Research in the Diagnosis of Brain and Spinal Cord Tumors
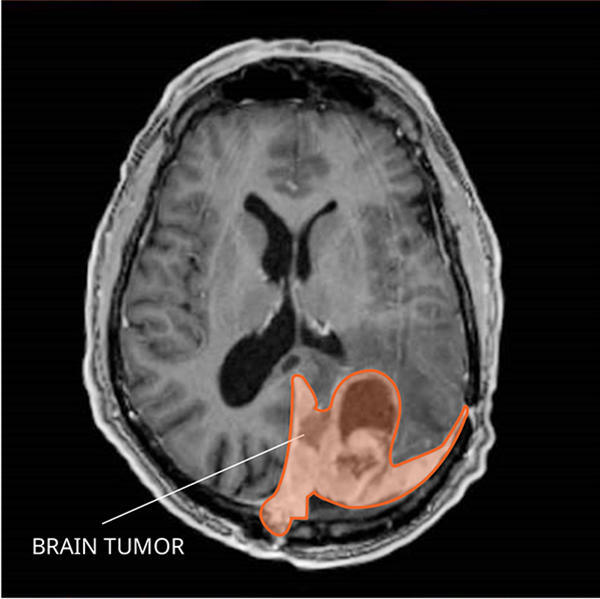
Many types of brain and spinal cord tumors look similar when the cells are examined under the microscope. Even with trained pathologists examining tissue samples, up to 10% of people with a brain or spinal cord tumor receive the wrong diagnosis at first. This can potentially affect outcomes, because tumors that look similar at the cellular level may require very different treatments.
NCI-supported researchers are studying ways to improve the diagnosis of brain and spinal cord tumors. For example:
- A type of blood test called a liquid biopsy was able to distinguish between several different types of brain tumors in adult patients. This test checks for chemical changes in tumor DNA that has been shed into the bloodstream. Researchers hope that such tests could not just improve the accuracy of diagnoses but someday be used to diagnose brain tumors without the need for invasive surgery to get biopsy samples.
- A different liquid biopsy test was able to detect a specific genetic alteration in children with a rare type of brain tumor. Such tests could eventually help select patients for studies of new targeted therapies.
- Another study found that a blood test that detects genomic changes in DNA shed from a brain tumor called medulloblastoma could identify children who still had evidence of cancer after treatment. Such children are at high risk of relapse and may benefit from more aggressive therapy upfront.
- Researchers are also measuring changes in the way certain genes are expressed in a type of brain tumor called meningioma. Such measurements may identify which patients need radiation therapy after surgery and which patients can safely skip it.
- Scientists are also testing the use of artificial intelligence, or AI, for the analysis of images to speed the diagnosis of brain tumors during surgery.
If you have received a diagnosis of a rare brain or spinal cord tumor and are seeking a second opinion, the NCI-CONNECT program offers free consultations, as well as advice for patients’ cancer care teams at home.
Research in Treatments for Brain and Spinal Cord Tumors in Adults
Treatments for brain and spinal cord tumors can damage normal cells as well as tumor cells in the brain and spinal cord, so they may come with serious side effects. And many brain tumors come back (recur) soon after treatment.
Researchers are testing ways to improve the treatment of brain and spinal cord tumors, including targeted therapies, improving radiation response, and immunotherapies.
Targeted Therapy for Brain and Spinal Cord Tumors
Targeted therapies use drugs or other substances to attack specific types of cancer cells with less harm to normal cells. Researchers are developing treatments that target the specific changes that drive the growth of brain and spinal cord tumors.
- Recent studies have found that some brain tumors have mutations in a gene called IDH.
- In a large clinical trial, treatment with the targeted drug vorasidenib (Voranigo) slowed the growth of tumors in some people with low-grade gliomas that had mutations in the IDH1 or IDH2 genes, postponing the need for additional therapies. In 2024, the FDA approved vorasidenib for these patients following surgery.
- For tumors with mutations in IDH, treatment with a type of drug called a PARP inhibitor may make them more sensitive to chemotherapy. A clinical trial is testing this strategy in people with a type of brain tumor called a glioma that has recurred after initial treatment.
