Prevention of Liver Cancer
There are several types of liver cancer in adults. The two most common types are hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC). ICC is cancer that occurs in parts of the bile ducts within the liver. It is sometimes considered a type of bile duct cancer.
HCC is the most common form of liver cancer among adults in the United States. The survival rates of both HCC and ICC are low.
Several conditions can increase your chances of developing HCC or ICC. Researchers are testing ways to prevent and treat some of these conditions.
Cirrhosis
The most important risk factor for HCC is cirrhosis, a disease that occurs when scar tissue forms in the liver and prevents it from working correctly. NCI’s HCC Early Detection Strategy Study, a long-term study that followed people with cirrhosis, found that about 2 to 3 of every 100 people developed the disease each year.
Through NCI’s Cancer Prevention Clinical Trials Network, several studies have tested whether drugs used to treat other diseases can prevent cirrhosis from advancing to liver cancer. For instance, a study found the best dose of a cancer drug called erlotinib (Tarceva) for follow-up studies on the prevention of liver cancer. Another study, awaiting results, tested green tea polyphenols. And an ongoing study is testing a cholesterol-lowering medication (statin).
Metabolic Dysfunction-associated Steatohepatitis (MASH)
MASH (formerly called nonalcoholic steatohepatitis or NASH) is a common liver disease that can cause cirrhosis and may lead to liver cancer. MASH is the most severe form of nonalcoholic fatty liver disease, where there is more fat than normal in the liver. In 2021, a clinical trial showed that the weight loss drug semaglutide resolved MASH in most patients.
Hepatitis Virus Infection
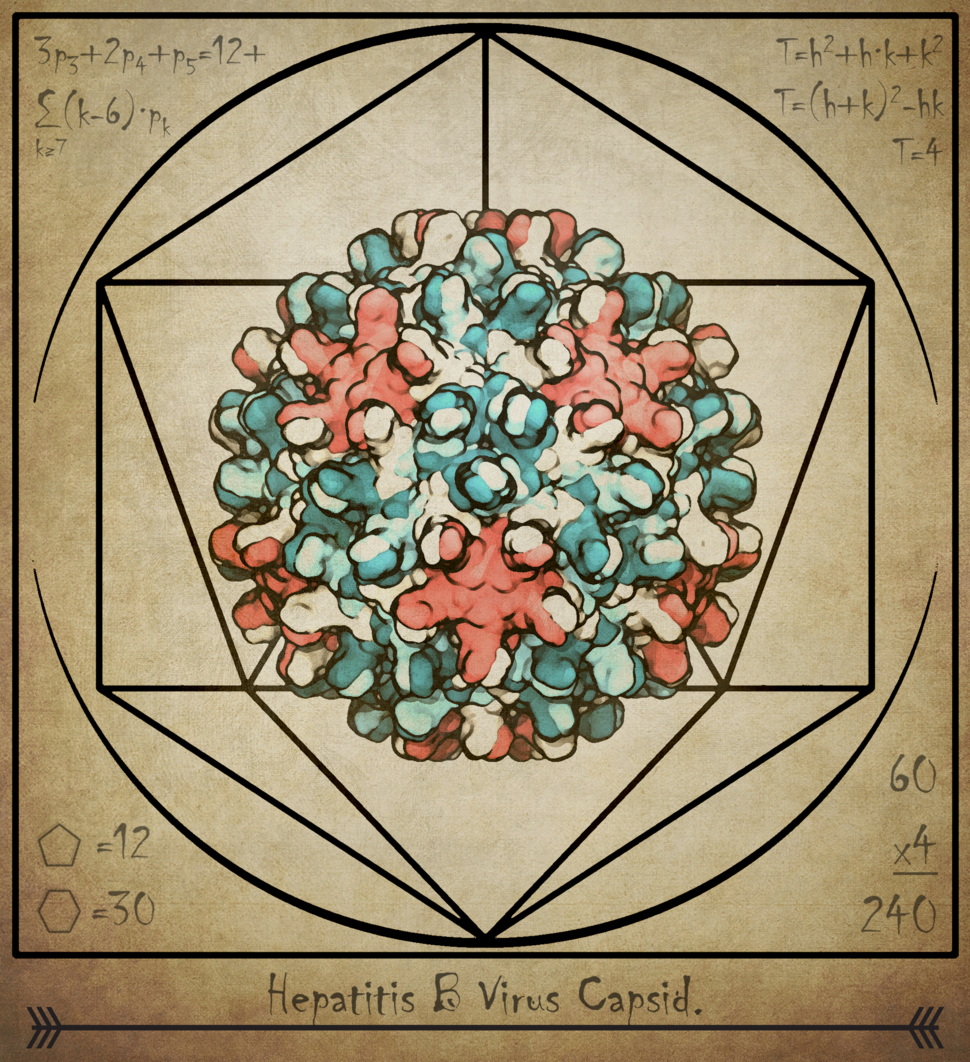
Another common risk factor for HCC is chronic infection with hepatitis B virus or hepatitis C virus. Infection with hepatitis B virus can be prevented by vaccination. There is no vaccine for hepatitis C virus, but researchers are working on developing and testing one.
