Brain Cancer’s Cholesterol Addiction May Offer New Treatment Strategy
, by NCI Staff
To survive and grow, brain cancer cells are heavily dependent on a constant supply of cholesterol provided by other brain cells, a new study suggests.
Moreover, the researchers found that brain cancer cells take in more cholesterol than normal brain cells and subvert normal mechanisms of cholesterol regulation, allowing them to stockpile cholesterol. But this dependency creates a potential vulnerability, the researchers showed. In mice with human brain tumors, treatment with a drug that depletes cholesterol killed tumor cells, slowed tumor growth, and improved survival.
Finding effective treatments for brain cancer is challenging because most drugs are unable to penetrate the blood-brain barrier. However, the cholesterol-targeted drug that the researchers tested was able to accumulate in the brain.
The results of the study, published November 14 in Cancer Cell, may offer a new strategy for treating brain cancer, wrote Paul Mischel, M.D., of the Ludwig Institute for Cancer Research at the University of California San Diego, and his colleagues.
“It’s an exciting and novel angle for targeting this tumor type,” said Matthias Holdhoff, M.D., Ph.D., of the Brain Cancer Program at the John Hopkins Sidney Kimmel Comprehensive Cancer Center, who was not involved in the study.
An Essential Fat
Although high cholesterol is a well-known risk factor for heart disease, it is actually an essential fat molecule that is critical for maintaining the structure and functions of cells and organs. Growing cells especially rely on cholesterol, explained Dr. Mischel.
Healthy cells require a balanced level of cholesterol—too much or too little of it can be toxic. That balance is maintained, in part, by negative feedback signals: When cholesterol levels rise too high, cholesterol synthesis and uptake are shut down.
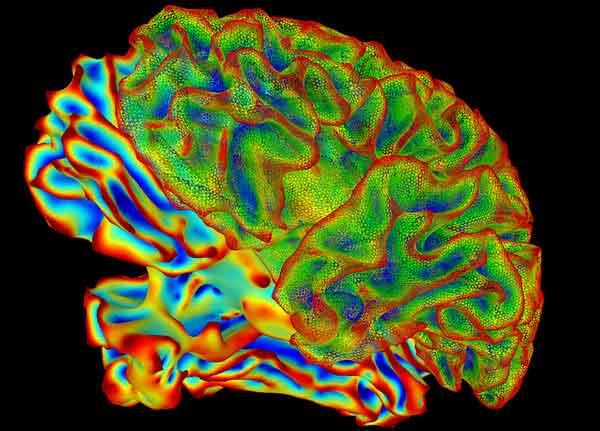
Of all organs in the human body, the brain has the highest level of cholesterol, and nearly all of it is made on site by a specific type of brain cell.
In previous studies, Dr. Mischel and his colleagues showed that brain cancer cells are “stuffed with cholesterol,” he said, and that, compared with normal brain cells, they express more of a protein responsible for cholesterol uptake.
“This really got us thinking about what cholesterol does in brain cancer,” said Dr. Mischel. “We began to think about this concept of targeting co-dependencies”—using drugs to target enzymes or proteins that are not oncogenes, but that cancer cells may also depend on for growth and survival.
“A lot of knowledge has emerged over the last 10 years on oncogenes and mutations that drive brain cancer growth,” said Dr. Holdhoff. “But to date we don’t have ways to effectively target these mutations.”
Based on their earlier findings and the unique environment in the brain, Dr. Mischel and his colleagues hypothesized that the growth and survival of brain cancer cells may depend on cholesterol and that targeting molecules involved in cholesterol regulation could represent a therapeutic opportunity.
Addiction Rehab
The researchers focused on glioblastoma (GBM), a highly aggressive type of brain cancer for which there has been little improvement in clinical outcomes over the last 50 years.
They first compared the expression of key proteins involved in cholesterol synthesis and import in GBM tumor samples and healthy brain tissue samples. They found that GBM tumors express fewer proteins involved in cholesterol synthesis but overexpress proteins involved in cholesterol import. This suggested that GBM cells largely obtain cholesterol from an outside source.
Further lab tests confirmed this finding, showing that a GBM cell line took up 3- to 4-fold more cholesterol than healthy brain cells.
The researchers next examined a negative feedback signal that regulates cholesterol levels. When molecules made from excess cholesterol bind to proteins called liver X receptors (LXRs), cholesterol import is halted and export is revved up—lowering total cholesterol levels.
The researchers discovered that this LXR feedback signal was less active in GBM cells than in healthy brain cells, which, the authors suggest, “gives tumor cells access to an abundant and uninterrupted source of cholesterol.”
Dr. Mischel and his colleagues decided to test whether treating GBM cells with an LXR agonist—a synthetic molecule that binds to LXRs and activates the feedback signal—might reduce their cholesterol levels and inhibit their growth.
When the researchers treated several GBM cell lines with the LXR agonist LXR-623, they found that the cells took up less cholesterol and exported more, lowering net cholesterol. Furthermore, LXR-623 killed several GBM cell lines but not healthy brain cells.
And encouragingly, results from a human clinical trial testing LXR-623 in the context of heart disease suggested that it might be possible for the drug to reach the brain.
When the researchers tested LXR-623 in normal mice, they found that the drug penetrated the blood-brain barrier and accumulated to concentrations that had produced anticancer activity in their earlier lab tests. In addition, treating mice with GBM tumors derived from human patients with LXR-623 killed tumor cells, substantially reduced tumor size, and improved survival.
And, as the research team found in their cell line experiments, the tumors of mice treated with LXR-623 expressed more cholesterol-export protein and less cholesterol-import protein.
Treating mice with LXR-623 did not damage healthy brain cells or affect normal levels of fat in the liver, they found, suggesting that the effect of LXR-623 was relatively selective for cancer cells in the brain.
Given these promising results, said Dr. Mischel, “we are trying to figure out the right strategy to make this drug available to patients. And then, how do we design the right trials, and for which subsets of patients?”
Perfect Fit
In light of their findings, Dr. Mischel reflected, “it’s remarkable how the cancer cells have developed a set of adaptations that are just perfectly fit for the brain environment.”
First, instead of making cholesterol themselves—a process that is “very costly energy-wise,” he explained—glioblastoma cells absorb cholesterol made by other brain cells.
Second, GBM cells bypass the LXR feedback loop and another built-in feedback loop that limits cholesterol synthesis. These adjustments allow them to basically act like “parasites” on the brain’s cholesterol system, he continued.
“But these adaptations do come at a cost, by creating a vulnerability,” Dr. Mischel emphasized. These and similar findings from other studies may represent “the tip of the iceberg for cancer co-dependencies that are shaped by the tumor microenvironment,” he said.
Dr. Mischel and his study coauthor Benjamin Cravatt, Ph.D., of the Scripps Research Institute are developing strategies to identify and target co-dependencies in cancer.
“Thinking into the future, it is unlikely that a single therapy will carry the glioblastoma field forward,” said Dr. Holdhoff. “It’s more likely that combination therapy will eventually lead to better outcomes. So more knowledge on non-oncogenes that are driving tumor growth will be an important piece in the big mosaic of understanding these cancers,” he continued.