Causes of childhood MEN2 syndrome
MEN2 syndrome is an inherited disorder, meaning it is caused by an inherited, harmful genetic change (also called pathogenic variant or mutation) in the RET gene. In most families with MEN2A and 50% of families with MEN2B, this mutation is inherited from a parent. In some cases, the mutation in the RET gene appears for the first time in the child. Learn more about how cancer develops at What Is Cancer?
Genetic counseling for children who may have MEN2 syndrome
It may not be clear from the family medical history whether your child has MEN2 syndrome. Genetic counseling before genetic testing can help assess your child's risk of having a gene change that caused your child's tumor and whether genetic testing is needed. Genetic counselors and other specially trained health professionals can discuss your child's diagnosis and family medical history to understand:
- the options for genetic testing for mutations in the RET gene, which is usually linked to an aggressive cancer called medullary thyroid carcinoma
- the risk of cancer for your child and their siblings
- the risks and benefits of learning genetic information
Genetic counselors can also help you cope with your child's genetic testing results, including how to discuss the results with family members. They can advise you about whether other members of your family should receive genetic testing.
Learn more about genetic testing at Genetic Testing for Inherited Cancer Risk.
Diagnosing MEN2 based on the family medical history
A child may be diagnosed with MEN2A syndrome when a genetic test finds a mutation in the RET gene or when the child, their parent, sibling, or aunt or uncle has two or more of the following conditions: medullary thyroid carcinoma, pheochromocytoma, or parathyroid gland disease.
Familial medullary thyroid cancer may be diagnosed when two or more family members have medullary thyroid cancer and no family members have parathyroid or adrenal gland problems.
MEN2B may be diagnosed when the child has a personal or family medical history of medullary thyroid cancer or pheochromocytoma. They may also be diagnosed if they have certain physical symptoms of MEN2B.
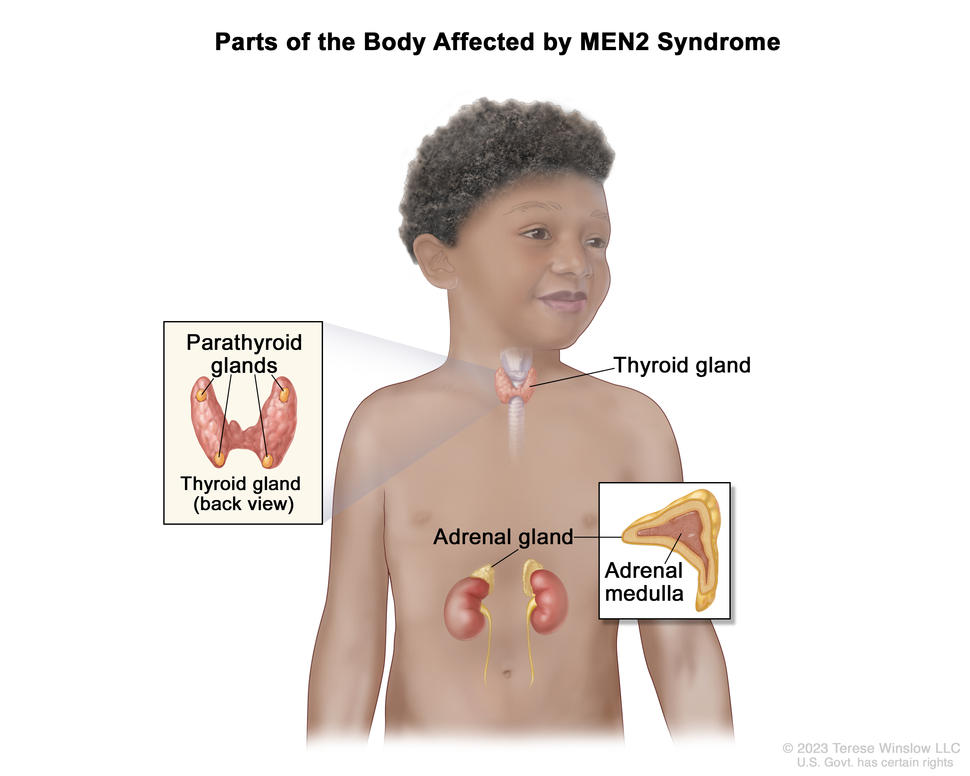
Symptoms of tumors caused by childhood MEN2A syndrome and MEN2B syndrome
In MEN2A, a tumor may be the first symptom of the syndrome. Children with MEN2B may have a slender body with long, thin arms and legs and curvature of the spine (scoliosis). The lips may appear large and bumpy because of benign tumors in the mucous membranes.