Chronic infection with hepatitis D virus, which can only be contracted by people infected with hepatitis B virus, may also increase the risk of HCC. Vaccination again hepatitis B virus also prevents infection with hepatitis D virus. NCI's Liver Cancer Program recently completed a study in Mongolia that helps explain how infection with the hepatitis D virus increases risk of HCC among people infected with hepatitis B virus.
Inflammation
Inflammation of the colon (colitis) and inflammation of the bile ducts (primary sclerosing cholangitis) increase the chances of developing ICC. NCI researchers recently found preliminary evidence that these conditions may make gut bacteria leak into the liver, leading to a buildup of certain immune cells that help ICC grow. Scientists think that blocking these gut bacteria or immune cells might be a way to prevent ICC.
Sex Hormones
In the US, liver cancer is more likely to be diagnosed in men than women, but scientists don’t know why. In a large study looking at blood tests from more than 380,000 people, NCI researchers found that higher levels of both androgens and estrogens were linked with liver cancer in men. These findings add to evidence from an earlier NCI study that looked at sex hormones and HCC risk among women. Research is underway to explore how sex hormones might influence liver cancer risk.
Early Detection of Liver Cancer
Liver cancer that is diagnosed at an early stage has a good chance of being cured with surgery, liver transplantation, or treatments such as radiofrequency ablation. Several imaging and blood tests are being studied to see if they can detect liver cancer at an early stage, especially among people who are most at risk for liver cancer.
Screening and Surveillance
The National Liver Cancer Screening Trial is an NCI-supported clinical trial comparing two kinds of liver cancer screening tests in more than 5,000 people with cirrhosis or chronic hepatitis B infection. Half of the participants will be screened with an ultrasound exam of the liver plus a test for a blood-based biomarker called alpha-fetoprotein. The other participants will get screening with a test called GALAD, which takes into account levels of three blood-based biomarkers, plus the person’s age and sex.
People who have liver diseases like cirrhosis or NASH and are at increased risk of getting HCC often receive regular ultrasound exams of the liver, sometimes with a blood test for alpha-fetoprotein. This close monitoring is often referred to as liver cancer surveillance.
There are many challenges with surveillance tests. For example, doctors cannot always tell which patients are at high risk for HCC and may benefit from surveillance. The test results are not always accurate. There is also a financial burden associated with surveillance. Sometimes it is hard for people to get to a clinic for the tests. Likely, as a result of those challenges, there is mixed evidence on whether having these tests regularly prevents people from dying of liver cancer.
Researchers from NCI's Translational Liver Cancer (TLC) Consortium are working to improve early detection of liver cancer. In one study, TLC-supported researchers are evaluating ways to identify which people with cirrhosis are at highest risk of HCC. They are also trying to determine how best to monitor people at higher risk, such as those with small liver masses. Another TLC-supported study is exploring whether the combination of MRI and a blood test called a liquid biopsy can detect HCC in people with cirrhosis. TLC-supported researchers are also using machine learning to combine multiple factors and predict HCC risk in people with cirrhosis.
Imaging
Small, early-stage liver tumors can be difficult to detect on an ultrasound exam, especially for people who have obesity or cirrhosis. Scientists are developing new kinds of imaging tests that may be better at detecting small tumors.
For example, NCI scientists are testing the use of a radioactive substance, called a radiotracer, that may help doctors see specific parts of the body. The scientists are learning if the radiotracer may be better able to find HCC than standard imaging.
