amounts of alcohol (31). These increased risks are seen only among people who carry the ALDH2 variant and drink alcohol—they are not observed in people who carry the variant but do not drink alcohol.
Can drinking red wine help prevent cancer?
The plant secondary compound resveratrol, found in grapes used to make red wine and some other plants, has been investigated for many possible health effects, including cancer prevention. However, researchers have found no association between moderate consumption of red wine and the risk of developing prostate cancer (32) or colorectal cancer (33).
What happens to cancer risk after a person stops drinking alcohol?
Most of the studies that have examined whether cancer risk declines after a person stops drinking alcohol have focused on head and neck cancers and on esophageal cancer. In general, these studies have found that stopping alcohol consumption is not associated with immediate reductions in cancer risk. The cancer risks eventually decline, although it may take years for the risks of cancer to return to those of never drinkers.
For example, ex-drinkers still had higher risks of oral cavity and pharyngeal cancers than never drinkers even 16 years after they stopped drinking alcohol, although it was lower than before they stopped drinking (34). One study estimated that it would take more than 35 years for the higher risks of laryngeal and pharyngeal cancers associated with alcohol consumption to decrease to the level of never drinkers (35).
Is it safe for someone to drink alcohol while undergoing cancer chemotherapy?
As with most questions related to a specific individual’s cancer treatment, it is best for patients to check with their health care team about whether it is safe to drink alcohol during or immediately following chemotherapy treatment. The doctors and nurses administering the treatment will be able to give specific advice about whether it is safe to consume alcohol while undergoing specific cancer treatments.