India’s First Homegrown CAR T-Cell Therapy Has Roots in NCI Collaboration
, by Linda Wang
In 2015, Alka Dwivedi, then a graduate student at the Indian Institute of Technology (IIT) Bombay, began wondering whether a CAR T-cell therapy could be made in India.
At the time, several CAR T-cell therapies—a type of immunotherapy in which a person’s T cells are modified in a laboratory to selectively kill cancer cells—were being tested in clinical trials in the United States. And although CAR T-cell therapies looked to be promising treatments for blood cancers like leukemia and lymphoma, they could have serious side effects and were expected to carry a high price tag once approved for use.
Both issues, she felt, meant that these cutting-edge treatments—at least in the form in which they were being produced at the time—wouldn’t be a viable option for many people in low- and middle-income countries like India. Dr. Dwivedi and her colleagues envisioned designing a different CAR T-cell therapy, one that could be produced in, and meet the needs of, people with cancer in their country. But they knew they couldn’t do it alone.
Over the next several years, Dr. Dwivedi (who earned her Ph.D. in 2021) embarked on a collaborative journey that brought her and colleagues Rahul Purwar, Ph.D., of IIT Bombay, and Gaurav Narula, M.D., of Tata Memorial Centre in Mumbai, to the National Institutes of Health (NIH) Clinical Center in Bethesda, Maryland.
During their time at the NIH Clinical Center, this team shadowed leading experts in CAR T-cell therapy at NCI’s Center for Cancer Research. The training provided by NCI scientists—including Nirali Shah, M.D., who studies CAR T-cell therapies for children with blood cancers—proved invaluable, Dr. Dwivedi said. The visit helped guide Dr. Dwivedi and her co-investigators in designing an effective CAR-T cell therapy, actalycabtagene autoleucel (NexCAR19), that could be manufactured in India, made available at a reasonable cost, and meet the needs of patients in India’s health care system.
In October 2023, India’s counterpart to the US Food and Drug Administration, the Central Drugs Standard Control Organization, made NexCAR19 India’s first approved CAR-T cell therapy.
The approval was based on the results of two small clinical trials conducted in India in 64 people with advanced lymphoma or leukemia. According to trial results presented in December 2023 at the American Society of Hematology meeting, 67% of patients (36 out of 53) in the two trials had a notable decrease in the extent of their cancer (objective response), with the cancer disappearing altogether in about half (complete response).
ImmunoACT, a spin-off company of IIT Bombay, funded the trial and will be manufacturing actalycabtagene autoleucel and bringing it to market.
“This is a big achievement for India,” said Dr. Dwivedi, who is now continuing her training in NCI’s Center for Cancer Research. “It’s the team effort that brought us here.”
“This is like a dream come true and an incredible win for the patients in [India],” Dr. Purwar, who was Dr. Dwivedi’s graduate advisor at IIT Bombay and is founder and CEO of ImmunoACT, said in a statement. “Now our patients in India and [other] countries with limited resources will have access to this lifesaving drug at an affordable cost.”
Designing an indigenous CAR T-cell therapy
In India, cancer is rapidly becoming a much bigger public health problem than it once was. According to the most recent estimates, new cancer diagnoses in the country reached nearly 1.6 million in 2023, up from about 980,000 in 2010. And 800,000 people are estimated to die from cancer each year, a number that is expected to grow substantially in the coming decades.
Despite this expanding burden of cancer in India, many new cancer treatments are inaccessible because of their high cost and the general lack of insurance coverage among people in India. In addition, some treatments, including CAR T-cell therapy, can cause severe side effects that must be treated in a hospital, further driving up the costs of treatment and requiring access to a nearby hospital, which isn’t the case for many people in the country.
In the United States, six CAR T-cell therapies have been approved to treat blood cancers, primarily lymphomas and some forms of leukemia, and, most recently, multiple myeloma. But these approved therapies all contain antibody fragments derived from mice, which can trigger severe side effects as a patient’s immune system tries to reject the foreign substance.
