Vulnerability in Brain Tumors May Open Door to New Treatments
, by Edward Winstead
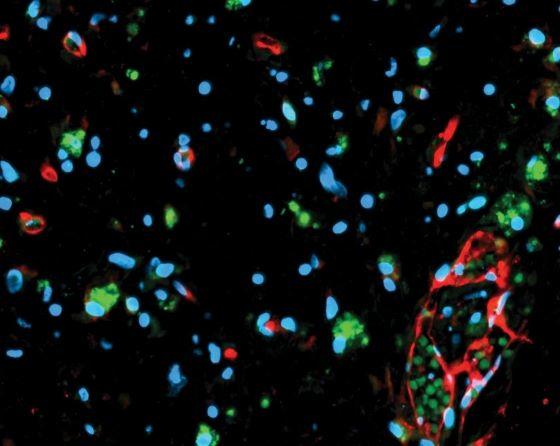
Two new studies have uncovered a vulnerability in different forms of brain tumors that may make the cancers susceptible to the same treatments. The brain tumors are gliomas, which are among the most lethal cancers.
One study focused on diffuse midline gliomas, which occur most often in children. The other study focused on gliomas with mutations in the IDH1 or IDH2 genes, which tend to occur in adults.
Both investigations led to a similar insight: Some gliomas become dependent for their survival on one of the ways that cells produce chemicals called pyrimidine nucleotides, which are components of DNA.
The dependence of certain glioma cells on this process, called de novo pyrimidine nucleotide synthesis, creates a vulnerability. And the new research suggests that a drug may be able to exploit this vulnerability for the benefit of patients with gliomas.
In both studies, a drug called BAY 2402234 penetrated the brains of mice with gliomas and shrank their tumors, though by different mechanisms. Results from the NCI-supported studies were published in Cancer Cell on August 18.
Based on the findings, both teams of investigators are planning clinical trials to test the drug in people with diffuse midline glioma or IDH-mutant glioma.
“This drug prevents the formation of one of the building blocks of DNA, reducing the ability of cancer cells to divide or repair themselves and leading to cell death,” said Mioara Larion, Ph.D., of NCI’s Center for Cancer Research, who studies brain tumors but had no role in the new studies.
The finding that “two vastly different brain tumors share a common vulnerability was unexpected and very interesting,” Dr. Larion continued. “We and others are excited about the possibility of using inhibitors that target certain metabolic pathways to treat patients.”
Desperate need for new treatments
Gliomas are the most common brain tumor among adults. The cancer is usually fatal, and no new drugs have been approved for the disease over the past decade.
“There is a desperate need for new treatments for glioma brain tumors,” said Diana Shi, M.D., of the Dana-Farber Cancer Institute, and a member of the team that conducted the study of gliomas with IDH mutations.
Dr. Shi and her colleagues identified BAY 2402234 while screening hundreds of compounds for their ability to slow the growth of IDH-mutant glioma cells. The drug, which has been tested in people with leukemia, blocks the activity of an enzyme called DHODH, which is involved in pyrimidine synthesis.
In experiments with mouse models, the drug inhibited the growth of IDH-mutant gliomas but not gliomas without the mutations.
In glioma cells, IDH mutations can cause DNA damage when there is an imbalance in the level of nucleotides. These imbalances are caused by blocking pyrimidine synthesis, the researchers found.
They also observed that genes involved in sensing and repairing DNA damage were less active in IDH-mutant gliomas than in gliomas without these mutations.
“We believe that patients with IDH-mutant gliomas may benefit from treatments that target ... DHODH,” said Samuel McBrayer, Ph.D., of the Children’s Medical Center Research Institute at UT Southwestern, who co-led the study with William G. Kaelin, Jr., M.D., of Dana-Farber.
As a next step, the researchers are working to reach an agreement with the developers of BAY 2402234, the Broad Institute and Bayer Pharmaceuticals, to launch a clinical trial of the drug in people with certain types of glioma.
The trial will be sponsored by NCI’s Glioblastoma Therapeutics Network (see box) and will focus on a type of glioma called grade 4 IDH-mutant astrocytoma.
Developing new models of gliomas
A challenge in developing treatments for gliomas has been the limited number of models for assessing how a drug may affect a brain tumor.