- Other treatments for IDH-mutated tumors are targeting changes in cancer metabolism.
- A recent study found that targeting a genetic change called BRAF V600E in a rare type of brain tumor called papillary craniopharyngioma let many people delay invasive surgery or radiation therapy for years.
- Another drug that targets this and other BRAF changes, called tovorafenib (Ojemda), was approved in 2024 to treat pediatric low-grade glioma. Although most often found in children, these tumors can also occur in adolescents and adults.
- Some studies are trying to target proteins found widely in brain and spinal cord tumors. For example, NCI researchers are testing a drug that blocks dopamine receptors in recurrent brain and spine tumors. Dopamine receptors are found in many of these tumor types.
- Researchers are using powerful computers to look through enormous databases of genetic mutations and combinations of genes, called fusion genes, found in brain tumors. The goal is to pinpoint which genes the tumor cells rely on to survive. These mutations and fusions could then potentially be targeted with new or existing drugs.
Scientists are also trying to understand other biological factors that influence brain tumor development and its response to treatment. For example, studies have found that glioblastoma in women tends to respond better to standard treatments. Such work may uncover further avenues for treatment personalization.
Testing targeted therapies for brain and spinal cord tumors can be challenging, because clinical trials will be limited to fewer patients with already rare cancers. Examples of NCI-led initiatives to overcome this challenge and foster collaboration across cancer centers include the NCI-led Brain Tumor Trials Collaborative and NCI-CONNECT clinical trial network. (See more in the NCI-Supported Research Programs section below.)
Improving the Response to Radiation
The amount and shape of the tissue that gets treated with radiation is tailored to each tumor’s size and location. However, the dose (or amount) of radiation used is usually the same for everyone with a specific tumor type.
- Researchers want to find ways to figure out whether a tumor’s response to radiation can be predicted before treatment. That would make it possible for people with tumors that are unlikely to shrink after standard doses of radiation to instead join clinical trials that are testing other strategies, such as higher radiation doses. Scientists are also studying whether machine learning, also called artificial intelligence or AI, can predict radiation response based on data from MRI scans of brain tumors.
- Scientists are also trying to develop substances called radiation sensitizers to improve killing of cancer cells. Dozens of small clinical trials across the country are studying radiation sensitizers in glioblastoma. For example, a trial led by NCI researchers is looking at whether the drug selinexor (Xpovio), when combined with chemotherapy and radiation, can improve survival.
Immunotherapy
For some blood cancers and solid tumors, immunotherapy drugs have provided huge gains in survival for some people. But to date, immunotherapy has not worked well for brain tumors. Issues may include:
- The blood–brain barrier. This network of blood vessels and tissue that helps protect the brain also prevents some drugs and types of immune cells from reaching tumors.
- The widespread use of anti-inflammatory drugs called corticosteroids to manage the symptoms of brain tumors. These drugs may limit the availability of the immune system to fight cancer. For example,
- A recent NCI-supported study found that corticosteroids may reduce the effectiveness of immunotherapy for brain cancer by suppressing the body’s immune response.
- Another study from NCI researchers found that steroids used to treat brain cancer may affect the development of T cells, which are key immune cells for fighting cancer.
However, some people with brain or spinal cord tumors given immunotherapy in clinical trials have had their tumors shrink or disappear. Researchers want to know if these responses could be predicted, both to spare people unnecessary treatment and to develop new strategies to make resistant tumors respond to immunotherapies.
- NCI researchers are running a clinical trial testing a combination of two immunotherapy drugs in people with newly diagnosed glioblastoma. As part of the study, they’re analyzing the activity of immune cells in the blood both before and during treatment. The findings might help predict who will benefit from immunotherapy and who won’t.
- Other studies are examining whether people whose brain tumors have certain mutations, such as those in the IDH gene, are more likely to have their tumors shrink from immunotherapy.
