Steroids May Limit the Effectiveness of Immunotherapy for Brain Cancer
, by NCI Staff
The use of steroids to manage symptoms of brain tumors, such as the buildup of fluid in the brain, may limit the effectiveness of immunotherapy drugs against these tumors, a new study suggests.
Immunotherapy drugs known as immune checkpoint inhibitors have been effective for some patients with certain types of cancer, including melanoma and lung cancer. But these drugs have generally not been effective against brain tumors, including glioblastoma, the most common type of brain tumor.
Some studies have suggested that the use of the steroid dexamethasone to treat symptoms of brain tumors may hinder the effectiveness of immunotherapy drugs for treating glioblastoma. The new study adds to this evidence.
Using two different mouse models of glioblastoma, the researchers found that mice that received steroids and immunotherapy did not live as long as mice treated with immunotherapy alone, they reported November 25 in Clinical Cancer Research.
When the researchers analyzed data from 163 patients with glioblastoma who received immune checkpoint inhibitors through clinical trials or a compassionate use basis at Dana-Farber Cancer Institute, they found similar results: The use of dexamethasone was associated with shorter survival.
“We know that steroids have potential side effects, but our findings suggest that they also have detrimental effects in terms of diminishing the body’s immune response against a tumor,” said David Reardon, M.D., clinical director of Dana-Farber's Center for Neuro-Oncology, who led the research.
“Our results indicate that the use of steroids in patients with glioblastoma who are receiving immunotherapy needs to be very judicious,” Dr. Reardon said. “We would recommend that such patients be put on the lowest dose of dexamethasone for the shortest possible period of time.”
Dexamethasone and Brain Tumors
Dexamethasone is a highly effective drug for managing symptoms associated with brain tumors, including headaches and weakness, noted Dr. Reardon. It is an immune suppressor that also reduces inflammation. “Dexamethasone is really the only steroid that can effectively decrease inflammatory reactions in the brain to help our patients,” he said.
Some patients receive dexamethasone to prevent inflammation in the brain and remain on the medicine indefinitely. But, based on the new findings, it may be time to reevaluate how dexamethasone is used in brain cancer, the researchers suggested.
“This study underscores the importance of understanding how the drugs we use to treat patients with cancer affect the immune system,” said Masaki Terabe, Ph.D., an investigator in the NIH Neuro-Oncology Branch, who was not involved in the study.
If the immune system is suppressed as a result of treatment with dexamethasone, Dr. Terabe continued, “then treating a patient with a drug that is designed to facilitate an immune reaction against cancer will not be effective.”
In Mice and Humans, Steroids Dampen Immune Response
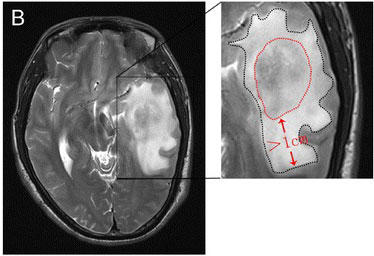
In their study, the researchers used two different mouse models of glioblastoma—one that tends to respond to immunotherapy and another that tends not to. The second model more accurately represents how glioblastoma behaves in humans, the study authors noted.
But the researchers wanted to see whether steroids would diminish the response to immunotherapy even in mice with brain tumors that tend to respond to immunotherapy, explained Dr. Reardon. By treating some mice with dexamethasone and immunotherapy and others with immunotherapy alone, they found that the answer was yes.
And because radiation therapy is a standard treatment for glioblastoma, the researchers also treated both mouse models with radiation and immunotherapy. Among these mice, the use of dexamethasone appeared to be associated with reduced survival.
In addition to the mouse studies, the researchers analyzed data on the 163 patients with glioblastoma who received immunotherapy at Dana-Farber to determine which factors were associated with patient outcomes. Roughly a third of these patients had also received dexamethasone.
The investigators analyzed a variety of factors, including steroid use, the size of the tumor when treatment began, whether the patient was newly diagnosed or had recurrent disease, and age. Of these factors, steroid use was most strongly associated with a patient’s outcome, the researchers found.
“The use of dexamethasone was the strongest negative risk factor for overall survival,” said Dr. Reardon. He cautioned that the findings need to be confirmed in a prospective clinical trial.
Potential Biological Mechanisms
Glioblastomas can evade detection by the immune system through a variety of means, Dr. Reardon noted. “If dexamethasone further impairs the immune system, then by treating patients with the drug we would be shooting ourselves in the foot.”
To identify potential biological mechanisms that could explain how dexamethasone impairs the immune response against tumors, the researchers focused on immune cells called T cells, which are critical for immune responses against tumors.
Treating both mouse models with dexamethasone led to a reduced number of T cells in the animals. “If there are fewer of these T cells to mount an immune response against a tumor, then it’s going to be harder for the immune system to attack a tumor and provide a therapeutic benefit for patients,” said Dr. Reardon.
The mouse studies also indicated that dexamethasone may impair the ability of T cells to generate immune responses. “The steroid may affect both the quantity and the quality of T cell responses,” Dr. Reardon noted.
A related finding—that steroids may affect the development of T cells—was reported in a 2018 study led by Mark Gilbert, M.D., chief of the NIH Neuro-Oncology Branch. Administering steroids before immunotherapy “may blunt the generation of an anti-tumor response,” these researchers concluded.
Future Challenges
The new study, Dr. Gilbert said, “is critical for the field of neuro-oncology and could bring about much-needed changes in the design of future brain tumor immunotherapy trials.”
These studies could help determine the best time during the course of treatment to administer steroids. It may be the case that it is better to wait to administer steroids until after an immune response has developed, Dr. Reardon noted, but he added that more research is needed.
Another challenge will be to develop alternative treatments for inflammation in the brain that do not affect the immune response. “One of the main messages of our study is that we need new ways to manage symptoms in our patients that do not affect the immune response,” said Dr. Reardon.