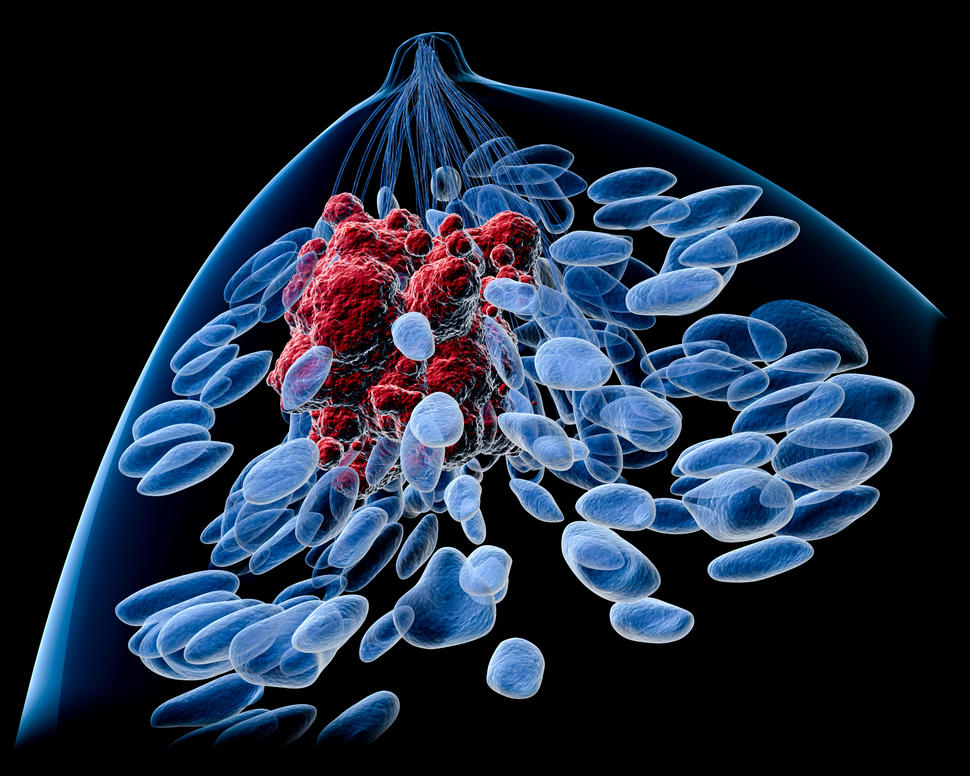
Trial Tests Abemaciclib As New Option for Early-Stage Breast Cancer
, by Carmen Phillips
UPDATE: On October 12, 2021, the Food and Drug Administration (FDA) approved abemaciclib (Verzenio) in combination with endocrine therapy (either an aromatase inhibitor or tamoxifen) following surgery to treat some people with HR-positive, HER2-negative breast cancer. Under the approval, patients’ cancers must have spread to nearby lymph nodes and exhibit certain traits that make the cancer more likely to come back, including high levels of a protein called Ki-67.
The approval was based on 3-year survival results from the monarchE trial (described below). Those results show more than 86% of people treated with abemaciclib and endocrine therapy had not experienced a recurrence after 3 years compared with 79% of those treated with endocrine therapy alone.
FDA also approved a companion diagnostic test called Ki-67 IHC MIB-1 pharmDx for this indication.
Updated results from a large study suggest that the drug abemaciclib (Verzenio) may be a new treatment option for people with the most common type of breast cancer.
Nearly 90% of people diagnosed with breast cancer have early-stage disease. And most of the time the cancer is classified as HR positive and HER2 negative. Although the available therapies for this type of breast cancer are very effective, a portion of patients are at particularly high risk of their cancer returning, or relapsing, in the years following treatment.
The new findings from the study—a clinical trial called monarchE—suggest that for people at high risk of relapse, adding abemaciclib to their treatment regimen may decrease the chances of their cancer coming back.
