Primitive neuro-ectodermal tumors (PNETs) are primary central nervous system (CNS) tumors. This means they begin in the brain or spinal cord. PNET is a term that stands for a group of tumors, and these tumors are currently being reclassified and given other specific names based on their molecular features.
To get an accurate diagnosis, a piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.
What Are the Grades of PNETs?
Primary CNS tumors are graded based on a tumor tissue analysis performed by a neuropathologist. This group of tumors, formerly known as PNETs, is comprised of grade 4 (also written as grade IV) tumors. That means they are malignant (cancerous) and fast-growing. The tumor types in this group are:
- Medulloepithelioma
- CNS neuroblastoma
- CNS ganglioneuroblastoma
- Embryonal tumor with multilayered rosettes and other unspecified embryonal tumors
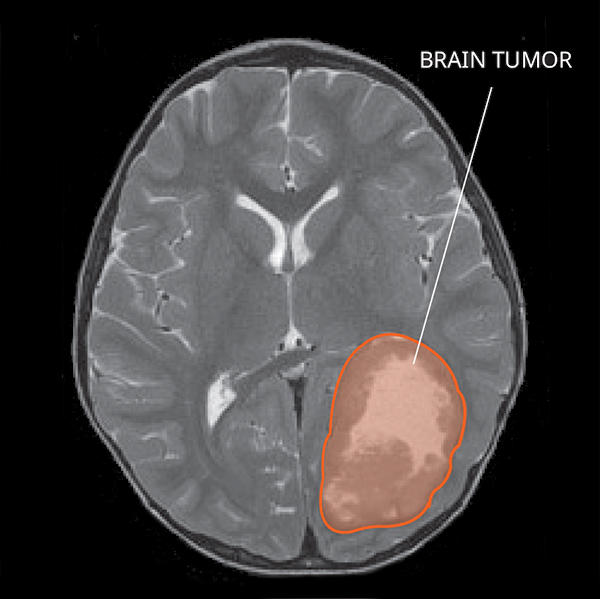
What Do PNETs Look like on an MRI?
On a magnetic resonance imaging (MRI) scan, PNETs usually initially appear as a single mass in the cortex, which is the outer layer of the brain. PNETs often enhance with contrast and more than one tumor can be identified. Sometimes, there are cysts (fluid collections) found within the mass. PNETs may also have some swelling around them.
What Causes PNETs?
Cancer is a genetic disease—that is, it is caused by certain changes to genes that control the way our cells function. Genes may be mutated (changed) in many types of cancer, which can increase the growth and spread of cancer cells. The cause of PNETs is not known. However, some PNETs are related to genetic changes.
Where Do PNETs Form?
PNETs are commonly found in the brain. Rarely, they can be found in the brainstem or spinal cord. PNETs form from the ectoderm, the outermost layer of cells on an embryo during early development.
Do PNETs Spread?
PNETs can spread to other areas of the CNS and organs. About a third of patients have tumors that have already spread at the time of diagnosis.
What Are the Symptoms of PNETs?
PNET symptoms depend on the tumor’s location. Here are some possible symptoms that can occur:
- Headaches
- Seizures
- Thinking or memory problems
- Weakness
- Numbness
- Problems with balance and movement
People with PNETs in the spine may have:
- Bowel or bladder incontinence
- Pain in the back and legs
Who Is Diagnosed with PNETs?
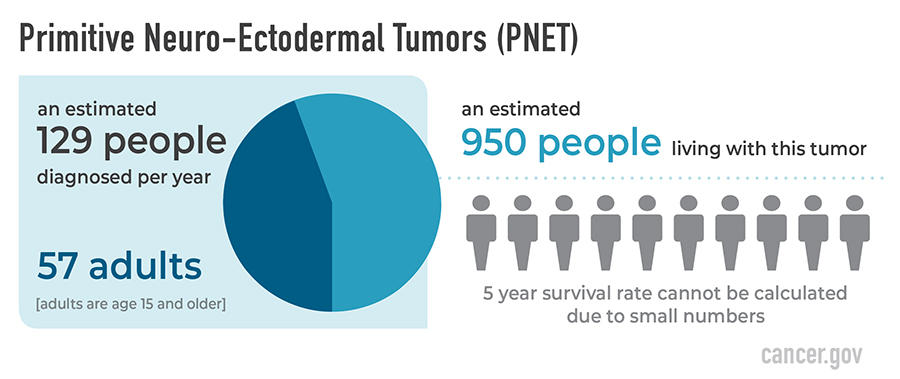
The former diagnosis of PNETs includes a heterogeneous group of tumors, most of which can occur in adults but are more common in children. They are very rare tumors and their classification is evolving. Tumors that were previously diagnosed as PNETs can now be reclassified with new diagnostic techniques into other tumor types, including recently described new tumors.
As of 2016, these tumors are no longer classified all together as PNETs. Therefore, statistics for the number of people diagnosed per year, the number of people living with the disease, and the survival rates in the United States are difficult to estimate. The PNET data below were captured between 2000 and 2014. At that time, an estimated 950 people were living with this tumor in the United States.
What Is the Prognosis of PNETs?
The likely outcome of the disease or chance of recovery is called prognosis. Prognosis is based on tumor grade, location, tumor type, extent of tumor spread, genetic findings, the patient’s age, and tumor remaining after surgery (if surgery is possible).
The relative five-year survival rate for PNETs between 2000 and 2014 cannot be calculated due to small numbers. There are many factors that can affect prognosis. If you want to understand your prognosis, talk to your doctor.
What Are the Treatment Options for PNETs?
The first treatment for PNETs is surgery, if possible. The goal of surgery is to obtain tissue to determine the tumor type and remove as much tumor as possible without causing more symptoms.
People with PNETs usually receive additional treatments as well. Surgery is usually followed by radiation in patients age 3 years or older, sometimes to both the brain and the spine. Clinical trials testing new chemotherapy, targeted therapy, or immunotherapy drugs may also be available. Treatments are decided by the patient’s health care team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location.
Open Clinical Studies for PNETs
- PLX038 in CNS Tumors
- Immune Checkpoint Inhibitor Nivolumab for Patients with Rare CNS Cancers
- ONC206 for Patients with Rare CNS Neoplasms
Learn More
- Video: Clinical Trial Tests Nivolumab for Patients with Rare Brain and Spine Cancers
- Statistical Report Highlights Key Trends in Adolescents and Young Adults with Brain Tumors
- Modifying a Chemotherapy Drug Offers Hope to People with Rare Brain and Spine Tumors
- Smart Wearables Show Promise for Tracking Sleep Patterns in Brain Tumor Patients
- Read our NCI-CONNECTions Blog for current news and information on brain and spine tumors
Referrals
NCI-CONNECT doctors and nurses work with you and your primary doctor to collaborate on a comprehensive care plan that treats your brain or spine tumor. They will also help you cope with the physical and emotional aspects of your diagnosis. Learn about requesting a consultation >