Levels of Immune Cells within Ovarian Tumors Linked to Survival for Some Patients
, by NCI Staff
A large international study suggests that the presence of certain immune cells in the tumors of some patients with ovarian cancer are associated with improved survival.
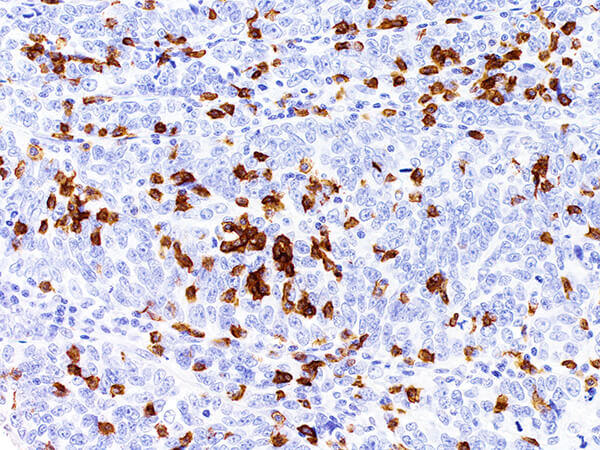
For the analysis, researchers with the Ovarian Tumor Tissue Analysis Consortium counted immune system cells called cytotoxic CD8-positive tumor-infiltrating lymphocytes (TILs) in the tumors of more than 5,500 patients. They then compared the results with information on how long these patients lived.
The strongest link between the number of TILs and overall survival was for patients with high-grade serous ovarian cancer, which is the most common and lethal histological type, or histotype, of the disease. For these patients, as the number of TILs in tumors increased there were corresponding improvements in survival.
Ellen L. Goode, Ph.D., of the Mayo Clinic and her colleagues reported their findings in JAMA Oncology on October 12.
There are five major histotypes of ovarian cancer: endometrioid, clear cell, mucinous, and low-grade serous ovarian cancer, as well as high-grade serous ovarian cancer.
The new study suggests that, at least for some patients with ovarian cancer, the numbers of these cells in tumors—and not merely the presence or absence of these cells—may be associated with overall survival in ovarian cancer, the researchers noted.
“One of the messages of this study is that the more immune cells you have in your tumor, the better,” said study coauthor Martin Koebel, M.D., of the University of Calgary, who was among the dozens of investigators from 70 institutions worldwide who conducted the research.
“This was a validation study, and its main strength was the size of the patient sample,” Dr. Koebel continued. He noted, however, that the association between the number of TILs and survival appears to vary depending on the histotype of ovarian cancer.
Counting Immune Cells in Ovarian Tumors
Previous studies have linked TILs and overall survival in several cancers, including ovarian cancer. But the ovarian cancer studies have been relatively small and could not evaluate patients with the various histotypes of the disease.
To address these issues, the consortium collected and analyzed data from thousands of patients in nine countries, including nearly 3,200 patients with high-grade serous ovarian cancer. The researchers classified the levels of CD8-positive immune cells in ovarian tumors as none, low, moderate, or high.
They then compared the levels with information on patient survival. Looking at all high-grade serous ovarian tumors combined, the median survival was 2.8 years for patients with no CD8-positive TILs and 3 years, 3.8 years, and 5.1 years for patients with low, moderate, or high levels of CD8-positive TILs, respectively.
“What’s remarkable is the size of the effect,” said Dr. Koebel. “The median overall survival for the group with high levels of intratumoral lymphocytes is almost double that of the group with no lymphocytes.”
Results Vary Depending on Histotype of Ovarian Cancer
Overall, the findings suggest that the association of CD8-positive TIL levels with ovarian cancer survival may depend on certain factors, such as which histotype of ovarian cancer a patient has or the molecular signature within a histotype, Dr. Koebel noted.
When the researchers evaluated the association among patients with less common histotypes of the disease, the results were mixed. TIL levels were associated with survival among patients with endometrioid and mucinous tumors, but not among patients with clear cell and low-grade serous ovarian cancers.
Among patients with high-grade serous ovarian cancer, high levels of CD8-positive TILs were associated with favorable outcomes even when the researchers considered known prognostic factors, such as stage of the disease and the extent of cancer remaining after surgery.
For patients with high-grade serous ovarian cancer who inherited harmful mutations in the BRCA2 gene, however, CD8-positive TILs did not appear to be associated with survival, whereas they were for patients with inherited mutations in the BRCA1 gene.
“The impressively large number of patients in this study allowed the investigators to ask detailed questions about whether the numbers of CD8-positive TILs correlate with overall survival in women with ovarian cancer, and how this differs between histologic subtypes of ovarian cancer,” said Christina M. Annunziata, M.D., Ph.D., of NCI’s Center for Cancer Research, who was not involved in the study.
She was not surprised, based on the results of earlier and smaller studies, that clear cell cancers and mucinous cancers were more likely to have no CD8-positive cells at all. But this finding suggests “that the presence of CD8-positive cells may not be a reliable marker for sensitivity to immunotherapy, because many of the ‘responders’ in immune checkpoint inhibitor studies have been women with clear cell cancers,” Dr. Annunziata explained.
“The presence of CD8-positive cells has potential clear prognostic value for women with ovarian cancer,” she added. “Additional studies are needed before we can predict which patients will respond to immune checkpoint inhibitors.”
Investigating the Factors that Influence Infiltration
The study authors wrote that identifying the factors that drive the infiltration of immune cells into ovarian tumors will likely reveal insights into the diversity of patient outcomes in this cancer. This research could also lead to strategies for improving the effectiveness of current and future treatments.
“We know the immune system is important in many cancers,” said Dr. Goode of the Mayo Clinic. “It’s clear that much more research on immune factors in ovarian and other types of cancers is needed to help us harness the immune system for the treatment of patients with cancer.”
Dr. Goode and her colleagues are now trying to understand which factors might affect TIL levels in tumors, including characteristics of the tumor and the affected individual, such as inherited factors, features of the tumor microenvironment, and other immune cells.
The current study, she added, “underscores the need for global research that uses rigorous scientific methods to tease out prognostic factors in ovarian cancer.”