An ependymoma is a primary central nervous system (CNS) tumor. This means it begins in the brain or spinal cord.
To get an accurate diagnosis, a piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.
What Are the Grades of Ependymomas?
Primary CNS tumors are graded based on a tumor tissue analysis performed by a neuropathologist. Ependymomas are grouped in three grades (grade 1, 2, or 3, also written as grade I, II, or III) based on their characteristics under a microscope and their behavior:
Grade 1 ependymomas are low-grade tumors. Subependymomas, an ependymoma subtype, are grade 1 ependymomas that can arise in the brain or the spine. Both are more common in adults than children.
Grade 2 ependymomas are also low-grade tumors. However, they are more likely to recur than grade 1 ependymomas, especially if they cannot be completely removed during surgery. These include the subtypes myxopapillary ependymoma and conventional ependymoma grade 2. Myxopapillary ependymoma typically arises in the spine and is more common in adults. Conventional grade 2 ependymoma can occur in either the brain or spine and are more frequent in adults or children depending on the molecular subtype.
Grade 3 ependymomas are malignant (cancerous). This means they are fast-growing tumors. They occur most often in the brain but can also occur in the spine.
The location and molecular features of each ependymoma subtype can predict prognosis better than grade alone. These are the main subtypes of ependymoma, according to the 2021 World Health Organization (WHO) classification:
- Supratentorial ependymoma, ZFTA fusion-positive
- Supratentorial ependymoma, YAP1 fusion-positive
- Posterior fossa group A (PFA) ependymoma
- Posterior fossa group B (PFB) ependymoma
- Spinal ependymoma
- Spinal ependymoma, MYCN amplified
- Myxopapillary ependymoma
- Subependymoma
What Do Ependymomas Look like on an MRI?
Ependymomas usually appear as one or more well-defined masses that often brighten with contrast on a magnetic resonance imaging (MRI) scan.
What Causes Ependymomas?
Cancer is a genetic disease—that is, it is caused by certain changes to genes that control the way our cells function. Genes may be mutated (changed) in many types of cancer, which can increase the growth and spread of cancer cells. The cause of ependymomas is not known. However, they can occur in people with certain genetic diseases, such as Neurofibromatosis type 2.
Where Do Ependymomas Form?
Ependymomas can form anywhere in the CNS. They often occur near the ventricles in the brain and the central canal of the spinal cord. On rare occasions, they can form outside the CNS, such as in the ovaries. Ependymomas develop from ependymal cells called radial glial cells. Ependymal cells are one of three types of glial cells that support the CNS.
Do Ependymomas Spread?
Ependymomas rarely spread outside the CNS. However, they can spread to other areas of the CNS through cerebrospinal fluid (CSF).
What Are the Symptoms of an Ependymoma?
Symptoms related to an ependymoma depend on the tumor’s location. Here are some possible symptoms that can occur.
People with an ependymoma in the brain may have:
- Headaches
- Nausea
- Vomiting
- Dizziness
People with an ependymoma in the spine may have:
- Back pain
- Numbness and weakness in their arms, legs, or trunk
- Sexual, urinary, or bowel problems
Who Is Diagnosed with an Ependymoma?
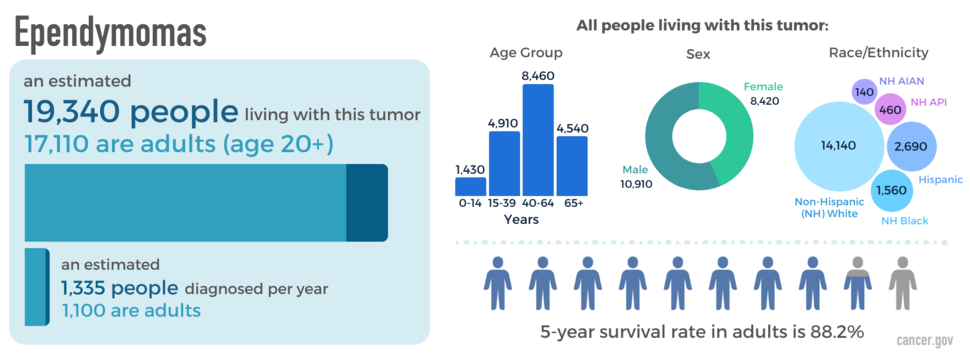
Ependymomas occur in both children and adults. Those in the lower half of the brain (“posterior fossa”) are more common among children. Those in the spine are more common among adults. Ependymomas occur more often in males than females. They are most common in non-Hispanic white people. An estimated 19,340 people are living with this tumor in the United States.
What Is the Prognosis of an Ependymoma?
The likely outcome of the disease or chance of recovery is called prognosis. Prognosis is based on the tumor grade, location, tumor type, extent of tumor spread, genetic findings, patient’s age, and tumor remaining after surgery (if surgery is possible).
The relative five-year survival rate for ependymoma is 88.2 percent. However, many factors can affect prognosis. These include the tumor grade and molecular type, the person’s age and health when diagnosed, and how they respond to treatment. If you want to understand your prognosis, talk to your doctor.
What Are the Treatment Options for Ependymomas?
The first treatment for an ependymoma is surgery, if possible. The goal of surgery is to obtain tissue to determine the tumor type and remove as much tumor as possible without causing more symptoms.
Many people won’t need additional treatment after surgery. For those that do, these treatments may include radiation, chemotherapy or clinical trials. Clinical trials test new chemotherapy, targeted therapy, or immunotherapy drugs. Treatments are decided by the patient’s health care team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location.
Open Clinical Studies for Ependymomas
- PLX038 in CNS Tumors
- Immune Checkpoint Inhibitor Nivolumab for Patients with Rare CNS Cancers
- ONC206 for Patients with Rare CNS Neoplasms
Learn More
- A Celebration of Hope for the Brain and Spine Tumor Community
- Video: Clinical Trial Tests Nivolumab for Patients with Rare Brain and Spine Cancers
- Statistical Report Highlights Key Trends in Adolescents and Young Adults with Brain Tumors
- Modifying a Chemotherapy Drug Offers Hope to People with Rare Brain and Spine Tumors
- Read our NCI-CONNECTions Blog for current news and information on brain and spine tumors
Referrals
NCI-CONNECT doctors and nurses work with you and your primary doctor to collaborate on a comprehensive care plan that treats your brain or spine tumor. They will also help you cope with the physical and emotional aspects of your diagnosis. Learn about requesting a consultation >