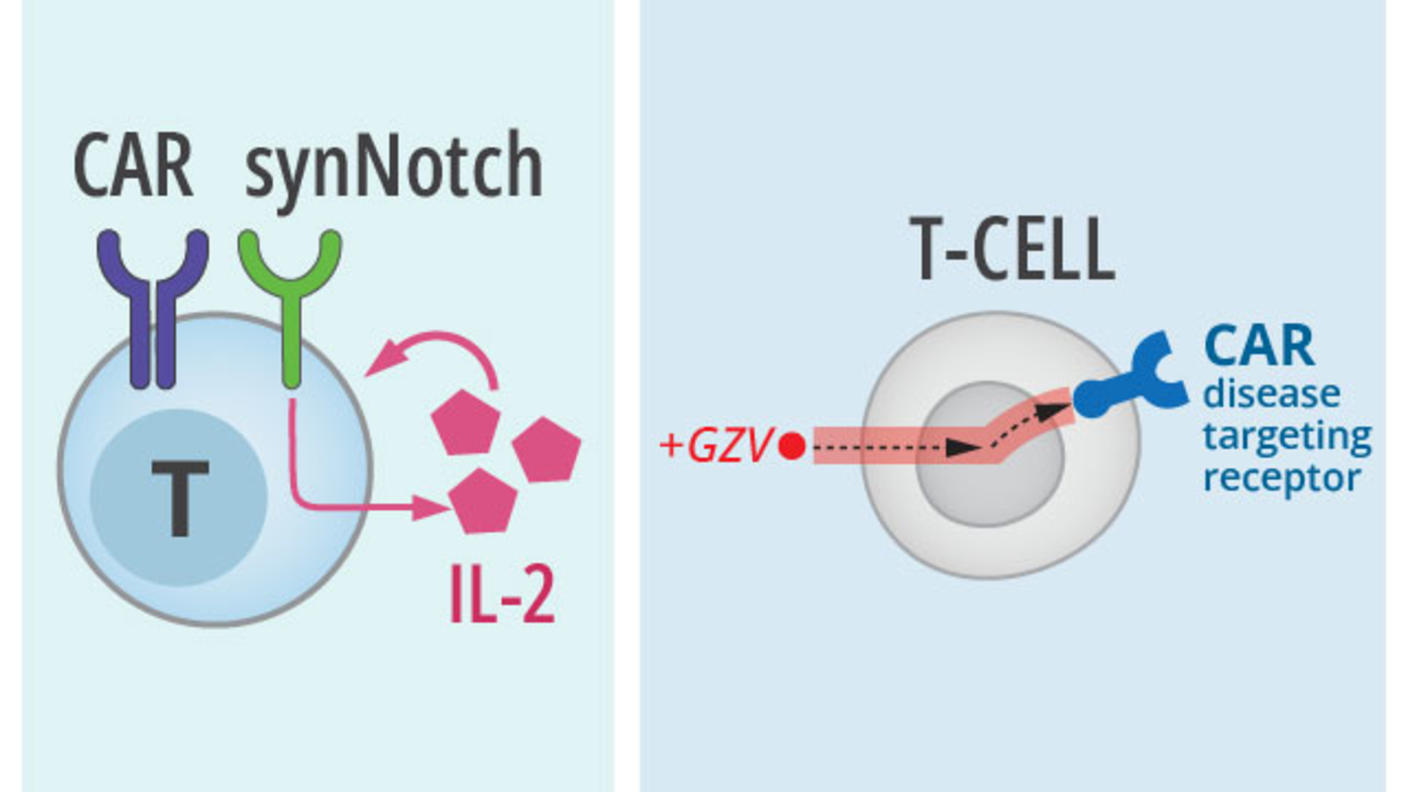
Using a similar approach to one being pursued by research groups in the United States and elsewhere, Dr. Dwivedi and her colleagues tried modifying CAR T cells to carry a more human-like antibody. They hoped that this “humanized” CAR T-cell therapy would escape immune system attack.
