Types of mastectomy
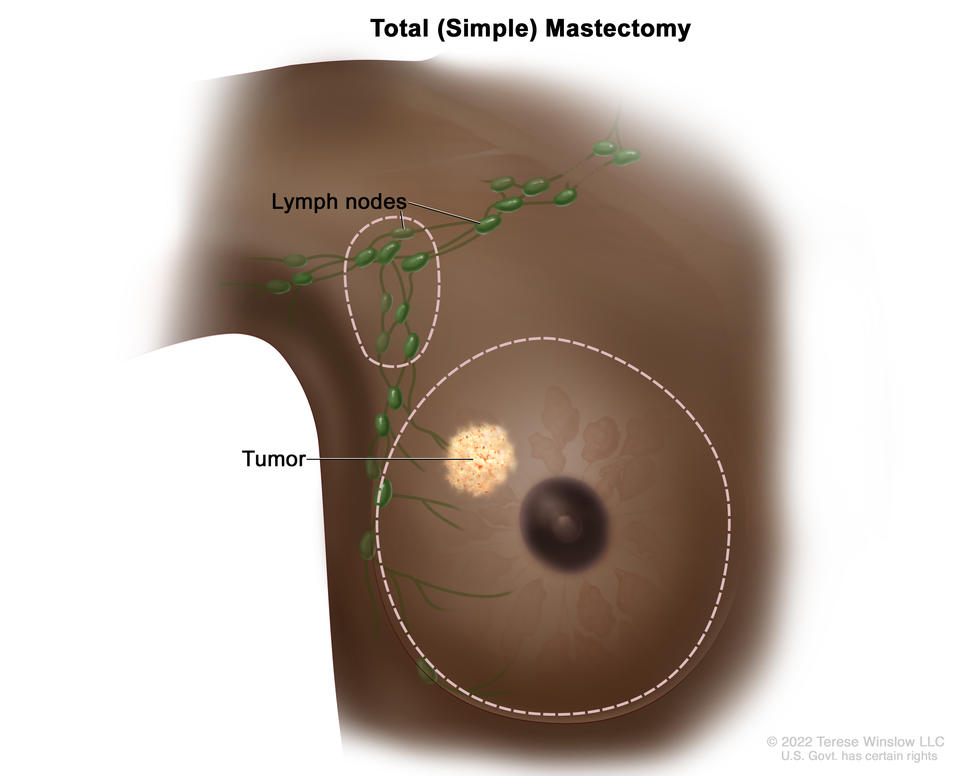
- Total mastectomy (also called simple mastectomy). In this type of surgery, the surgeon removes your whole breast, including the nipple, areola, breast tissue, and skin. Sometimes, they also remove one or more of the lymph nodes under your arm in a procedure called sentinel lymph node biopsy.
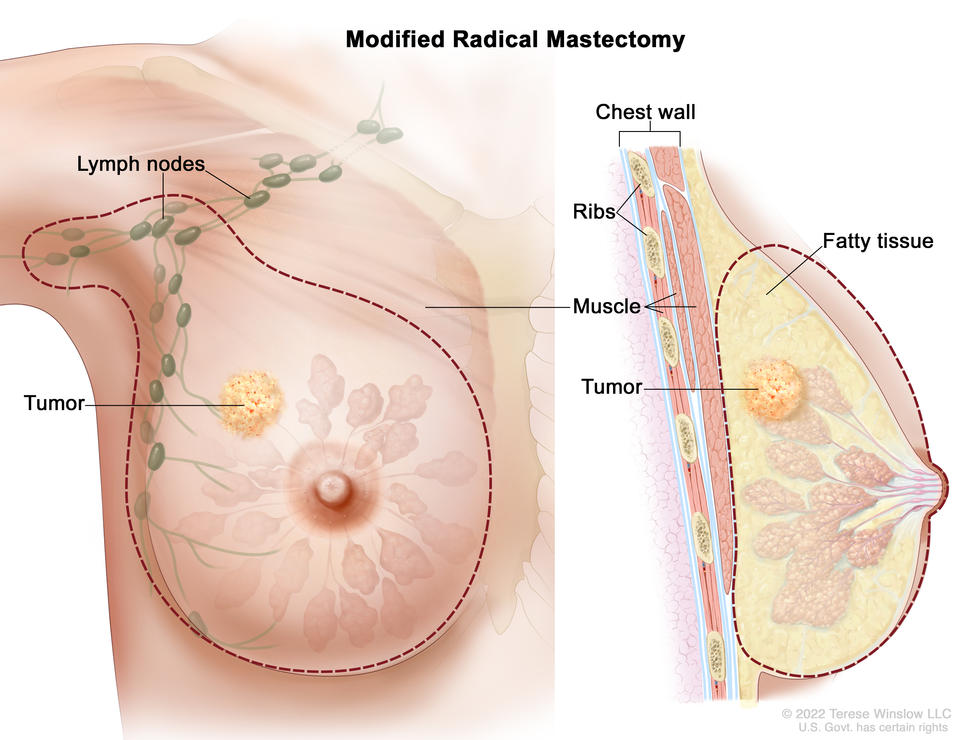
- Modified radical mastectomy. This is the same as a total mastectomy, but the surgeon also removes lymph nodes under your arm (axillary lymph node dissection). Because cancer cells may spread to the lymph nodes, lymph node removal can help reduce the risk of the cancer coming back. But it is often used only for more advanced stages of breast cancer.