The symptoms of tumors associated with MEN2A or MEN2B syndrome depend on where the tumors form in the body. It's important to check with your child's doctor if your child has any of the symptoms below.
Symptoms of medullary thyroid cancer include:
- a lump in the throat or neck
- trouble breathing
- trouble swallowing
- hoarseness
Symptoms of pheochromocytoma include:
- high blood pressure
- pain in the abdomen or chest
- a strong, fast, or irregular heartbeat
- headache
- heavy sweating for no known reason
- dizziness
- feeling shaky
- being irritable or nervous
Symptoms of parathyroid gland disease include:
- hypercalcemia
- pain in the abdomen, side, or back that doesn't go away
- pain in the bones
- a broken bone
- kidney stone
- weakness
- a lump in the neck
- trouble speaking
- trouble swallowing
These symptoms may be caused by problems other than MEN2 syndrome. The only way to know is to see your child's doctor.
Tests to diagnose tumors caused by MEN2 syndrome
If your child has symptoms that suggest MEN2 syndrome, their doctor will need to find out if these are due to this syndrome or another problem. The doctor will ask when the symptoms started and how often your child has been having them. They will ask about your child's personal and family medical history and do a physical exam. Depending on these results, they may recommend other tests. If your child is diagnosed with MEN2 syndrome, the results of these tests will help you and your child's doctor plan treatment.
The tests used to diagnose a mutation in the RET gene or tumors caused by MEN2 syndrome include:
Lab tests
- Blood chemistry study measures the amounts of certain substances released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease.
- Blood hormone study measures the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may also be checked for high levels of the hormone calcitonin or parathyroid hormone (PTH).
- 24-hour urine test is used to diagnose neuroendocrine tumors, such as pheochromocytoma. Urine is collected for 24 hours to measure the amounts of a group of hormones called catecholamines in the urine. Substances caused by the breakdown of catecholamines are also measured. An unusual amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher than normal amounts may be a sign of pheochromocytoma.
- Venous sampling for an overactive parathyroid gland is a procedure in which a sample of blood is taken from veins near the parathyroid glands. The sample is checked to measure the amount of parathyroid hormone released into the blood by each gland. Venous sampling may be done if blood tests show there is an overactive parathyroid gland but imaging tests don’t show which one it is.
- Pentagastrin stimulation test is a test in which blood samples are checked to measure the amount of calcitonin in the blood. Calcium gluconate and pentagastrin are injected into the blood and then several blood samples are taken over the next 5 minutes. If the level of calcitonin in the blood increases, it may be a sign of medullary thyroid cancer.
- Genetic testing analyzes cells or tissue to look for changes in genes or chromosomes. These changes may be a sign that a person has or is at risk of having a specific disease or condition. To diagnose MEN2 syndrome, a sample of blood or saliva is checked for the RET gene.
Imaging tests
- Ultrasound exam uses high-energy sound waves (ultrasound) that bounce off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
- MRI (Magnetic resonance imaging) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- PET scan uses a small amount of radioactive sugar (radioactive glucose) injected into a vein. Then the PET scanner rotates around the body to make detailed, computerized pictures of areas inside the body where the glucose is taken up. Because cancer cells often take up more glucose than normal cells, the pictures can be used to find cancer cells in the body.
- Thyroid scan uses a small amount of a radioactive substance that is swallowed or injected. The radioactive material collects in thyroid gland cells. A special camera linked to a computer detects the radiation given off and makes pictures that show how the thyroid looks and functions and whether the cancer has spread beyond the thyroid gland.
- Sestamibi scan is a type of radionuclide scan used to find an overactive parathyroid gland. A very small amount of a radioactive substance called technetium 99 is injected into a vein and travels through the bloodstream to the parathyroid gland. The radioactive substance will collect in the overactive gland and show up brightly on a special camera that detects radioactivity.
- CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. Learn more about Computed Tomography (CT) Scans and Cancer.
- MIBG scan is used to find neuroendocrine tumors, such as pheochromocytoma. A very small amount of a substance called radioactive MIBG is injected into a vein and travels through the bloodstream. Neuroendocrine tumor cells take up the radioactive MIBG and are detected by a scanner. Scans may be taken over 1–3 days. An iodine solution may be given before or during the test to keep the thyroid gland from absorbing too much of the MIBG.
Biopsy
A biopsy is a procedure in which a sample of tissue is removed from the tumor so that a pathologist can view it under a microscope to check for signs of cancer. The following biopsies are used to check for tumors from MEN2 syndrome:
- Fine-needle aspiration (FNA) is a procedure in which tissue is removed using a thin needle.
- Surgical biopsy is the removal of tissue during surgery.