- Another study led by NCI researchers is testing whether the immunotherapy drug nivolumab (Opdivo) can shrink or control the growth or spread of specific types of recurrent rare brain or spine tumors. The trial is also testing the changes that nivolumab induces in immune cells in the blood during treatment, and whether the drug can improve the symptoms of people with these tumors.
Research in Survivorship and Quality of Life for People with Brain or Spinal Cord Tumors
Because both brain and spinal cord tumors and their treatments can be debilitating, researchers are looking for new ways to improve quality of life for people with these tumors.
- This may include using people’s quality of life to measure the benefit of new drugs or treatment combinations. For example, in a recent NCI-led trial of a drug combination to treat a rare tumor called ependymoma, most people’s tumors didn’t shrink. However, because they reported a reduction in symptoms from their tumor, the combination is now included in some professional recommendations for treatment of this cancer.
- NCI scientists are looking at whether genomic factors can predict the likelihood that a patient will experience side effects from certain treatments. They’re also performing experiments in the lab to understand the biological processes linked with these side effects. Results from these studies could potentially influence treatment decisions.
- For people with many cancer types, simply monitoring symptoms has been found to improve not just quality of life but survival. An NCI study is tracking symptoms and the well-being of people with brain and spinal cord tumors over time. People in that study can also take part in research into using virtual reality to reduce stress.
Research in the Treatment of Brain and Spinal Cord Tumors in Children
Tumors of the brain and spinal cord in children are relatively rare. But about 4,000 children and adolescents nationwide receive a diagnosis of a brain or spinal cord tumor every year, making them the second most common cancer type in this age group after leukemia.
Treatment has improved for young patients with these tumors over the last several decades. Although some brain and spinal cord tumors can’t be cured, almost three-quarters of children and adolescents treated for one will be alive 5 years after diagnosis.
However, effective treatments can harm children’s developing nervous systems. Current research in childhood brain and spinal cord tumors focuses on understanding the underlying causes of these cancers, developing new treatments, and reducing the toxic effects of effective therapies. For example,
- One study found that some children with medulloblastoma, a type of brain cancer, can safely get less radiation therapy without reducing their long-term survival. The effectiveness of this approach depended on the genetic alterations found in children’s tumors. A follow-up study is looking more closely at reducing the intensity of treatment in children with medulloblastoma caused by changes in a gene called WNT.
- Some children with a type of brain tumor called low-grade glioma have certain changes in a gene called BRAF in their cancer cells.
- A 2022 clinical trial found that, for children whose tumors have a BRAF mutation called V600, a combination of two targeted drugs was safer and better than standard chemotherapy at shrinking these tumors and keeping them from growing again. Approved by the FDA in 2023, these drugs, dabrafenib (Tafinlar) and trametinib (Mekinist), can be given orally as a liquid, making treatment easier for children as well.
- Most low-grade gliomas have BRAF gene changes called rearrangements or fusions. These happen when pieces of the gene get switched around or stuck to pieces of other genes. In 2024, tovorafenib (Ojemda) received FDA approval for treating low-grade gliomas that have these or other BRAF changes and that have returned after initial treatment. An ongoing study is now comparing tovorafenib against chemotherapy as part of initial treatment for children with low-grade glioma.
- A targeted drug called selumetinib (Koselugo) is approved for treating nerve tumors in children with a rare condition called neurofibromatosis type 1 (NF1) . A small study found that it could also shrink a type of brain tumor called low-grade glioma in some children with NF1 whose tumors have certain BRAF changes. NCI researchers have launched a clinical trial of the drug in children with and without NF1 who have low-grade glioma with these BRAF changes.
- A rare type of brain tumor called diffuse midline glioma, which occurs more commonly in children than adults, currently has no cure. An NCI-supported clinical trial is testing CAR T cells, a type of immunotherapy, that target cells with a mutation found in some of these tumors. The treatment has been found to shrink tumors and reduce neurologic symptoms caused by the tumor in some children.
