Pancreatic Cancer Cells May Obtain Nutrients from Neighboring Cells
, by NCI Staff
Pancreatic cancer cells grow by instructing neighboring cells to provide them with nutrients, a new study published online August 10 in Nature has shown.
The researchers found that when grown together in culture, cancer cells prompted cells from the tumor microenvironment to degrade their own proteins and supply the cancer cells with the resulting amino acids. This external nutrient supply led to increased metabolism and growth in the pancreatic cancer cells. In separate experiments in mice, blocking the supply of nutrients from cells in the tumor microenvironment slowed pancreatic tumor growth.
According to the study's lead investigator, Alec Kimmelman, M.D., Ph.D., of NYU Langone Medical Center, and his colleagues, the study is one of the first detailed reports of what they called “metabolic crosstalk” between pancreatic cancer cells and cells in the tumor microenvironment.
The Pancreatic Tumor Microenvironment
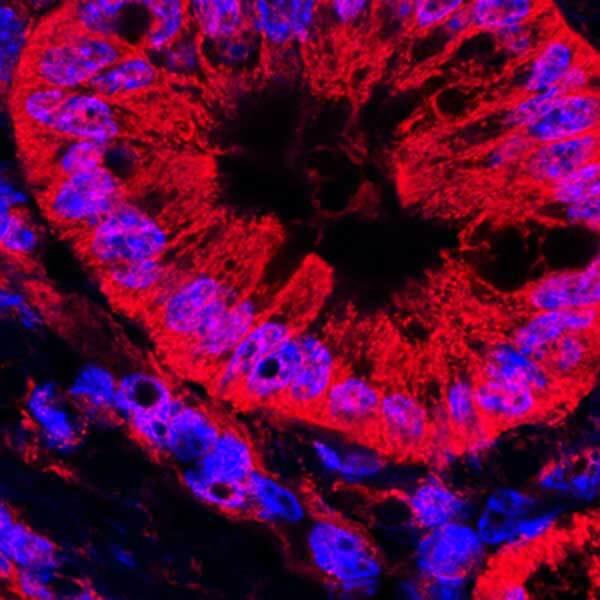
Pancreatic ductal adenocarcinoma (PDAC) is the most common and a very aggressive type of pancreatic cancer, with less than 8% of those diagnosed surviving 5 or more years. A distinct characteristic of PDAC is the presence of a dense web of proteins and noncancerous cells surrounding the cancer cells, collectively called the stroma.
Interactions with stromal cells can be both beneficial and harmful for pancreatic cancer cells. The thick stroma protects pancreatic cancer cells by limiting their exposure to chemotherapy drugs, but it also blocks their access to blood vessels that supply nutrients such as glucose. As a result, pancreatic cancer cells are forced to scavenge for other nutrients to support their metabolism and growth, Dr. Kimmelman explained.
Pancreatic stellate cells (PSCs), star-shaped cells that secrete structural proteins, are abundant in the stroma. Previous studies suggested that PDAC cells encourage PSC growth, and that PSCs, in turn, can promote PDAC growth—prompting Dr. Kimmelman and his colleagues to hypothesize that PDAC cells may obtain extra nutrients from PSCs.
To test their idea, the researchers treated either human PDAC cells or healthy pancreatic cells with culture medium—an aqueous solution that contains molecules secreted by the cultured cells—from a PSC cell line. They found that the treated PDAC cells, but not the healthy pancreatic cells, showed signs of increased metabolism specifically in the mitochondria, the compartment in cells that generates energy.
The researchers then analyzed the PSC culture medium to try to identify what was driving the increased PDAC metabolism. Of the nearly 200 candidate metabolites they analyzed, they found that two amino acids secreted by PSCs, alanine and aspartate, were absorbed by PDAC cells. But, they showed, only alanine stimulated mitochondrial metabolism in PDAC cells.
“Alanine has not typically been studied as a major fuel source for tumor cells; it is mostly viewed as a building block for proteins,” said Dr. Kimmelman. “But in this case, alanine has a critical role in tumor metabolism.”
The researchers believe that using alanine as a main energy source allows “the cancer cells to utilize more traditional fuel sources—such as glucose—for other things, like making building blocks of DNA and RNA,” explained Dr. Kimmelman. This adaptation, he added, allows cancer cells to be more “flexible” in the nutrient-scarce tumor microenvironment.
Alanine from Autophagy
The team then delved further into this “crosstalk” between PDAC cells and PSCs. They hypothesized that PSCs may produce extra alanine through autophagy, an essential function in cells that degrades superfluous, damaged, and toxic molecules into basic units (such as amino acids).
The researchers discovered that when they co-cultured PDAC and PSC cells together, autophagy increased in the PSCs. Furthermore, they found that PSCs required essential autophagy genes to secrete alanine and enhance PDAC metabolism.
The team also observed that PSC culture medium enhanced PDAC cell growth in low-nutrient conditions—similar to the actual tumor microenvironment—and that this effect was dependent on autophagy in PSCs. They found that in mice, tumors from PDAC cells implanted along with PSCs that lacked autophagy-related genes grew slower and were less lethal than tumors from PDAC cells implanted with normal PSCs.
Future Investigations
These findings demonstrate the importance of studying cancer metabolism “in the proper context, in this case, in the presence of relevant supporting cell types,” the researchers wrote. “When we study cancer cells in isolation we may be missing crucial parts of the story, such as the collaborative metabolic crosstalk between stromal and cancer cells,” agreed Michael Espey, Ph.D., of NCI’s Division of Cancer Biology, who was not involved in the study.
And while the role of autophagy in cancer cells has been studied for many years, the tumor-promoting effect of autophagy in noncancerous cells is a unique discovery that warrants further investigation, said Dr. Kimmelman. Several completed and ongoing clinical trials have tested autophagy inhibitors, with mixed results. The new study results, he continued, suggest that autophagy inhibitors could potentially provide a “two-for-one effect” in pancreatic cancer.
The scientists are now working to uncover the molecular signal PDAC cells use to rev up autophagy in PSCs. “There have only been a handful of secreted molecules reported to increase autophagy, so we are trying to figure out what this one is,” said Dr. Kimmelman.