Enzalutamide Gets Added Approval for Prostate Cancer That Hasn’t Spread
, by Carmen Phillips
The number of treatment options for prostate cancer has exploded over the last decade. That trend is showing no signs of letting up, with the Food and Drug Administration’s (FDA) recent decision to expand the approved uses of enzalutamide (Xtandi) to treat people with prostate cancer that hasn’t spread, or metastasized, to other parts of the body.
Under this new approval, announced on November 16, enzalutamide can now be used alone, or in combination with leuprolide, to treat nonmetastatic prostate cancer that is castration sensitive.
The new approval also requires that the patient have had an increase in their blood PSA levels after earlier surgery or radiation, known as a biochemical recurrence. However, the approval only applies to those considered to be at high-risk of their cancer spreading.
FDA’s decision was based on the results of a large clinical trial called EMBARK. In the trial, patients treated with the combination of enzalutamide and leuprolide had better metastasis-free survival than those treated with leuprolide (and a placebo). Metastasis-free survival is a measure of how long people live after starting treatment without their cancer spreading or without dying from any cause.
Trial participants treated only with enzalutamide also had better metastasis-free survival than those treated with leuprolide alone.
But the extent to which this new approval and the EMBARK results will, or should, change patient care is still unclear, explained Fatima Karzai, M.D., of NCI’s Center for Cancer Research, who specializes in treating prostate cancer but was not involved in the trial.
For example, Dr. Karzai said, more time is needed to know whether trial participants treated with enzalutamide alone or in combination with leuprolide live longer overall. As a result, this new approval “will garner different treatment approaches” that oncologists recommend to their patients.
Other experts believe the approval will have a substantial impact on patient care. One of the trial’s lead researchers, Stephen Freedland, M.D., of Cedars-Sinai in Los Angeles, said many patients with these high-risk biochemical recurrences will now be treated with the enzalutamide and leuprolide combination.
Dr. Freedland acknowledged that side effects are a concern. “But there are a lot of benefits” to using both drugs together, he added, including “delaying metastasis.” The development of metastases not only requires immediate treatment but also can cause significant pain, particularly when the cancer has spread to the bones.
In addition, Dr. Freedland noted that other analyses from the trial suggests that, overall, treatment with both drugs doesn’t harm people’s quality of life.
From castration-resistant to castration-sensitive localized prostate cancer
