What is a mammogram?
Mammograms are x-ray images of the breasts. Mammograms are used for breast cancer screening because they can find tumors at an earlier stage, before they cause symptoms.
Mammograms can also be used to check for breast cancer after a woman or her doctor finds a lump or other change. This type of mammogram is called a diagnostic mammogram.
The same machines are used for both types of mammograms. However, diagnostic mammography requires images from more angles than screening mammography, so the dose of radiation is higher.
What can a mammogram show?
Mammograms can show a mass (breast lump), deposits of calcium (called calcifications), and other changes. They also show breast density. A radiologist will study the mammogram for unusual changes. When possible, the radiologist will compare your most recent mammogram with past mammograms to check for changes in breast tissue since your last mammogram.
Mass (also called a breast lump): The size, shape, and edges of a lump give the radiologist important information. A lump that is not cancer often looks smooth and round and has clear, defined edges. Lumps that look like this are often benign cysts. However, if the lump has a jagged outline, an irregular shape, or other unusual features, more tests may be needed.
Calcifications are deposits of calcium in the breast that are too small to be felt. There are two types, neither of which is related to calcium in your diet:
- Macrocalcifications look like small white dots on a mammogram. They are often caused by aging, an old injury, or inflammation and are usually benign.
- Microcalcifications look like white specks on a mammogram. If found in an area of rapidly dividing cells or grouped together in a certain way, they may be a sign of DCIS or breast cancer.
Breast density describes the relative amounts of dense and fatty tissue in the breasts, as seen on a mammogram. Mammography is more likely to miss cancer in women with dense breasts.
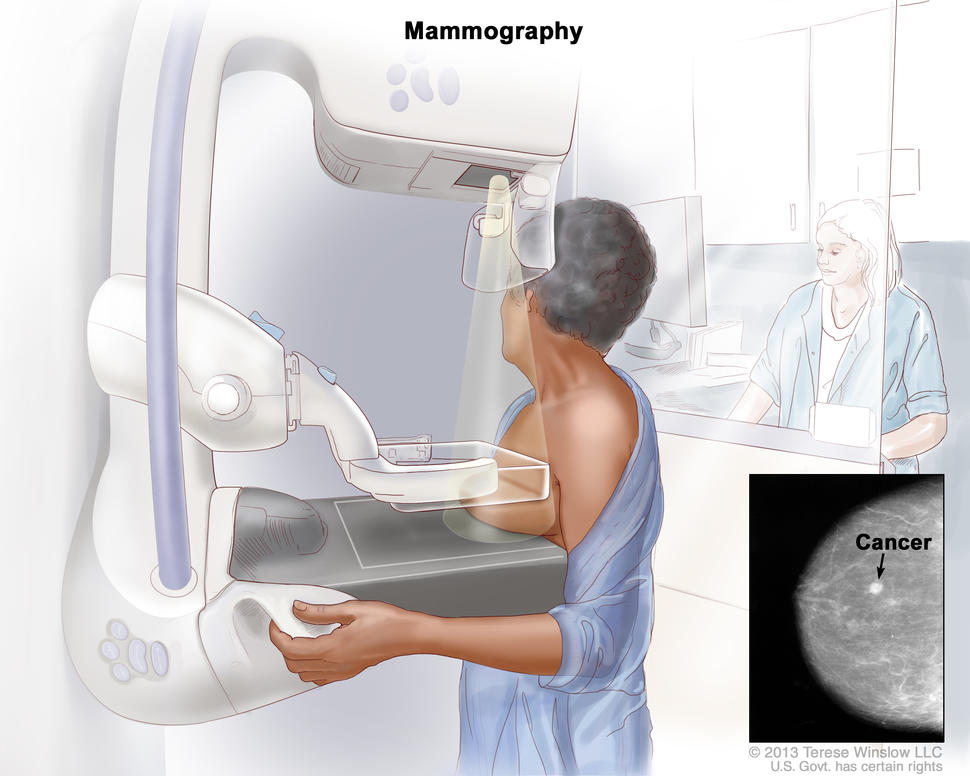
What happens during a mammogram?
During a mammogram, your breast is placed between two plates that are then pressed together. Pressing the breast helps get a better x-ray picture of the inside of your breast. Several images are taken from different angles, with the breast repositioned each time.
For some people, the compression of the breast can be painful. Taking an over-the-counter pain medication before the procedure may lessen the discomfort.
If possible, try not to schedule your mammogram right before or during your menstrual period, when your breasts may be especially tender.
You should avoid using personal care products, such as deodorants, antiperspirants, powders, lotions, creams, or perfumes, around the breasts or under the arms on the day of your mammogram.
How are mammogram results reported?