Biomarkers
A biomarker is a molecule found in blood or other tissues that serves as a sign of a condition or disease. Scientists are working to find biomarkers in blood, urine, or other body fluids that are reliable signs of early-stage liver cancer.
Scientists in NCI’s Early Detection Research Network (EDRN), a network of institutions researching biomarkers for early-stage cancer, identified several promising biomarkers of early-stage liver cancer that were further studied in NCI’s HCC Early Detection Strategy Study, a long-term study of people with cirrhosis. Investigators found the biomarkers in blood samples from people who developed liver cancer a year later. It is these biomarkers, along with age and sex, that are being evaluated as a screening test in the National Liver Cancer Screening Trial.
NCI also led a study of Baltimore residents to explore genetic features of liver cancer and to find biomarkers for early detection or prevention. Using data from this study, NCI researchers found several potential biomarkers of HCC.
A 2023 study from NCI’s TIGER-LC consortium identified biomarkers in blood that could potentially identify HCC and ICC in people at risk of the diseases. The biomarkers are based on antibodies to various viruses present in blood.
Liver Cancer Treatment
Liver cancer is often diagnosed at an advanced stage. Treatment options for advanced liver cancer include chemotherapy, targeted therapy, immunotherapy, radiation, embolization, and ablation. For more information on treatment options, see our page on liver cancer treatment.
Targeted Therapy
Targeted therapies are drugs that attack molecules that help cancer cells grow, divide, and spread.
Targeted Therapy for HCC
For many years, sorafenib (Nexavar) was the only targeted therapy available for people with advanced HCC. But research has led to the discovery of several newer targeted therapies for HCC, including lenvatinib (Lenvima).
However, most people with advanced HCC don't live for more than 5 years after diagnosis. So researchers are continuing to develop and test treatments that target signaling pathways that drive the growth of HCC cells.
Targeted Therapy for ICC
Several targeted therapies are available for people with ICC that has specific genetic alterations. These include pemigatinib (Pemazyre) and futibatinib (Lytgobi), for tumors with a genetic changes that fuses the FGFR2 gene to another gene—seen in about 15% of people with ICC—and the combination of dabrafenib (Tafinlar) and trametinib (Mekinist), for tumors with a specific mutation in the BRAF gene). Ongoing research in this area includes:
- Clinical trials testing other new targeted therapies for people with ICC who have specific gene changes in their cancer cells. For example, studies are testing targeted therapies such as olaparib (Lynparza) and LY3410738 in people whose ICC or extrahepatic cholangiocarcinoma cells have changes in the IDH1 gene or IDH2 gene.
- Clinical trials testing targeted therapies such as adagrasib (Krazati) for people whose tumors carry genetic changes in the KRAS gene, found in around 12% of people with ICC.
Immunotherapy
Immunotherapy drugs help the body's immune system better respond to cancer. Sometimes combining immunotherapy drugs with chemotherapy or targeted therapy drugs can be more effective than either type of drug alone.
Immunotherapy for HCC
Immune checkpoint inhibitors have become the standard treatment for people with HCC, with several currently approved to treat the disease.
Some examples of ongoing immunotherapy research in HCC include:
- Studying why immunotherapies work for only some people with liver cancer. NCI's Liver Cancer Program has recently identified molecular characteristics linked with survival after immunotherapy treatment for HCC or ICC.
- Efforts by NCI’s Immuno-Oncology Translational Network (IOTN) to explore how the immune system interacts with HCC tumors as they develop and what makes some HCCs more sensitive to treatment with immune checkpoint inhibitors.
- An NCI-supported clinical trial testing a CAR T-cell therapy for adults with advanced HCC. The therapy involves removing a person’s own immune cells and modifying them in a lab so they can better recognize and attack HCC. The goal of the trial is to see if the new therapy is safe.
Immunotherapy for ICC
Immunotherapy is a standard treatment for people with ICC. Scientists are also researching new ways to use immunotherapy to treat ICC. For example:
- In a small clinical trial of people with advanced bile duct cancer, NCI researchers showed that an immunotherapy drug (pembrolizumab [Keytruda]) plus two chemotherapy drugs (CAPOX) shrank or stopped the growth of tumors in more than 80% of patients.