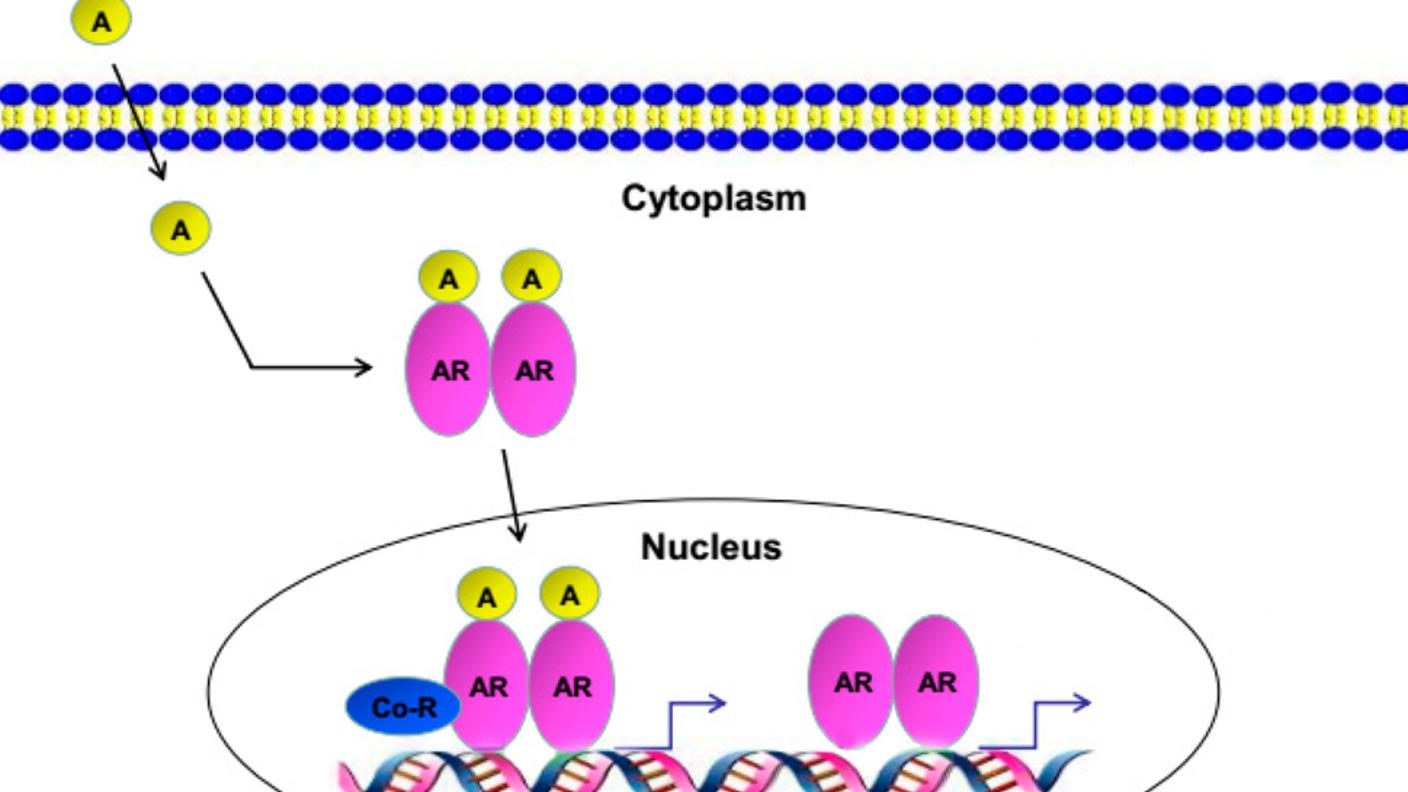
Enzalutamide works by disrupting testosterone’s interaction with cancer cells. It's already approved by FDA to treat nonmetastatic and metastatic prostate cancer, including when the cancer can no longer be controlled with drugs that block testosterone production (like leuprolide), known as castration-resistant disease.
In up to half of people with castration-sensitive localized prostate cancer who previously had surgery or radiation to eliminate the tumor, their PSA levels start to creep up, sometimes rapidly, within 10 years. When any such uptick happens, it may mean that the cancer is starting to grow again in the prostate or that there are small tumors somewhere else in the body.
A key measure that oncologists use to judge whether rising PSA levels are a concern is how long it takes for the levels to double from the time they became detectable again.
When the PSA doubling time is rapid, around 9 months or less, studies have suggested it means those patients are at high-risk of having their cancer spread to other organs.
But how to best address biochemical recurrences—even those with rapid PSA doubling times—has been “a gray zone,” Dr. Karzai explained.
Should treatment begin immediately to prevent the cancer from gaining steam? Or should treatment wait until the patient is experiencing symptoms or for confirmation from imaging scans that the cancer has spread?
Currently, many people with a biochemical recurrence with a PSA doubling time of 9 months or less are started on leuprolide or similar drugs, she said.
The EMBARK trial was designed to try to bring some clarity to the question.
In large clinical trials, enzalutamide improved how long men with castration-sensitive prostate cancer that has already spread live overall. So, with the EMBARK trial, researchers wanted to see if enzalutamide might also improve outcomes in people with prostate cancer that hasn’t spread but that—based on rising PSA levels—may be poised to.
Better metastasis-free survival, time with no treatment
Funded by Pfizer and Astellas Pharma, the manufacturers of enzalutamide, the trial enrolled nearly 1,100 participants who had been treated for localized prostate cancer. All participants had PSA levels that had returned and doubled within 9 months, but with no signs that their cancer had spread.
EMBARK participants were randomly assigned to treatment with both enzalutamide and leuprolide or with either drug alone.
After starting treatment, participants had full-body CT scans and bone scans every 6 months to look for signs that their cancer had returned. Participants whose PSA levels decreased to undetectable levels within 37 weeks could pause treatment. Such breaks are often called “treatment holidays.” Treatment resumed if their PSA levels started to rise again.