Participants in the trial who received abemaciclib for 2 years along with standard postsurgical, or adjuvant, hormone therapy were about 30% less likely to have their cancer come back in an invasive form than participants who received the standard adjuvant hormone therapy alone.
The study’s lead investigator, Priya Rastogi, M.D., of the University of Pittsburgh Department of Medicine, reported the findings on December 9 at the San Antonio Breast Cancer Symposium (SABCS).
Overall, the more than 5,600 participants in the trial had good survival outcomes regardless of whether they received abemaciclib. The vast majority experienced no return of their cancer during the short time they were followed. Participants treated with abemaciclib did have a higher risk of some side effects, including a very small number of women who experienced blood clots or inflammation in the lungs.
While oncologists who specialize in treating breast cancer largely agreed that the trial findings are promising, they also noted that it’s not yet clear if abemaciclib is ready for widespread use in patients with early-stage disease.
The early results from the monarchE trial “are clearly encouraging,” said Ruth O’Regan, M.D., of the University of Wisconsin Carbone Cancer Center, who was not involved in the study. “But longer follow-up [of study participants] is crucial,” Dr. O’Regan stressed during an SABCS session on the trial’s findings.
Larissa Korde, M.D., M.P.H., head of Breast Cancer and Melanoma Therapeutics in NCI’s Division of Cancer Treatment and Diagnosis, said that she believes abemaciclib could become an important treatment for some women with high-risk disease. But some significant unknowns remain, Dr. Korde added.
“One unanswered question is whether the treatment is actually preventing recurrences or just delaying them,” she said.
Testing CDK4/6 Inhibitors in Early-Stage Breast Cancer
Largely due to advances in treatment over the past several decades, the long-term prognosis for people diagnosed with early-stage, HR-positive, HER2-negative cancer is generally very good.
Standard treatment includes surgery and radiation, followed by adjuvant treatment with hormone-blocking drugs (also called endocrine therapy) and, for many patients, chemotherapy. In some instances, patients will receive a short course of chemotherapy before surgery, also known as neoadjuvant therapy, to shrink the tumor and improve the chances that it can be completely removed.
The chances of the cancer returning under this general treatment approach are modest. But several factors are known to increase the risk, including whether the cancer has spread to several lymph nodes near the breast (in the armpit), having a large tumor in the breast, and having a higher “grade” cancer, meaning there are certain physical features of tumor tissue (under a microscope) that are indicative of more aggressive cancer.
Another factor that doctors have begun to use in this risk calculation is the percentage of tumor cells in a biopsy sample that express the Ki-67 protein, which is associated with cell division. However, this marker—called the Ki-67 index—is not routinely determined for all patients.
There is an “unmet need” for new treatment options for patients with high-risk disease, Dr. Rastogi said. And that’s where abemaciclib entered the picture.
Abemaciclib is one of three drugs approved by the Food and Drug Administration (FDA) that block the activity of two proteins on cancer cells, CDK4 and CDK6. The two others are palbociclib (Ibrance) and ribociclib (Kisqali). All three drugs are approved to treat advanced or metastatic breast cancer, based on data from large clinical trials showing that they can substantially improve how long patients live without their cancer getting worse.
Based on their effectiveness in treating advanced breast cancer, several clinical trials were launched to see if CDK4/6 inhibitors might fill a treatment gap for people with high-risk early-stage breast cancer.
Positive Results, But Limited Follow-Up
To participate in the monarchE trial, participants had to have evidence of cancer in the lymph nodes nearest to their tumor, as well as at least one of several other disease characteristics linked to an increased risk of the cancer recurring. The trial was funded by Eli Lilly, which manufactures abemaciclib.
Participants were assigned at random to receive standard adjuvant hormone therapy alone or in combination with abemaciclib. Many trial participants also received some form of adjuvant chemotherapy. The median patient follow-up thus far in the trial is approximately 19 months, and only about a quarter of participants have completed 2 years of adjuvant therapy.
