The Importance of Cancer Screening and Detection Research
People whose cancers are detected through screening, before symptoms develop, may be less likely to die from their disease than people whose cancers are not found until symptoms appear. As a result of important successes in screening and early detection, the risk of death has declined for some cancer types. Deaths from cervical cancer in the United States, for example, dropped substantially after screening with the Pap test became common practice, and screening for colorectal, lung, and breast cancer have also been shown to reduce deaths from these cancers. For some cancer sites, like the cervix, skin, colon, and rectum, screening for and removal of precancerous growths can prevent cancer from occurring in the first place.
However, even effective screening tests can have downsides, including the risk of overdiagnosis and overtreatment—the diagnosis and treatment of cancers that would not cause symptoms, health complications, or death.
This understanding has led to intensive study of ways to identify and distinguish those screen-detected cancers that are truly life threatening and require immediate treatment from those for which treatment is unnecessary or can be safely delayed.
And, unfortunately, effective screening tests do not exist for many cancers. Research to identify early detection strategies for these cancer types may lead to new developments that can prevent cancer deaths. A greater understanding of the underlying biology of many cancers—in particular, how they progress from precancers to invasive cancer—is creating new avenues for advances in screening and early detection. Technological advances in areas such as imaging and detection of DNA and proteins shed by cancer cells into the circulation may also contribute to better, more precise screening and earlier detection.
Selected NCI Activities in Cancer Screening and Detection Research
Developing and testing new interventions for screening and early detection can take decades. These studies also are often expensive and logistically difficult to conduct. Although research on cancer screening and early detection can be challenging, the potential rewards, in terms of cancer deaths avoided, make it an extremely important and valuable area of study.
NCI supports a variety of programs designed to improve early detection, enhance cancer screening, and address screening barriers that contribute to health disparities.
- NCI established the Cancer Screening Research Network (CSRN) to study emerging technologies for cancer screening – such as multi-cancer detection (MCD) tests – with the goal of reducing cancer-related illnesses and deaths. MCD tests are a new type of blood test that may find multiple kinds of cancers. In 2025, the CSRN will begin enrolling people without cancer in a pilot Vanguard Study to address the feasibility of using MCD tests in a larger randomized controlled trial. This larger trial will evaluate whether the benefits of using MCD tests to screen for cancer outweigh the harms, and whether they can detect cancer early in a way that reduces deaths. Learn more about the Vanguard Study on Multi-Cancer Detection Tests.
- Discovering and validating biomarkers that can help detect cancer at its earliest stages is the primary mission of NCI's Early Detection Research Network (EDRN). A number of biomarkers discovered by EDRN-supported researchers are being studied to determine whether they are ready for clinical testing, including biomarkers for prostate, pancreatic, ovarian, and esophageal cancer.
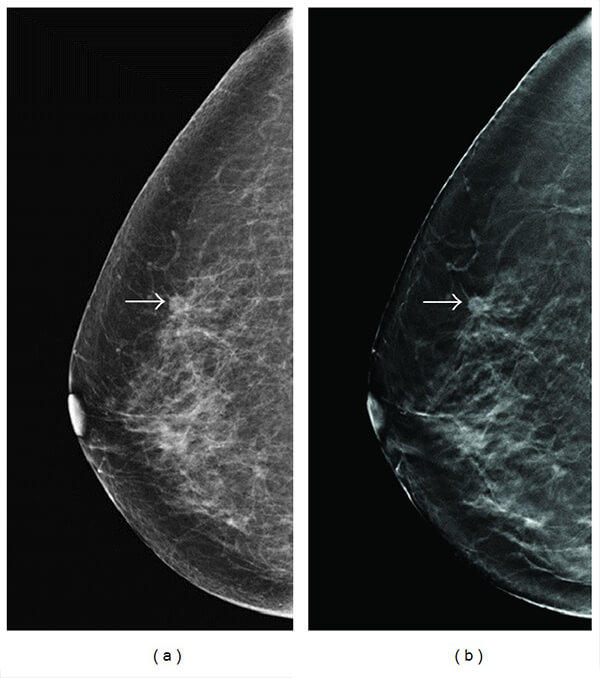
- NCI also leads and supports large cancer screening trials to learn the best way to find cancer and prevent deaths from the disease. Tomosynthesis Mammographic Imaging Screening Trial (TMIST) is a randomized breast screening trial that is comparing two Food and Drug Administration (FDA)-approved types of digital mammography, standard digital mammography (2-D) and tomosynthesis mammography (3-D), to see which one is better at detecting cancer early. The Women Informed to Screen Depending On Measures of risk (WISDOM) study is comparing two approaches to breast screening: annual mammograms and personalized screening schedules based on a woman’s risk for breast cancer, including genetic risk factors, lifestyle, and breast density.
- The institute conducts and funds research that correlates findings from studies on the performance of imaging modalities for early detection of cancer with similar data from biomarker studies. The goal is to improve the overall efficacy of screening by combining these approaches to detect cancer earlier and reducing the number of false-positive screening results.
- The Cancer Intervention and Surveillance Modeling Network (CISNET) uses statistical modeling to understand the population-wide impact of cancer control interventions, including screening. CISNET studies have been used by the US Preventive Services Task Force to inform their recommendations on screening guidelines for lung, breast, colorectal, prostate, and cervical cancers, as well as by the Centers for Medicare and Medicaid Services to inform coverage policies for related screening.
- NCI family studies have identified the genetic causes of several hereditary cancers, which has implications for preventive care and cancer screening among these individuals. For example, NCI researchers are investigating hereditary melanoma and a rare cancer called chordoma, as well as the genetic factors behind cancer predisposition syndromes like Li-Fraumeni syndrome, Fanconi anemia, and telomere biology disorders.
- Researchers at NCI have led efforts to prevent and control cervical cancer by improving screening. Those efforts include developing and validating HPV genotyping assays for low-cost, rapid HPV DNA tests for screening in low-resource settings, developing molecular markers to detect cervical precancers, unifying screening guidelines and recommendations, and integrating global screening and vaccination efforts. The Cervical Cancer ‘Last Mile’ Initiative, for example, is a public–private partnership investigating whether self-collected samples can be used for HPV testing in cervical cancer screening.
- Accelerating Colorectal Cancer Screening and follow-up through Implementation Science (ACCSIS) is building the evidence base for multilevel interventions to increase rates of colorectal cancer screening, follow-up, and referral to treatment—especially in underserved groups, including racial and ethnic minority populations and people living in rural or difficult-to-reach areas.
- Population-based Research to Optimize the Screening Process (PROSPR) is an NCI-funded research network that aims to inform how to improve the cancer screening process—from recruitment to screening, diagnosis, and referral for treatment—in community health care settings. PROSPR is conducting multilevel observational research to evaluate factors that affect the quality and outcomes of the screening process for cervical, colorectal, and lung cancers.
Recent Research Findings in Cancer Screening and Detection
- Blood Test Accurately Detects Early-Stage Pancreatic Cancer
- Pump Up the Volume: “Priming Agents” May Improve Cancer Liquid Biopsies
- NIH launches research network to evaluate emerging cancer screening technologies
- First Direct Comparison of Screening Methods for Nasopharyngeal Carcinoma
- 3-in-1 Approach Helps Women in Rural Areas Get Cancer Screenings
- Can the New “Omics” on the Block Find Liver Cancer in Blood?
- Validation of a Low-cost, Rapid HPV DNA Genotyping Test for Cervical Cancer Prevention