Breast Cancer Surgery Choice May Affect Young Survivors’ Quality of Life
, by Edward Winstead
The type of surgery young women with early-stage breast cancer choose may affect their quality of life years later, according to a new study.
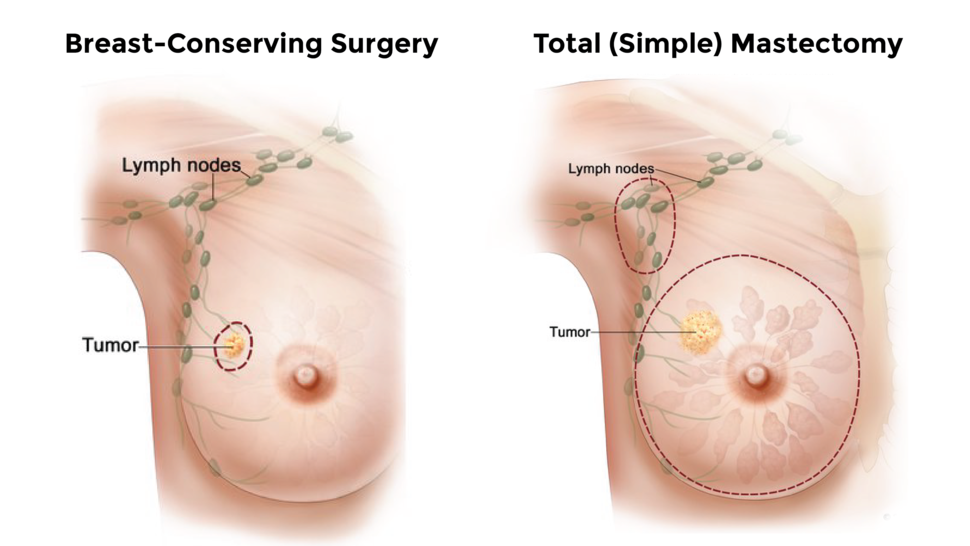
Women who had one or both breasts surgically removed (a unilateral or bilateral mastectomy) had lower scores on a quality-of-life survey, indicating worse quality of life, than women who had surgery to remove just the tumor and some nearby healthy tissue (breast-conserving surgery), researchers found.
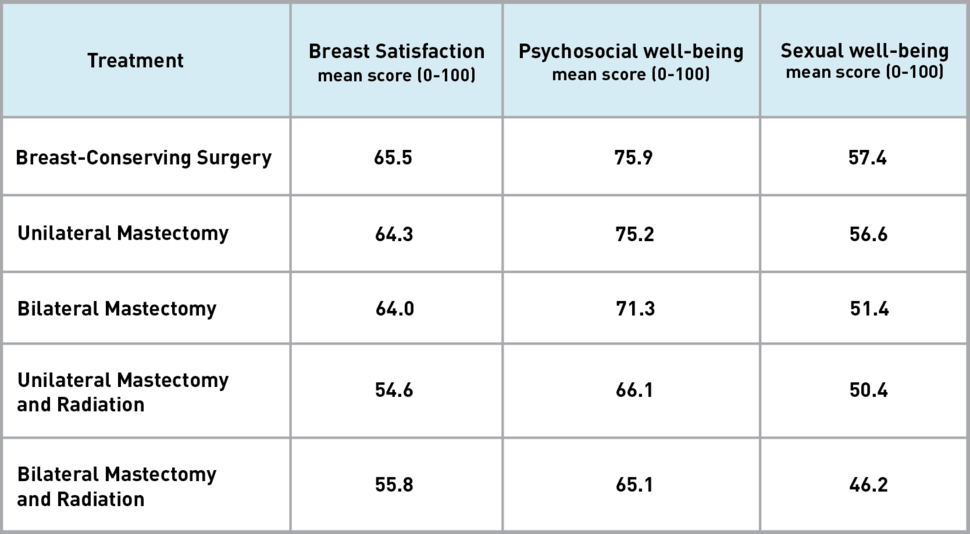
The researchers sent a questionnaire called BREAST-Q to 560 young breast cancer survivors (40 years or younger at the time of diagnosis) to complete as part of their follow-up. The women were asked about several topics, including their satisfaction with their breasts after surgery, psychosocial well-being (e.g., anxiety levels), and sexual well-being.