The findings reported at the San Antonio meeting included a 3-month update of a planned early (interim) analysis of the trial published in September.
Along with the nearly 30% reduction in the risk of developing invasive cancer in participants who received abemaciclib (called invasive disease-free survival), there was also a similar decrease in the risk of cancer returning as metastatic disease (called distant relapse-free survival).
The development of metastatic cancer is an important indicator for people with early-stage breast cancer, Dr. Korde said, because when it returns in another part of the body, such as the liver or lungs, the cancer is no longer considered to be curable.
Dr. Rastogi also presented results for the subgroup of patients with a high Ki-67 index score. (See Table)
| Patients | Abemaciclib | Standard Therapy | Risk Reduction |
|---|---|---|---|
| 2-Year Invasive Disease-Free Survival | 92.3% | 89.3% | 28.7% |
| 2-Year Distant Relapse-Free Survival | 93.8% | 90.8% | 31.3% |
| 2-Year Invasive Disease-Free Survival High Ki-67† | 91.6% | 87.1% | 30.9% |
† Only includes the 2,498 patients for which Ki-67 was assessed at a central laboratory.
Overall, side effects were more common in the abemaciclib group, leading more of these participants to skip doses of the drug or take lower doses. Nearly 17% of participants in the abemaciclib group stopped taking the drug because of side effects, compared with fewer than 1% of participants in the hormone therapy–only group.
Most of the participants who stopped taking abemaciclib did so within the first 5 months of starting it, Dr. Rastogi explained. And most of those who changed to a reduced dose or skipped doses of the drug have been able to continue taking it, she said.
Blood clots and lung inflammation, both of which can be fatal, occurred in fewer than 3% of people in the abemaciclib group, compared with fewer than 1% in the hormone therapy–only group.
Ready for Prime Time?
Abemaciclib is currently approved by FDA to treat advanced or metastatic breast cancer (alone and in combination with an aromatase inhibitor). It’s not approved to treat early-stage breast cancer but, according to Eli Lilly, the company recently filed for that approval.
However, several breast cancer experts noted that it’s not yet clear how abemaciclib would be used to treat early-stage breast cancer.
In part, that’s because in two other clinical trials involving a similar group of patients, adding the CDK4/6 inhibitor palbociclib to adjuvant hormone therapy failed to improve invasive disease-free survival. Results from one of those trials, called Penelope-B, also were presented at SABCS.
Dr. O’Regan noted several key differences between Penelope-B and monarchE, including different treatment durations: 1 year of palbociclib versus 2 years of abemaciclib.
In addition, the Penelope-B trial results covered a median of 4 years of patient follow-up. However, Dr. O’Regan pointed out that, after 2 years of follow-up in the trial, the magnitude of the difference in invasive disease-free survival between the treatment groups was very similar to the difference reported in monarchE.
That raises the question of whether the improvement in invasive disease-free survival could disappear after the monarchE participants are followed for a longer time, said C. Kent Osborne, M.D., of the Dan L. Duncan Comprehensive Cancer Center at Baylor College of Medicine, during a press briefing.
Dr. Osborne agreed that longer follow-up of monarchE participants will be important, particularly since the cancer in people with early-stage disease can return 5 or 10 years after they’ve completed treatment.
In addition, he noted that CDK4/6 inhibitors are thought to work by stopping or slowing the growth of cancer cells, not by killing them. That’s important, he said, because when these drugs are used in people with advanced cancer, there have been some reports that “tumors seem to grow faster when you stop [treatment].”
If FDA’s approval of abemaciclib is expanded to include early-stage breast cancer, Dr. Korde said, oncologists will need to discuss the pros and cons of this treatment option with their patients.
“As with any therapy, I think the risks of the drugs need to be carefully weighed against the risk of recurrence,” she said. “One could argue that in a very high-risk population, the potential benefit outweighs the risk, but I think this decision needs to be made on an individual basis.”