Five years after starting treatment, Dr. Freedland and his colleagues reported, about 87% of participants treated with enzalutamide and leuprolide were still alive with no evidence of metastasis, compared with 80% of people treated with only enzalutamide and 71% with only leuprolide. The findings were published in October in The New England Journal of Medicine.
Dr. Freedland noted that, to date, there is a strong statistical trend suggesting that people treated with both drugs also will live longer overall than those treated with leuprolide alone. But participants will have to be followed longer before it’s known for sure.
About 91% of people in the combination treatment group were able to pause treatment because of undetectable PSA levels, compared with 86% in the enzalutamide-only group and 68% in the leuprolide group.
Many patients in all three groups were able to pause treatment for 2 years or more, although the median length of treatment suspension was longest in the combination treatment group (20 months versus 17 and 11 months, respectively).
Side effects and quality of life
There were no surprises in terms of the side effects seen in the trial in people treated with enzalutamide alone or with leuprolide. That said, side effects were common and sometimes serious in all three treatment groups.
In the enzalutamide–leuprolide group, the most common side effects were hot flashes, fatigue, and muscle aches, although many of these were also common in the leuprolide alone group. In the enzalutamide–alone group, the most common side effects include hot flashes, fatigue, and enlarged breasts. Severe side effects were not frequent in any of the groups and were generally higher in those treated with enzalutamide.
In an editorial that accompanied the trial results, Ana Aparicio, M.D., who specializes in treating prostate cancer at the University of Texas M.D. Anderson Cancer Center, noted that of the trial participants who died, potentially up to 60% were from causes other than prostate cancer.
The large number of noncancer deaths can point to a problem called overtreatment—that is, treatment that was not likely to extend or improve a person’s life.
“The extent to which the cancer treatments contributed to these deaths is unknown,” Dr. Aparicio wrote. “But even if there was no association, their frequency arguably diminishes [the treatments’] potential benefit.”
Nevertheless, she concluded, the results show that, at least for some patients, the upside of “early cancer control” with enzalutamide alone or combined with leuprolide “outweigh[s] its risks.”
According to a separate analysis from EMBARK published in October in NEJM Evidence, treatment with enzalutamide and leuprolide did not appear to decrease EMBARK participants’ quality of life, Dr. Freedland noted.
The prospect of a prolonged treatment holiday is also an important consideration, he continued.
“After 8 or 9 months of therapy, if you do really well, we stop [treatment],” he said. “It’s not years and years of treatment. We’re going to be very aggressive for a period, and if you do well, chances are really high you’ll reach that [suspension] threshold.”
Treatment decisions in the era of PSMA-PET
The first participants in EMBARK were enrolled more than 8 years ago. Since that time, an imaging technology used specifically in people with prostate cancer, called PSMA PET, has emerged. This form of PET imaging can detect tumors missed by conventional PET imaging, which was used in the EMBARK trial.
In a study presented in June 2023 at American Society of Clinical Oncology annual meeting, in fact, researchers showed that, based on PSMA-PET findings, many people with biochemical recurrences with rapid PSA doubling times actually had small tumors either in and around the prostate or elsewhere in the body.
Use of PSMA-PET has expanded rapidly in the United States, so questions have been raised about how it should alter how people interpret the EMBARK results and—with this new approval—apply its findings in everyday patient care.
Although PSMA-PET scans can find small tumors missed by standard imaging (PET and bone scans), Dr. Karzai said, “it remains unclear whether early identification will alter the course of a patient’s disease.” In other words, a small tumor somewhere in the body may not grow or spread soon, if ever.
More research is needed on how to apply PSMA-PET imaging findings to decisions about treatment, Dr. Freedland said.
But, even in the absence of PSMA-PET results, he added, factors such as patient age, their overall health, and how they weigh the potential benefits of different treatments versus their risk will all come into play.
“While we don’t expect 100% of patients will go on [the combination treatment], it’ll be interesting to see how physicians and patients interpret these data and make decisions in the real world,” Dr. Freedland said.
For the time being at least, Dr. Karzai said, good doctor–patient communication about treatment options will be important.
“Clinicians will need to have balanced conversations with patients about the benefits of treatment when compared to the side effects” of both drugs, she said.