Getting a second opinion
You may want to get a second opinion to confirm your child’s MEN2 diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the genetic test report, pathology report, slides, and scans before giving a recommendation. They may agree with the first doctor, suggest changes to the treatment plan, or provide more information about your child’s cancer.
To learn more about choosing a doctor and getting a second opinion, visit Finding Cancer Care. You can contact NCI’s Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital that can provide a second opinion. For questions you might want to ask at your child's appointments, see Questions to Ask Your Doctor About Cancer.
Cancer surveillance for children with MEN2 syndrome
Surveillance is closely following a child's condition without giving any treatment unless there are changes in test results. Children who are diagnosed with MEN2 syndrome will be checked for signs of pheochromocytoma starting at age 10 years and will continue to be checked throughout life. Talk with your child's doctor about tests and procedures needed and how often they should be done.
Who treats children with tumors caused by MEN2 syndrome?
A pediatric oncologist, a doctor who specializes in treating children with cancer, oversees treatment for children with tumors caused by MEN2 syndrome. The pediatric oncologist works with other health care providers who are experts in treating children with cancer and who specialize in other areas of medicine. Other specialists may include:
Types of treatment for children with tumors caused by MEN2 syndrome
There are different types of treatment for children and adolescents with tumors related to MEN2 syndrome. You and your child's cancer team will work together to decide treatment. Many factors will be considered, such as your child's overall health and whether the cancer is newly diagnosed or has come back.
Your child’s treatment plan will include information about the cancer, the goals of treatment, treatment options, and the possible side effects. It will be helpful to talk with your child’s cancer care team before treatment begins about what to expect. For help every step of the way, see our booklet, Children with Cancer: A Guide for Parents.
Types of treatment your child might have include:
Surgery
Surgery may be done to remove the thyroid gland when a child has medullary thyroid cancer caused by MEN2 syndromes. The thyroid may also be removed to prevent medullary thyroid cancer from developing.
Targeted therapy
Targeted therapy uses drugs or other substances to block the action of specific enzymes, proteins, or other molecules involved in the growth of tumor cells.
Selpercatinib and vandetanib are used to treat medullary thyroid cancer caused by MEN2 syndrome.
Learn more about Targeted Therapy to Treat Cancer.
Clinical trials
For some children, joining a clinical trial may be an option. There are different types of clinical trials for childhood cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your child's age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Cancer Clinical Trial Information for Patients and Caregivers.
Treatment of tumors caused by childhood MEN2A syndrome
There is an increased risk of medullary thyroid cancer, an aggressive form of thyroid cancer, in people with MEN2A syndrome. Children with MEN2A syndrome and certain changes in the RET gene usually have surgery to remove the thyroid before age 5 years to lessen the chance cancer will form or spread. Treatment is also given for pheochromocytoma and hyperparathyroidism as needed.
Treatment of medullary thyroid cancer in children who have MEN2A syndrome may include:
- surgery to remove the thyroid
- targeted therapy with selpercatinib
Treatment of tumors caused by childhood MEN2B syndrome
There is an increased risk of medullary thyroid cancer, an aggressive form of thyroid cancer, in people with MEN2B syndrome. Infants with MEN2B syndrome and certain changes in the RET gene usually have surgery to remove the thyroid to lessen the chance cancer will form. Treatment is also given for pheochromocytoma and other conditions as needed.
Children with MEN2B syndrome who have medullary thyroid cancer may be treated with:
- surgery to remove the thyroid
- targeted therapy with vandetanib or selpercatinib
Treatment of recurrent tumors caused by childhood MEN2 syndrome
If the cancer linked to MEN2 syndrome comes back after treatment, your child’s doctor will talk with you about what to expect and possible next steps. There might be treatment options that may shrink the cancer or control its growth. If there are no treatments, your child can receive care to control symptoms from cancer so they can be as comfortable as possible.
Prognosis for children with tumors caused by MEN2A syndrome and MEN2B syndrome
If your child has been diagnosed with tumors caused by MEN2 syndrome, you likely have questions about how serious the cancer is and your child's chances of survival. The likely outcome or course of a disease is called prognosis. The prognosis for MEN2A syndrome is usually good. The prognosis for MEN2B syndrome is not as good as the prognosis for MEN2A syndrome because this syndrome can cause a more aggressive form of medullary thyroid cancer.
No two people are alike, and responses to treatment can vary greatly. Your child's cancer care team is in the best position to talk with you about your child's prognosis.
Follow-up care
As your child goes through treatment, they will have follow-up tests or check-ups. Some of the tests that were done to diagnose the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has recurred (come back).
Coping with your child's cancer
When your child has a tumor, every member of the family needs support. Taking care of yourself during this difficult time is important. Reach out to your child's treatment team and to people in your family and community for support. Learn more at Support for Families: Childhood Cancer.