"Fine Tuning" Engineered T Cells May Extend Immunotherapy Approach to More Cancer Types
, by NCI Staff
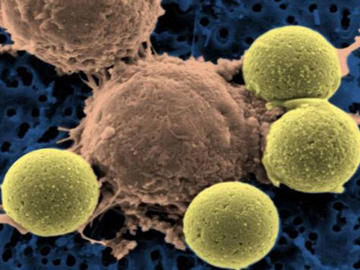
Engineering immune cells to have a decreased ability to bind to their targets on cancer cells doesn’t appear to impair their ability to kill cancer cells, but it may cause them to spare healthy cells that have low levels of the same molecular target.
The findings, which come from two new studies performed in cancer cell lines and mice, suggest a way to make an investigational form of immunotherapy, known as CAR T cell therapy, a potential treatment option for more cancers, say the investigators who led the studies.
Results from both studies were published September 1 in Cancer Research.
Overcoming 'On-Target, Off-Tissue' Toxicity
To date, CAR T cell therapy has been tested primarily in blood cancers, demonstrating remarkable results in some patients, including complete remissions that have lasted for many years in patients with advanced disease.
Producing this therapy is a highly complex process that involves engineering T cells collected from patients’ blood to produce special receptors on their surfaces — called chimeric antigen receptors, or CARs. The CARs are designed to bind to specific molecules, or antigens, that are found at higher than normal levels (overexpressed) on the surface of cancer cells. The engineered T cells are then grown in the laboratory into hundreds of millions of cells and infused back into the patient.
A substantial obstacle to extending the study of CAR T cells to patients with solid tumors has been “on-target, off-tissue toxicity,” where the engineered T cells “don’t discriminate between cancer cells and normal cells,” explained Daniel W. Lee, M.D., of NCI’s Center for Cancer Research, who is leading clinical trials of CAR T cells in children with cancer.
This phenomenon is a result of the difficulty in finding suitable target antigens on cancer cells in solid tumors that aren’t also found on normal cells, which makes them susceptible to attack by the T cells, a direct cause of side effects.
Affinity Tuning to the Rescue?
By decreasing the affinity of the engineered T cells for their target antigens, this new approach may offer a way to overcome this barrier, authors from both studies suggested.
In the first study, a research team led by Yangbing Zhao, M.D., Ph.D., of the University of Pennsylvania, tested CAR T cells engineered to target the HER2 protein (also called ErbB2), which is overexpressed in approximately one-fourth of breast cancers, as well as in several other solid tumors.
Dr. Zhao and his colleagues manufactured a series of CAR T cells that had either a strong attraction (high affinity) or a low attraction (low affinity) to HER2. Studies in cell lines and mice showed that the affinity of the CAR T cells for HER2 affected their ability to distinguish between low- and high-HER2 expressing cells.
For example, in mice bearing HER2 overexpressing tumors on one side of their body and low HER2 expressing tumors on the other side, inoculating them with the high-affinity CAR T cells shrunk tumors on both sides. But when the mice were inoculated with the low-affinity CAR T cells, only the high HER2-expressing tumors regressed, while the low-expressing tumors continued to grow.
The second study, led by Laurence Cooper, M.D., Ph.D., of Ziopharm Oncology Inc., formerly of The University of Texas MD Anderson Cancer Center, and his colleagues, reported similar findings in a different experimental model. The research team constructed CAR T cells that had either high or low affinity for EGFR, a tumor-associated antigen that is overexpressed in more than 60 percent of human glioblastoma tumors, among other cancers, but in low levels on normal cells.
In an animal model of glioblastoma that overexpresses EGFR, both the high- and low-affinity CAR T cells shrank the tumors. But, because of their toxicity, overall, the high-affinity T cells did not substantially improve how long mice lived compared with untreated mice. Survival was improved, however, in mice treated with the low-affinity CAR T cells. In mice with low EGFR expressing tumors (a stand-in for normal cells with low EGFR expression), the high-affinity CAR T cells shrank tumors and appreciably improved how long some mice lived, whereas the low-affinity CAR T cells had little effect on tumors or survival.
Much of the research to improve CAR T cell performance has been focused on enhancing the activation of T cells by modifying the portion of the engineered receptor that is inside the cell, Dr. Cooper explained in a news release.
“Our study has shown that another possibility is to tweak the extracellular portion of the CAR that docks with the tumor by adjusting its affinity for the target protein,” he said.
Still Work To Do
More research is needed to determine whether low-affinity CAR T cells are a viable option for solid tumors, Dr. Lee cautioned.
The mouse models used in these studies, for example, are very limited in their ability to predict side effects from low-affinity CAR T cells, he continued.
“And, theoretically, the price one pays for an affinity-tuned CAR is a lower response rate or the depth of response—a partial response versus complete response,” Dr. Lee said. “We just won’t know this until these CARs enter clinical trials.”
Affinity-tuned CAR T cells are just one option being studied for extending this treatment approach to patients with solid tumors, he added. “The field is actively trying to overcome this limitation.”