Gene Fusion May Drive Rare Childhood Brain Tumor
, by NCI Staff
Researchers have identified a genetic rearrangement that may drive the development of a rare benign brain tumor in children. The rearrangement, which causes parts of two genes to fuse, may spur the growth of tumors through three distinct biological mechanisms simultaneously, the researchers found.
The study focused on angiocentric gliomas, a rare subtype of low-grade pediatric tumors that was first described less than a decade ago. Fewer than 30 cases have been reported in the scientific literature. Based on their findings, the study authors propose that angiocentric gliomas should be classified as a distinct biologic entity and that the presence of the gene fusion should be used to confirm the diagnosis.
Pratiti Bandopadhayay of the Dana-Farber Cancer Institute in Boston and her colleagues reported their results in Nature Genetics on February 1.
Finding the Gene Fusion
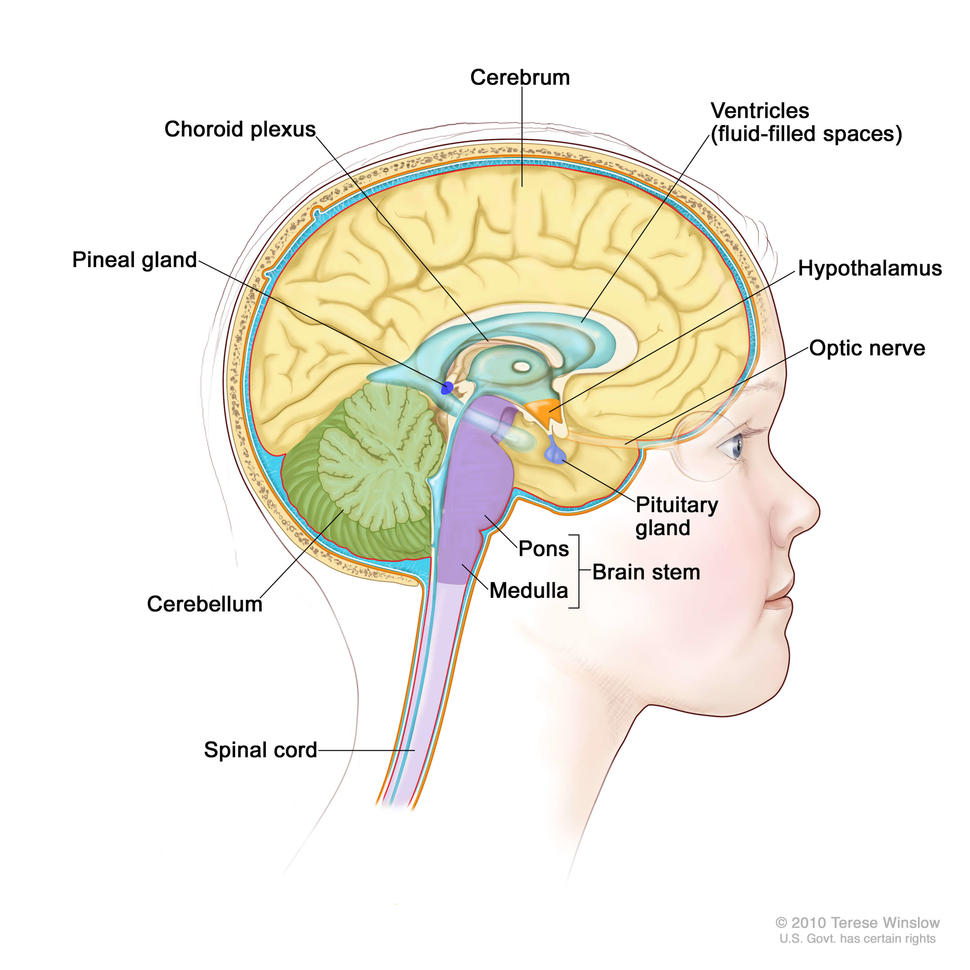
Angiocentric gliomas arise in the cerebral cortex and do not spread to other parts of the body, so surgery is the primary treatment. Although these tumors are benign, they can damage the brain as they grow and cause long-term health problems, including blindness.
To identify genetic alterations associated with these tumors, the researchers analyzed genomic data on 249 pediatric low-grade gliomas, including 19 angiocentric gliomas. The methods of analysis included whole-genome sequencing, RNA sequencing, and exome (the protein-coding regions of the genome) sequencing.
In the current analysis, the researchers detected alterations in the MYB gene in each of the 19 angiocentric gliomas. The MYB gene encodes a transcription factor and is considered a “proto-oncogene,” which means that it can promote the development of cancer if it is altered in certain ways. Genetic rearrangements involving the MYB gene, have been reported previously in patients with angiocentric gliomas.
In at least 7 of the 19 samples, the MYB gene was fused with another gene, and in all but one case the partner was a gene called QKI, which normally functions to prevent cells from becoming malignant, the researchers noted. The MYB-QKI fusion gene was not detected in other types of pediatric low-grade gliomas.
To validate their findings, the researchers analyzed 12 additional angiocentric gliomas. They found MYB gene abnormalities in each sample, confirming the association of MYB alterations with angiocentric gliomas.
Exploring the Biological Mechanisms
Next, the researchers conducted experiments in cells and animal models to better understand how the MYB-QKI fusion gene may drive the development of angiocentric gliomas.
They found evidence for three mechanisms that may act simultaneously. First, the fusion gene codes for a shortened version of the MYB protein that promotes cell proliferation. Second, the altered MYB “feeds back” on the fusion gene to cause its own overexpression. And third, by inactivating one of the two copies of the QKI tumor suppressor gene, the fusion disrupts QK1 protein from keeping tumor development in check.
The results may have implications for understanding other childhood brain tumors, the study authors noted.
“Pediatric tumors are characterized by simple genomes with single driver alterations,” they wrote. “Our findings that one rearrangement contributes to oncogenicity through multiple mechanisms may be applicable to a large number of pediatric tumors."
Test to Distinguish from Other Brain Tumors
Based on the findings of this study, the authors collaborated with Azra H. Ligon, Ph.D., of Dana Farber/Brigham and Women’s Cancer Center to develop the first molecular diagnostic test for these tumors.
The test could help distinguish angiocentric gliomas from tumors that have a higher potential for recurrence or that require further treatment, they suggested. Patients with angiocentric gliomas could be spared the additional treatments such as radiation or chemotherapy that are aimed at preventing tumor recurrence.
“Now we know these angiocentric gliomas have a different biology, and we have an exact way of identifying them so that patients can avoid this additional therapy that has life-long consequences,” said Rameen Beroukhim, M.D., Ph.D., of Dana-Farber in a news release.