- Other studies are using information about mutations in children’s brain tumors to test new treatments in those who may benefit the most. One such study, the Pediatric MATCH study, is testing new targeted therapies in children with solid tumors—including those in the brain or spinal cord—that have not responded to standard treatments. In the study, children are assigned to an experimental treatment based on the genetic changes found in their tumors rather than on their type of cancer or cancer site.
Additional clinical trials for children with brain and spinal cord tumors are being performed by the NCI-supported Children’s Oncology Group and Pediatric Brain Tumor Consortium.
NCI-Supported Research Programs
Many NCI-supported researchers working at the National Institutes of Health (NIH) campus, as well as across the United States and throughout the world, are seeking ways to address tumors of the brain and spinal cord more effectively. Some research is basic, exploring questions such as the biological underpinnings of cancer. And some is more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s related research efforts.
- The NCI-CONNECT Rare Brain and Spine Tumor Network is part of the Rare Tumor Patient Engagement Network. This network aims to advance the understanding of rare adult brain and spinal cord cancers by establishing and fostering patient–advocacy–provider partnerships and networks to improve approaches to care and treatment. Consultations are free of charge for people seeking a second opinion or expertise on a rare tumor type. NCI-CONNECT is now partnering with the MyPART program to advance the understanding of these tumors in adolescents and young adults. The program also runs clinical studies and trials focused on the treatment of rare adult brain and spinal cord tumors and on improving quality of life, symptom control, and management of side effects.
- The Brain Tumor Trials Collaborative network includes over 30 institutions with expertise in neuro-oncology from across the United States. The network’s mission is to develop and carry out clinical trials in a collaborative environment to advance treatments for patients with brain and spine tumors. NCI serves as the lead institution, providing administrative support, a clinical database, and oversight for the network. The network includes a weekly virtual tumor board that allows doctors at other treatment centers to consult with NCI experts without their patients needing to travel.
- The goal of the Optimizing Engagement in Discovery of Molecular Evolution of Low-Grade Glioma (OPTIMUM) study is to improve the care of people with low-grade glioma by learning more about the biology of the disease. The study aims to involve more people with low-grade glioma directly in identifying research priorities and to recruit participants for genetic studies of the disease.
- NCI’s Brain Cancer Specialized Programs of Research Excellence (SPOREs) promote collaborative, interdisciplinary research. SPORE grants involve both basic and clinical/applied scientists working together. They support the efficient movement of basic scientific findings into clinical settings, as well as studies to determine the biological basis for observations made in individuals with cancer or in populations at risk for cancer.
- NCI's National Clinical Trials Network is a collection of organizations and clinicians that coordinate and support cancer clinical trials at more than 3,000 sites across the United States and Canada. The network has a variety of trials testing treatments for brain and other CNS tumors.
- NCI has also formed partnerships with the pharmaceutical industry, academic institutions, and individual investigators for the early clinical evaluation of innovative cancer therapies. The Experimental Therapeutics Clinical Trials Network was created to evaluate these therapies using a coordinated, collaborative approach to early-phase clinical trials. The network is currently running early-stage trials in brain and other CNS tumors.
- NCI’s Division of Cancer Epidemiology and Genetics conducts studies on people with brain and other CNS tumors to learn about genetic and other risk factors for these diseases.
- NCI’s Office of Cancer Survivorship, part of the Division of Cancer Control and Population Sciences, supports many research projects that study survivorship issues in people who have been treated for brain tumors.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Use our clinical trials search form to find trials to treat glioblastoma, glioma, medulloblastoma, and other types of brain and spinal cord tumors.
Brain and Spinal Cord Tumor Research Results
The following are some of our latest news articles on brain and spinal cord tumor research.
- Experimental CAR T-Cell Therapy Shrinks Tumors in Children with Deadly Brain Cancer
- Experimental mRNA Vaccine Hints at Potential Against Glioblastoma
- Tovorafenib Approved for Some Children with Low-Grade Glioma
- Genetic Signature May Help Tailor Treatment for Meningioma
- Engaging People with Low-Grade Glioma in Cancer Research
- Targeted Drug Combo May Change Care for Rare Brain Tumor Craniopharyngioma
View the full list of brain cancer research results and study updates.