- In a 2021 study of mice with ICC, NCI researchers saw promising results with a combination of two immunotherapy drugs—an immune checkpoint inhibitor and a drug called a CD40 ligand. The researchers have launched a clinical trial of the combination, together with CAPOX, for people with advanced bile duct cancer.
- NCI researchers have also found that people whose HCC or ICC cells that are molecularly similar to each other are more likely to respond to immunotherapies than people whose HCC or ICC cells are diverse. A related study by NCI scientists may explain why: Cancer-killing immune cells were less active in tumors with diverse HCC or ICC cells.
- An NCI-supported clinical trial is testing an investigational immunotherapy drug called PDS01ADC in combination with chemotherapy for adults with ICC.
Radiation Therapy
NCI’s National Clinical Trials Network (NCTN) is supporting two clinical trials of radiation therapy for people with HCC that cannot be removed with surgery.
- One ongoing trial is comparing proton therapy with standard photon therapy. Proton therapy is a new kind of radiation therapy that may cause less harm to healthy tissues.
- The other trial tested sorafenib with a type of radiation therapy called stereotactic body radiation therapy. This approach uses special equipment to position the patient and precisely deliver radiation directly to the tumor, which may cause less harm to the rest of the body. The study found evidence that sorafenib with stereotactic body radiation therapy improves survival compared with sorafenib alone.
Transarterial Therapy
Some liver cancer therapies can be put directly into the blood vessels that feed liver tumors. For example, transarterial therapy, also called transarterial embolization, involves placing small beads into blood vessels to cut off blood flow to the tumor.
Researchers are exploring ways to enhance transarterial therapy, such as using radioactive beads that not only block blood flow but also deliver radiation to the tumor. These therapies are also being studied in combination with targeted therapies and with immunotherapies.
For instance, an NCI-led clinical trial is testing a type of transarterial embolization called TACE plus two immunotherapies (tremelimumab [Imjudo] and durvalumab [Imfinzi]) and a targeted therapy (bevacizumab [Avastin]) as a treatment for people with HCC.
Two similar international trials have found that combining TACE with immunotherapy and targeted therapy improved how long people with HCC lived without their disease worsening.
Transplantation
Some people with early-stage liver cancer can be cured with a liver transplant. Currently, only patients with small tumors in their liver can get a liver transplant. But a 2022 study found that patients who first get treatment to make their tumors smaller can also be cured by a liver transplant.
Precision Medicine
Precision medicine is an approach to patient care that allows doctors to select treatments that are most likely to help patients based on the biology of their tumors.
Biomarkers that are found in tumor tissue (sometimes called tumor markers) may aid precision medicine approaches for liver cancer treatment.
For instance, investigators in NCI’s Center for Cancer Research are studying liver tumors in finer detail to try to identify molecular features that can help guide treatment decisions or lead to more-precise treatments. A 2021 study from NCI’s TIGER-LC consortium identified biomarkers in blood that could potentially help doctors determine how aggressive a patient’s HCC is.
Childhood and Adolescent Liver Cancer Treatment
Several types of liver cancer can develop in children and adolescents. The most common types are HCC and hepatoblastoma. Adolescents are more likely to develop HCC than younger children. Standard treatments for children or adolescents with liver cancer include surgery, chemotherapy, radiation therapy, and ablation therapy.
Adjusting Treatment by Risk Group
Because childhood and adolescent liver cancer is fairly rare, randomized clinical trials of new treatments can be a challenge to conduct. The Children’s Oncology Group, part of the NCI–supported National Clinical Trials Network, is collaborating with other institutions on the first randomized international trial for children with liver cancer, called the Pediatric Hepatic International Tumor Trial (PHITT).
PHITT includes several different studies (or arms) that are using patients’ risk groups (which reflect how likely a patient's cancer is to come back after treatment) to help guide new treatment approaches:
- One study testing whether fewer cycles of cisplatin, which can cause hearing loss at its standard dose, can effectively treat children with low-risk hepatoblastoma who have already had surgery to remove their tumors.
- A study randomly assigning children with intermediate-risk hepatoblastoma to receive cisplatin by itself or cisplatin with other chemotherapy drugs. The outcomes and side effects of the regimens will be compared. The hope is that treatment with cisplatin alone will be just as effective and will lead to fewer side effects and complications later in life.
- A study to see if one chemotherapy combination is better than another at getting rid of tumors in children with high-risk hepatoblastoma.