“We don’t have a great way to evaluate new drugs before they are tested in patients who have gliomas, and this has been a real bottleneck in the research,” said Kalil Abdullah, M.D., a neurosurgeon who specializes in treating brain tumors at the University of Pittsburgh’s Hillman Cancer Center.
To address this challenge, his laboratory has developed models called surgically explanted organoids, which are tiny 3-dimensional representations of a patient’s tumor. These models are derived from tissue samples collected during brain surgery, and they retain many of the biological characteristics of the original tumor.
In the new study, BAY 2402234 preferentially killed organoids created from IDH-mutant gliomas relative to organoids created from gliomas that lacked the mutations.
“As far as we know, this was the first study to use organoids developed from patients with lower-grade gliomas to evaluate a new drug,” said Dr. Abdullah. “And the results were very promising.”
Urgent need for progress against gliomas in children
As with gliomas in adults, there has been little progress in developing new treatments for gliomas that occur in children. The category of diffuse midline gliomas includes aggressive tumors known as diffuse intrinsic pontine gliomas, which occur most often in children and are almost uniformly fatal.
“There have not been advances of any substance for the treatment of diffuse midline gliomas in many, many decades,” said Daphne Haas-Kogan, M.D., who chairs the Department of Radiation Oncology at Dana-Farber and led the new study of these gliomas.
“The only intervention that works to alleviate the patient’s symptoms is radiation,” she continued. “But radiation is not curative, and therefore every patient with this disease dies.”
To identify new treatments for diffuse midline gliomas, Dr. Haas-Kogan and her colleagues conducted a CRISPR screen, which can reveal genes that are needed for the survival of certain cells. For some diffuse midline gliomas, the de novo pyrimidine nucleotide synthesis pathway appears to be essential, the researchers found. This dependency may arise because an alternate pathway used to produce pyrimidines stops working as it should, they believe.
“We’d like to develop a better understanding of this mechanism,” Dr. Haas-Kogan said. “The work could reveal additional vulnerabilities in these tumors that might point to potential therapies.”
When the researchers tested the drug BAY 2402234 in mouse models of diffuse midline gliomas, it shrank tumors. But the tumors eventually started growing back, and the mice died of the disease.
“The drug prolonged survival in the mice, but it’s not a cure,” said Sharmistha Pal, Ph.D., of Dana-Farber and a coauthor of the study. She noted that many cancers develop resistance to individual therapies, and the researchers are exploring strategies for overcoming drug resistance.
The researchers are planning to test BAY 2402234 in patients with diffuse midline gliomas through the Pacific Pediatric Neuro-Oncology Consortium. The group, which includes more than 20 hospitals around the world, has trials for patients with diffuse midline gliomas that allow for new agents to be added as they are discovered.
Building a strong scientific collaboration
The Cancer Cell studies of gliomas highlight the value of collaboration among researchers who study different types of cancer, noted Amanda Haddock, president of Dragon Master Foundation, a nonprofit dedicated to accelerating cancer research, who had no role in the glioma studies.
These studies began as independent investigations. But several years ago, the research teams began to share information after Drs. Haas-Kogan and Kaelin had a serendipitous conversation at a scientific meeting on gliomas.
After a day of presentations at Cold Spring Harbor Laboratory, the Dana-Farber colleagues met before dinner. As they chatted, each investigator shared the outlines of their glioma research, revealing the existence of parallel studies.
“At that point, we joined forces,” said Dr. Haas-Kogan, who noted that the collaboration accelerated her team’s work. For one thing, Drs. Kaelin and McBrayer had already identified BAY 2402234 as a potential treatment for IDH-mutant gliomas, and Dr. Haas-Kogan was not aware of the drug.
Just as important, Dr. McBrayer’s team had expertise on designing studies of metabolic pathways and interpreting the results. “They shared this knowledge with us over many Zoom calls,” said Dr. Haas-Kogan.
Likewise, Dr. McBrayer said his team benefited from collecting “corroborating evidence from two subsets of brain tumors.” The hope now is that people with gliomas will one day benefit as well.
“Fortunately, these researchers discovered each other and could complement each other’s work,” said Haddock. “This is exactly the kind of collaboration that is in the best interest of the patients, and we need to encourage and reward this type of work.”