You will receive the radiologist's report of your screening mammogram within about 2 weeks, either by mail or in your electronic medical record. The results will also be sent to the health care provider who ordered the mammogram. If you don't get your results within 2 weeks, you should contact your provider.
The report of your screening mammogram will usually include the BI-RADS category. BI-RADS categories provide a consistent way for radiologists to report a range of possible mammographic findings, with the recommended follow-up.
Breast Imaging Reporting and Database System (BI-RADS)
| Category | Assessment | Follow-up |
|---|---|---|
| 0 | Need additional imaging evaluation | Additional imaging needed before a category can be assigned |
| 1 | Negative | Continue regular screening mammograms |
| 2 | Benign (noncancerous) finding | Continue regular screening mammograms |
| 3 | Probably benign | Receive a 6-month follow-up mammogram |
| 4 | Suspicious abnormality | May require biopsy |
| 5 | Highly suggestive of malignancy (cancer) | Requires biopsy |
| 6 | Known biopsy-proven malignancy (cancer) | Biopsy confirms presence of cancer before treatment begins |
The mammogram screening report also includes information on breast density.
Depending on your result, you may be called back for further imaging or a biopsy. The letter with your results will explain what follow-up exams you may need.
Although it can be scary to be called back for further testing, it is important to keep in mind that most people who are called back are not found to have breast cancer.
When and how often should I have a screening mammogram?
The U.S. Preventive Services Task Force (USPSTF) currently recommends that women at average risk of breast cancer have screening mammograms every 2 years between ages 40 and 74. Talk with your doctor to find out your risk for breast cancer, based on your personal and family health history.
Some individuals at very high risk of breast cancer may be advised to begin screening for breast cancer at a younger age and to get screened more often than those at average risk. For example, anyone who received treatment for a childhood cancer that included radiation therapy to the breast or chest may be advised to begin screening at age 25, or 8 years after finishing radiation therapy, whichever is later. People who have known harmful mutations in the BRCA1 or BRCA2 genes may also consider having earlier or more frequent screening.
What are 3D mammograms?
Three-dimensional, or 3D, mammography, also called digital breast tomosynthesis (DBT), creates three-dimensional images of the breast. To do this, the DBT machine takes multiple pictures of thin “slices” across the breast that are then assembled into a 3D picture by computer software. DBT also creates 2D images of the breast like those created by standard mammography.
DBT combined with standard mammography is better at finding tumors than standard mammography alone. However, it's still unknown whether DBT is more effective than standard mammography at reducing deaths from breast cancer. The NCI-sponsored TMIST trial is comparing 2D mammography with DBT to answer this question.
Are mammograms done in people with breast implants?
Yes. Women with breast implants should continue getting mammograms. However, most women who have breast reconstruction with implants after mastectomy usually do not need a mammogram of the reconstructed breast.
Implants can hide some breast tissue, making it harder for a radiologist to see unusual changes on the mammogram. If you have breast implants you should let the mammography facility know. A special technique called implant displacement views may be used.
Where can I get a mammogram?
Mammograms are available in breast clinics, hospital radiology departments, mobile vans, private radiology offices, and doctors' offices. You may be able to schedule your own screening mammogram directly with the mammography facility without a referral from your doctor.
The Mammography Quality Standards Act (MQSA) is a federal law that requires mammography facilities across the nation to meet uniform quality standards. MQSA regulations also require that mammography facilities give patients an easy-to-read report of their mammogram results.
If you need help finding an FDA-certified mammography facility near you, you can contact NCI's Cancer Information Service at 1–800–4–CANCER (1–800–422–6237). A searchable list is available from the FDA.
How much does a mammogram cost?
Insurance plans governed by the federal Affordable Care Act must cover screening mammograms as a preventive benefit every 1–2 years for women ages 40 and over without requiring copayments, coinsurance, or deductibles. In addition, many states require that Medicaid and public employee health plans cover screening mammography. Contact your mammography facility or health insurance company to confirm the cost and coverage.
Medicare pays for annual screening mammograms for all female Medicare beneficiaries who are age 40 or older. Information about coverage of mammograms is available from Medicare.
If you need a diagnostic mammogram, check with your health insurance provider about coverage.
How can uninsured or low-income women get a free or low-cost screening mammogram?
Some state and local health programs and employers provide mammograms free or at low cost. For example, CDC's National Breast and Cervical Cancer Early Detection Program provides screening services, including clinical breast exams and mammograms, to low-income, uninsured women throughout the United States and in several U.S. territories. Contact information for local programs is available from the CDC or by calling 1–800–CDC–INFO (1–800–232–4636).
Information about free or low-cost mammography screening programs is also available from NCI's Cancer Information Service at 1–800–4–CANCER (1–800–422–6237) and from local hospitals, health departments, women's centers, or other community groups.