- A study testing whether adding gemcitabine and oxaliplatin to standard chemotherapy benefits children and adolescents who have HCC that can’t be surgically removed (unresectable) or has spread beyond the liver (metastatic).
Biomarkers of Prognosis
A biomarker is something found in blood or other tissues that serves as a sign of a condition or disease. Prognosis means an estimate of how a disease will affect someone long-term. Doctors can use biomarkers of prognosis to guide treatment decisions.
A specific pattern in the tumor tissue of children with hepatoblastoma, called small cell undifferentiated (or SCU) histology, was once thought to be a biomarker of an aggressive cancer. But a 2021 Children’s Oncology Group-led study found that children with SCU hepatoblastomas actually lived just as long as those without SCU.
PHITT also aims to identify biomarkers of prognosis. Trial researchers are collecting samples of participants’ blood, healthy tissue, and cancer tissue to create the world's largest repository of biological samples from children and adolescents with liver cancer.
By studying these samples, scientists have identified several potential biomarkers. These biomarkers could one day be used to guide treatment decisions for patients with hepatoblastoma.
Fibrolamellar Carcinoma
Fibrolamellar carcinoma, or FLC, is a rare type of liver cancer that usually grows in teens and young adults. Current treatments for fibrolamellar carcinoma include surgery, chemotherapy, and embolization.
A recent study in mice found that a combination of irinotecan and DT2216 showed promise for treating fibrolamellar carcinoma. Irinotecan is a chemotherapy and DT2216 is an experimental drug that gets rid of a protein which helps FLC survive.
NCI’s Pediatric Early Phase Clinical Trials Network (PEP-CTN) is planning to launch a trial testing irinotecan and DT2216 for people with fibrolamellar carcinoma. The clinical trial will first find safe doses of both medications when given together in children with solid tumors. The next part of the trial will enroll only patients with relapsed (came back after previous treatment) or refractory (was unaffected by previous treatment) fibrolamellar carcinoma to see if the drug combination can shrink their tumors.
NCI-Supported Research Programs
Many NCI-funded researchers working at the NIH campus, as well as across the United States and throughout the world, are seeking ways to address liver cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in liver cancer.
Prevention
The Cancer Prevention Clinical Trials Network conducts early-phase clinical trials of drugs and interventions that have the potential to prevent cancer, including liver cancer.
The Liver Cancer Pooling Project (LCPP) is an effort to pool data from different sources to study potential causes of liver cancer. Although there are several known risk factors for liver cancer, not all liver cancers are related to known causes. NCI investigators also use LCPP data to study factors that may protect people from developing liver cancer. For example, a study from LCPP found that people with higher levels of sex hormones (like testosterone) in their blood had a higher risk of developing HCC.
The Thailand Initiative for Genomics and Expression Research in Liver Cancer (TIGER-LC) is a consortium of researchers and clinicians from NCI and Thailand studying genetic differences between HCC and ICC, the most common form of liver cancer in Thailand. The study is designed to address liver cancer prevention, early detection, and treatment.
Early Detection
NCI’s Translational Liver Cancer (TLC) Consortium supports research to improve the early detection of liver cancer. The goals of the consortium are to better define the risks of developing liver cancer, improve surveillance for people who are at high risk of liver cancer, and improve the detection of early-stage liver tumors.
Treatment
The Liver Cancer Program is a multidisciplinary network of researchers and clinicians from across the NIH who are dedicated to improving the early detection, diagnosis, treatment, and health disparities of liver cancer in adults.
NCI’s Immuno-Oncology Translational Network (IOTN) is a network of researchers who are developing new immunotherapies to treat cancer, including liver cancer.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for liver cancer prevention, screening, and treatment.
Liver Cancer Research Results
The following are some of our latest news articles on liver cancer research:
- TACE-Based Treatment Combinations Effective Against Intermediate-Stage Liver Cancer
- Can the New “Omics” on the Block Find Liver Cancer in Blood?
- Seldom-studied immune cells in the liver may be helpful in treating cancer
- Study Tackles Key Questions about Liver Transplants for People with Liver Cancer
- Study Identifies Potential Drug Target to Prevent Some Liver Cancers
- NIH Scientists Develop Blood Test to Help Improve Liver Cancer Screening
View the full list of Liver and Bile Duct Cancer Research Results and Study Updates.