Pleomorphic xanthoastrocytoma (PXA) is a very rare type of astrocytoma, a primary central nervous system (CNS) tumor. This means it begins in the brain or spinal cord.
PXAs typically have genetic alterations, such as the BRAFV600E mutation, that affect a series of chemical reactions known as the MAPK signaling pathway. These genetic alterations can ultimately help the tumor cells grow and survive. While these genetic changes help form and maintain the tumor, they may also be targeted for treatment.
To get an accurate diagnosis, a piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.
What Are the Grades of PXAs?
Primary CNS tumors are graded based on a tumor tissue analysis performed by a neuropathologist.
PXAs tumors are grouped into two grades (grade 2 or grade 3, also written as grade II or grade III) based on their characteristics.
- Grade 2 PXAs are low-grade tumors. This means the tumor cells grow slowly.
- Grade 3 PXAs are malignant (cancerous). This means they are fast-growing tumors.
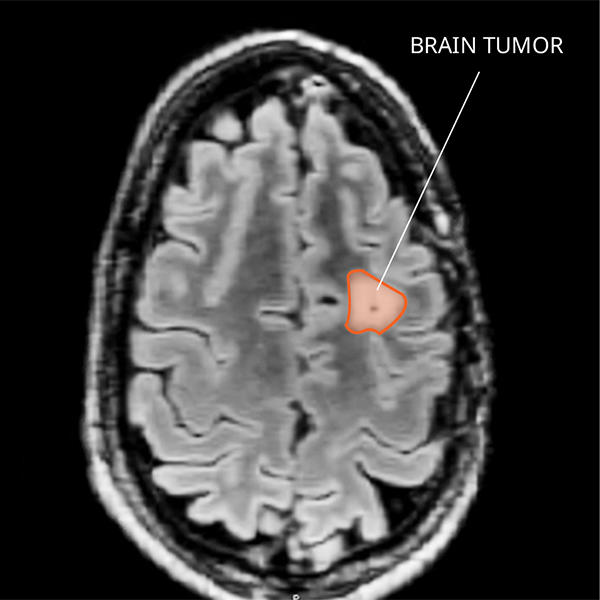
What Do PXAs Look like on an MRI?
PXAs often form fluid-filled cysts within solid tissue, which have a dense appearance on a magnetic resonance imaging (MRI) scan. The way grade 3 PXAs look varies and makes it difficult to tell them apart from other primary CNS tumors. Diagnosing PXAs can’t be done by imaging alone, because they may look similar to glioblastomas and other high-grade brain cancers.
What Causes PXAs?
Cancer is a genetic disease—that is, it is caused by certain changes to genes that control the way our cells function. Genes may be mutated (changed) in many types of cancer, which can increase the growth and spread of cancer cells.
The cause of most PXAs is not known. However, people with gene changes that can be passed down through families—such as Neurofibromatosis type I and familial melanoma/astrocytoma syndrome—are at increased risk of developing PXAs.
Where Do PXAs Form?
PXAs usually occur in one of the four lobes of the brain. The temporal lobe is the most common location. Rarely, PXAs form in the cerebellum, brainstem, and spinal cord. They are usually located close to the surface of the brain tissue. Scientists believe these tumors arise from cells that grow into glial and nerve cells.
PXAs can look a variety of ways under the microscope and can be challenging to diagnose, as they share characteristics with other primary brain tumors. An expert neuropathologist should confirm this diagnosis. Molecular testing will often reveal a BRAF gene change in these tumors.
Do PXAs Spread?
Grade 2 PXAs are slow-growing tumors that usually don’t spread. Grade 3 PXAs are fast-growing tumors that usually invade brain tissue in the lobe of the brain where they started. It’s rare for PXAs of any grade to spread to other areas of the CNS. There are no reported cases of spread outside the CNS.
What Are Symptoms of a PXA?
PXA symptoms depend on the tumor’s location. Here are some possible symptoms that can occur.
People with grade 2 PXAs may have:
- Seizures
- Epilepsy
- Chronic headaches
People with grade 3 PXAs may have:
- Seizures
- Weakness
- Numbness
- Speech and language changes
Who Is Diagnosed with a PXA?
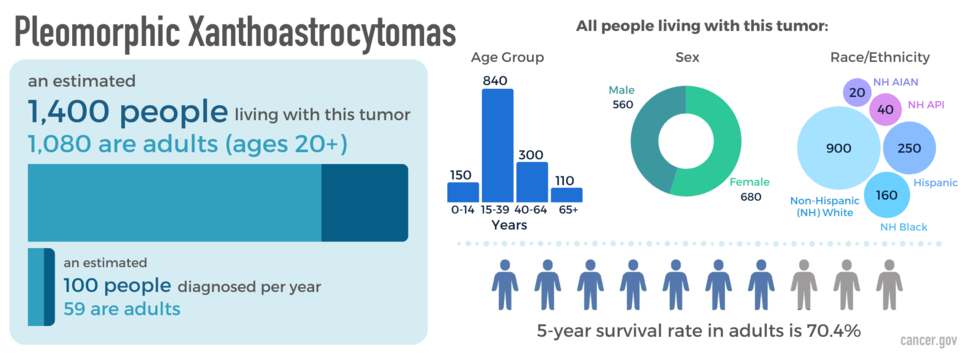
PXAs can occur at any age but are most common in young adulthood. These tumors occur slightly more often in females than males, and they are more common in non-Hispanic white people. An estimated 1,400 people are living with this tumor in the United States.
What Is the Prognosis of a PXA?
The likely outcome of the disease or chance of recovery is called prognosis. Prognosis is based on tumor grade, location, tumor type, extent of tumor spread, genetic findings, the patient’s age, and tumor remaining after surgery (if surgery is possible).
The relative five-year survival rate for PXA is 70.4 percent. However, there are many factors that affect prognosis. These include the tumor grade and molecular type, the person’s age and health when diagnosed, and how they respond to treatment. If you want to understand your prognosis, talk to your doctor.
What Are the Treatment Options for PXAs?
The first treatment for a PXA is surgery, if possible. The goal of surgery is to obtain tissue to determine the tumor type and remove as much tumor as possible without causing more symptoms. Grade 2 PXAs can often be treated by surgery alone.
If a PXA comes back after surgery, there is no standard treatment. Possible treatments at this time may include radiation, chemotherapy, or clinical trials. If a BRAF change is present, clinical trials using a drug to target that genetic alteration may also be an option. Treatments are decided by the patient’s health care team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location.
Open Clinical Studies for PXAs
- PLX038 in CNS Tumors
- Immune Checkpoint Inhibitor Nivolumab for Patients with Rare CNS Cancers
- ONC206 for Patients with Rare CNS Neoplasms
Learn More
- Video: Clinical Trial Tests Nivolumab for Patients with Rare Brain and Spine Cancers
- Statistical Report Highlights Key Trends in Adolescents and Young Adults with Brain Tumors
- Modifying a Chemotherapy Drug Offers Hope to People with Rare Brain and Spine Tumors
- Smart Wearables Show Promise for Tracking Sleep Patterns in Brain Tumor Patients
- Read our NCI-CONNECTions Blog for current news and information on brain and spine tumors
Referrals
NCI-CONNECT doctors and nurses work with you and your primary doctor to collaborate on a comprehensive care plan that treats your brain or spine tumor. They will also help you cope with the physical and emotional aspects of your diagnosis. Learn about requesting a consultation >