Persistence of Genetic Mutations after Chemotherapy Linked to Poor Outcomes in Some Patients with AML
, by NCI Staff
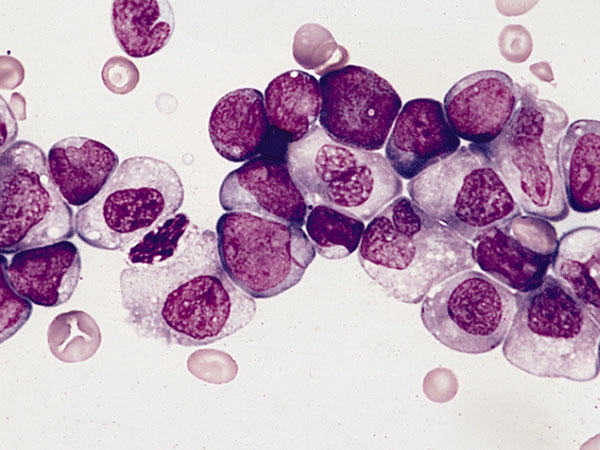
Patients with acute myeloid leukemia (AML) who achieved remission, but who had bone marrow cells that continued to exhibit leukemia-associated genetic mutations 1 month after the initiation of chemotherapy, had a substantially increased risk of relapse and reduced survival, according to a new study.
Published August 25 in the Journal of the American Medical Association (JAMA), the study showed that identifying the full set of leukemia-related mutations in AML cells at the time of diagnosis was no better at predicting disease relapse than current standard of care methods. However, the persistence of mutations after chemotherapy was associated with an increased risk of relapse and shorter survival.
Although the treatment of AML—a cancer of the blood and bone marrow—has improved in recent years, 20 percent of patients do not achieve a remission after initial, or induction, chemotherapy, and nearly half of those who do go into remission eventually see their cancer return. But there has not been a good way to identify which patients are most likely to relapse.
These new findings, the study authors wrote, "begin to define a genomic method" for identifying patients at increased risk of their disease returning after chemotherapy that appears to have induced long-term remission.
Earlier Studies Provide Clues
Although bone marrow transplantation can cure many patients with AML, it carries a risk of serious complications. So it is important for physicians to identify the patients most likely to benefit from a transplant based on their risk of recurrence. Although there are established clinical factors that can identify patients at high risk and low risk of relapse, the majority of patients are classified as intermediate risk based on several genetic characteristics of their cancer cells, and researchers have struggled to uncover other measures that can accurately identify those in this intermediate risk group who are at increased risk of relapse.
For years, the study's lead author, Timothy Ley, M.D., of Washington University in St. Louis, and his research team have been using genome sequencing approaches to identify potential mutations associated with AML that may inform prognosis. But, surprisingly, the researchers have found that few of the mutations they detected were associated with the risk of recurrence or other outcomes.
"We looked at everything, including all of the noncoding regions of the genome, and really, none of it was terribly informative," Dr. Ley said. "So that was pretty disappointing."
But in retrospect, he continued, it began to make sense. Tumors are composed of groups of cells, each of which carries a different set of mutations. These groups of cells, or subclones, "are important because they can contribute to relapse," said Dr. Ley. "[Different] subclones have different responses to chemotherapy. And we don’t know the genetic rules that define those responses."
Finally, the researchers "took a hint from the cytogeneticists," Dr. Ley said, by looking back to two earlier studies that had found that if bone marrow cells that carry clonal cytogenetic changes associated with the cancer persisted after initial chemotherapy, patients were more likely to relapse. But because AML cells with normal cytogenetics still harbor oncogenic mutations, Dr. Ley and his team wondered whether the persistence of genomically defined mutations after chemotherapy would provide a more accurate way to classify patients according to their risk of recurrence.
Persistent Mutations Help with 'Molecular Monitoring'
In the JAMA study, Dr. Ley’s team conducted exome sequencing of bone marrow samples collected from 50 adult patients with AML who had achieved a complete morphologic remission—defined as a return to normal blood cell counts and the absence of abnormal-looking cells—following induction chemotherapy. They wanted to see whether leukemia-associated mutations identified via sequencing prior to chemotherapy persisted after treatment. They analyzed samples collected both when patients were initially diagnose, and about 30 days after induction chemotherapy, which is when the bone marrow has recovered from treatment. Thirty-two of the 50 patients had been classified as intermediate risk based on traditional cytogenetic measures.
Patients who still had even a single leukemia-associated mutation 30 days after induction chemotherapy had a median event-free survival of 6.0 months and median overall survival of 10.5 months. In contrast, among patients whose treatment had cleared the bone marrow of all detectable cells harboring these mutations, median event-free survival was 17.9 months and median overall survival was 42.2 months. Similar results were observed for the 32 patients who were classified as intermediate risk.
The findings "provide critical insights into the role of molecular monitoring in AML and into the dynamics of genetic mutations during AML treatment," wrote Friederike Pastore, M.D., and Ross Levine, M.D., of Memorial Sloan Kettering Cancer Center in New York, in an accompanying editorial. Additional studies are needed, they continued, to validate the findings, test how a genomic approach to monitoring patients with AML compares with flow cytometric approaches, and determine whether the approaches could possibly be used in combination.
The work is promising, but Dr. Ley cautioned that "it's early days for using genomic data to treat people with cancer."
Although the simplest way to think about using sequence data to inform treatment is to identify a mutation and then use a drug that targets that mutation, the heterogeneity of tumors makes cancer treatment a much more complex problem, he explained.
"How to use genomic data to guide how patients are treated in the clinic is far from a settled matter," Dr. Ley said. "Much more work is needed to define the most informative approaches, and the best ways to apply this knowledge to the care of patients. Despite these caveats, however, I have to say we are making steady and encouraging progress."