But their initial attempts at designing such a CAR T cell did not work, and they couldn’t figure out why. That’s when they decided to seek outside guidance.
“We thought we should come to NCI and get trained,” Dr. Dwivedi said.
Learning from the leaders
The researchers came to NCI near the end of 2017 through a visiting scientist program sponsored by NCI’s Center for Global Health. In addition to working with Dr. Shah, Terry Fry, M.D., and their colleagues to learn more about designing CAR T cells, the group also worked with Steven L. Highfill, Ph.D., David F. Stroncek, M.D., and their team from NIH’s Center for Cellular Engineering to get advanced training on manufacturing cellular therapies.
“They wanted to learn the entire process,” said Dr. Shah. That included everything from how to manufacture CAR T cells that are of high-enough quality to be used in humans to how to design a clinical trial to test their therapy.
Dr. Dwivedi said that the experience of shadowing NCI scientists was a turning point for her team. When they returned to India, they successfully manufactured several versions of a humanized CAR T-cell therapy. Dr. Shah and her NCI colleagues also made numerous trips to India to help the IIT Bombay/Tata team as they moved through the manufacturing process.
When Dr. Dwivedi and her colleagues tested the different versions in lab and animal studies, one stood out for its ability to kill cancer cells while limiting the immune-related reactions that can lead to severe side effects. Actalycabtagene autoleucel, like most of the CAR T-cell therapies approved in the United States, targets CD19, a protein that is often produced in large amounts on the surface of leukemia and lymphoma cells.
With what appeared to be a promising treatment in hand, it was time to take the next big step: clinical trials.
Impressive clinical trial results
On June 4, 2021, a patient at Tata Memorial Hospital in Mumbai received the first infusion of actalycabtagene autoleucel, the CAR T-cell therapy that would become NexCAR19. This first part of the clinical trial only included 14 patients, all of whom had B-cell acute lymphoblastic leukemia that had returned or did not respond to standard treatments.
Based on promising results from the first 14 patients, a somewhat larger trial was quickly launched. The combined trials included 64 people with B-cell lymphoma or leukemia.
At the American Society of Hematology meeting, ImmunoACT cofounder Atharva Karulkar, Ph.D., and Hasmukh Jain, M.D., of Tata Memorial Centre, who led the clinical trial, presented data from the trials. Among 53 patients who could be evaluated (38 with lymphoma and 15 with leukemia), 26 of 38 patients with lymphoma (68%) and 10 of 15 patients with leukemia (72%) responded to the treatment. All of the responses in the leukemia group were complete responses—that is, they had no signs of cancer.
None of the 53 participants had the neurologic side effects that are often seen in people treated with the CAR T-cell therapies approved in the United States, and only a small portion (5%) had a severe form of an immune-relate side effects known as cytokine release syndrome.
Only five patients required hospitalization because of side effects. A pediatric trial in B-cell acute lymphoblastic leukemia is ongoing.
A model for global team science
Dr. Karulkar noted during his presentation that, in the United States, an infusion of CAR T-cell therapy costs about $400,000. By contrast, NexCAR19 is expected to cost around $50,000. ImmunoAct will manufacture the CAR T cells in a facility that’s being built in Mumbai and has plans to develop additional manufacturing sites across India. Initially, their hope is to treat around 1,200 patients a year.
“It is remarkable that they were able to generate a brand new CAR T-cell [therapy] that matched the results … being seen in the United States,” Dr. Shah said. “The fact that they have been able to keep the costs low and come up with a [treatment] that is relatively well tolerated—which is important for the patient population they're going to be treating in India—means that they’re going to [improve] the lives of so many people.”
Dr. Shah pointed out that this achievement goes far beyond developing India’s first CAR T-cell therapy. Through this collaborative effort, Dr. Dwivedi and her colleagues have built something that other low- and middle-income countries can model.
“What Dr. Dwivedi and the team there developed is an entire [cellular therapy] infrastructure,” Dr. Shah said. They’ve proven to public health agencies in other countries that they too are “able to now build [these therapies] from the bottom up.”