In each of these areas, the responses differed depending on whether a woman had undergone breast-conserving surgery, unilateral mastectomy, or bilateral mastectomy. Women who underwent a mastectomy followed by radiation therapy reported the lowest scores, indicating worse quality of life, according to results published in JAMA Surgery on September 1.
“Surgical choices that women with breast cancer make can have an impact on their long-term quality of life,” said Laura Dominici, M.D., a surgeon at the Dana-Farber Brigham Cancer Center, who led the study.
“As clinicians, we need to have conversations with our patients about the surgical options so that we can help them understand how the treatment they choose might affect their quality of life,” said Dr. Dominici.
Selecting a Surgical Treatment Strategy
Women diagnosed with early-stage breast cancer often have a choice of surgical treatments. Studies have shown that the different surgical approaches have similar survival rates and comparable risks of the cancer returning. Surgical complications, however, occur more frequently with mastectomy than with breast-conserving surgery.
Despite the similar outcomes, an increasing number of women in the United States with early-stage breast cancer choose mastectomy. This includes women with early-stage cancer in one breast who choose to undergo a contralateral prophylactic mastectomy—surgery that removes the other (healthy) breast.
Indeed, most participants in the study had early-stage breast cancer, and many would have been candidates for breast-conserving surgery, such as a lumpectomy, Dr. Dominici explained. Nonetheless, 72% chose to have a mastectomy (20% chose unilateral mastectomy and 52% chose bilateral) and 28% chose to have breast-conserving surgery.
Study participants filled out the BREAST-Q questionnaire a median of 5.8 years after their cancer diagnosis. Most were White, married, reported being financially comfortable, and had a college education.
The questionnaire asks patients to evaluate a range of issues on a scale from 0 to 100, with higher scores representing a more favorable outcome.
In the area of breast satisfaction, BREAST-Q asks women their thoughts about how well their breasts match, how they feel to the touch, and how they look in and out of clothing. The questionnaire also asks about a woman’s confidence in social settings, emotional health, and self-esteem.
Including the Study Results in Patient Counseling
Results from the new study should be incorporated into patient counseling, wrote Monica Morrow, M.D., a breast surgeon at Memorial Sloan Kettering Cancer Center, in an accompanying editorial.
The lower quality-of-life scores after mastectomy compared with breast-conserving therapy should be included in discussions about the merits of mastectomy versus breast-conserving therapy, Dr. Morrow added.
She pointed out that women with early-stage breast cancer have a low risk of developing cancer in the other (contralateral) breast. This information should be conveyed to patients along with the lack of survival benefit and higher risk of surgical complications with mastectomy, she wrote.
“A surgeon’s recommendation against contralateral prophylactic mastectomy is a powerful deterrent against the use of the procedure,” she wrote.
Trends in Breast Cancer Surgery
Just as mastectomies have become more common, the use of radiation therapy after mastectomy has also been increasing.
Given these trends, the study’s finding of decreased breast satisfaction among women who undergo mastectomy—and particularly among those who receive radiation therapy after breast reconstruction—are “concerning,” the researchers wrote.
“It’s important for us to be able to tell patients that they are potentially going to have a poorer quality of life if they choose a mastectomy, and particularly if they get post-mastectomy radiation,” said Dr. Dominici.
The results of this study emphasize the importance of conducting research on cancer survivors, so that women considering breast surgery can be informed about quality-of-life issues, said Emily Tonorezos, M.D., director of NCI’s Office of Cancer Survivorship.
“If women were considering only the risk of the cancer recurring, these surgical treatment options look similar,” Dr. Tonorezos continued. “But important differences emerge when we consider a patient’s longer-term satisfaction and well-being.”
A limitation of the study was that participants completed the questionnaire only at a single point in time, Dr. Tonorezos noted. Another was that the researchers did not know the participants’ quality of life when they chose their surgery. Nor did the researchers know why participants chose one treatment over another.
The results might not be broadly applicable to women beyond the type of patients in the study (e.g., White, married, college educated), the researchers noted.
“In the past, we might not have spent as much time talking with women about quality of life as we could have,” said Dr. Dominici. “This study demonstrates the importance of having these discussions with our patients.”