- Skin-sparing mastectomy. The surgeon removes the whole breast, as in a total mastectomy, but leaves the skin. A skin-sparing mastectomy leaves less scarring and makes for a more natural-looking reconstructed breast. But if the tumor is large or near the skin, this procedure may not be an option. Skin-sparing mastectomies require breast reconstruction right after surgery.
- Nipple-sparing mastectomy. The surgeon removes the whole breast but leaves the skin, nipple, and areola. Nipple-sparing mastectomy may not be an option if the tumor is large or if cancer cells are found near the skin, nipple, or areola. It also may not be an option for people with larger breasts.
- Radical mastectomy. This type of mastectomy was common in the past, but it is now rarely performed because it does not improve how long people live. It involves removing the chest wall muscles and all lymph nodes, as well as the whole breast, nipple, areola, and skin. A surgeon may still suggest a radical mastectomy if the cancer cells have spread to the chest wall muscles.
Single vs. double mastectomy
In a single (unilateral) mastectomy, only the breast with cancer is removed. A double (bilateral) mastectomy involves the removal of both breasts.
Your doctor may suggest a double mastectomy if:
- cancer is in both breasts
- you have cancer in one breast but are at high risk of developing cancer in the other breast because of a genetic mutation or strong family history of breast cancer
If you do not have a genetic mutation or strong family history of breast cancer, you do not have an increased risk of developing a new cancer in the other breast. For you, research shows that having a double mastectomy instead of a single mastectomy does not help you live longer.
You may choose to have a double mastectomy, even if your doctor suggests a single mastectomy, if:
- you want to reduce the risk of developing a new breast cancer in the healthy breast
- you prefer not to have routine screening to check for cancer in the healthy breast
- you want both breasts to be the same size
- you are concerned about how your chest will look after a single mastectomy
Discuss insurance coverage and the risks and benefits of a double mastectomy with your doctor before making a decision.
Mastectomy with breast reconstruction surgery
You can have breast reconstruction at the same time as the mastectomy, or at any time after. Some types of mastectomies (skin- and nipple-sparing) require reconstruction at the same time. Breast reconstruction is done by a plastic surgeon with experience in this type of surgery. The surgeon uses an implant or tissue from another part of your body to create the breast mound after the breast has been removed. If your nipple is removed, the surgeon may also make the form of a nipple and add a tattoo that looks like the areola.
For more information about types of breast reconstruction, recovery times, and possible complications, visit Breast Reconstruction After Mastectomy.
Going flat after a mastectomy
You may choose to not have breast reconstruction after a mastectomy. This is called “going flat.” If you decide against reconstruction, you have the option of wearing a breast prosthesis to create the breast form under your clothes. To make the chest flat and smooth after a mastectomy, the surgeon will perform an aesthetic flat closure.
Recovering after a mastectomy
Recovery after a mastectomy depends on the type of mastectomy you had and whether you had breast reconstruction. Most people begin returning to normal activities 4 weeks after surgery. But recovery could take longer for people who have breast reconstruction.
Mastectomy risks
As with any surgery, a mastectomy has possible risks:
- infection
- pain or other discomfort that may or may not get better over time (postmastectomy pain syndrome and phantom breast syndrome)
- arm and shoulder pain and stiffness
- lymphedema in the arm, especially when many lymph nodes have been removed
Mastectomy with reconstruction has additional risks. Learn more at Breast Reconstruction After Mastectomy.