For Older Adults, Geriatric Assessment Reduces Cancer Treatment Side Effects
, by Sharon Reynolds
For older adults undergoing treatment for advanced cancer, results from a clinical trial show that a health measurement tool called a geriatric assessment can be an important part of treatment planning. In the trial, older patients whose care was guided by a geriatric assessment were much less likely to experience serious side effects.
In the study, community hospital and clinic staff could use the information and care recommendations provided by the geriatric assessments to help make treatment choices for some patients. They could decrease the intensity of the treatment older adults received, increase the amount of supportive care, or do both.
Compared with people in the study who didn’t receive geriatric assessment–guided care (the usual care group), people who received assessment-guided care (the intervention group) not only experienced fewer side effects, they also were less likely to experience falls in their homes during treatment.
However, no differences in survival were seen between the two treatment groups. Findings from the study were published November 3 in The Lancet.
Older adults with other health problems, such as other diseases or physical disabilities, are rarely included in cancer clinical trials, explained Supriya Mohile, M.D., a geriatric oncologist at the University of Rochester's Wilmot Cancer Institute who led the study, which was funded in part by NCI.
That means that in real-world settings, where older patients often have other health conditions, clinicians don’t necessarily know the optimal doses of commonly used therapies that balance effectively treating their cancer with limiting treatment-related side effects.
“Historically, there's been a concern about undertreatment of older adults, but for those with aging-related conditions and advanced cancer, we’re probably overtreating them,” she said. In this study, “the geriatric assessment changed the decisions clinicians made about treatment and that led to lower toxicity.”
“The fact that there was no difference in [how long patients lived] despite receiving lower dosages of chemotherapy is important,” added Diane St. Germain, R.N., M.S., of NCI’s Division of Cancer Prevention (DCP), who was not involved with the study.
Chronological age vs. physiological age
Age is, in many respects, just a number. “And it would be ageist to say [that] all older adults should be treated the same,” said Dr. Mohile.
But older adults with cancer often have other health problems. These include cognitive challenges, health conditions such as heart disease and diabetes, and a general decrease in what’s known as physiologic reserve. Physiologic reserve "is the ability to recover … from something that's difficult, whether it's cancer and its symptoms or cancer treatment,” Dr. Mohile said.
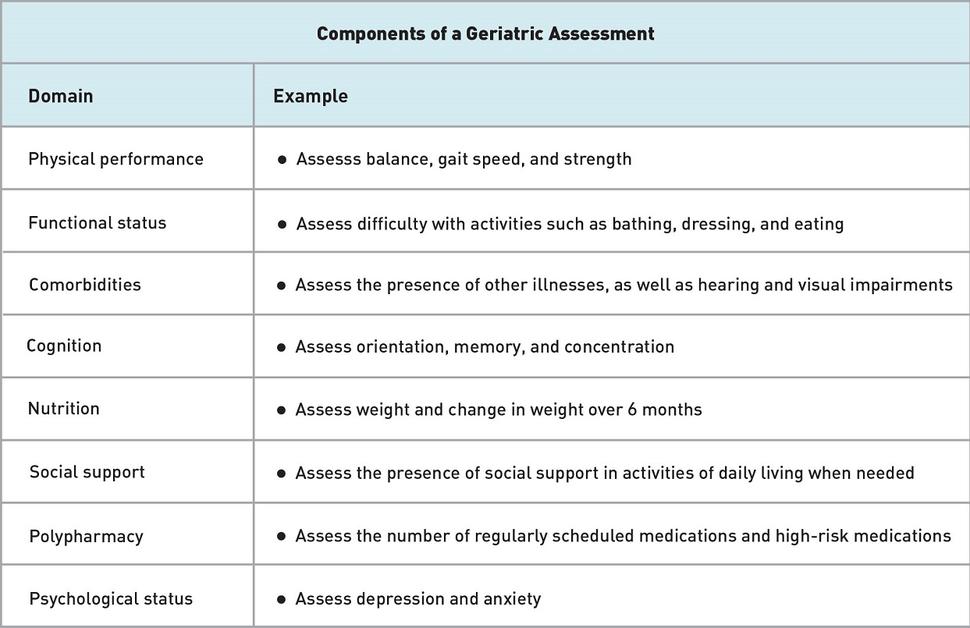
A geriatric assessment collects information about these health problems, or comorbidities, and impairments that otherwise tend not to be captured as part of routine cancer care. (See the table for examples.) These evaluations can potentially identify older adults at highest risk of serious side effects from cancer treatment.
Geriatric assessments help clinicians to determine if a 70-year-old is, for example, physiologically as healthy as the average 45- or 50-year-old or if they’re physiologically closer in health to the average 90-year-old, said Judith Hopkins, M.D., an oncologist with Novant Health in North Carolina who participated in the trial. “And that helps predict [treatment] toxicity,” she said.
Such concerns can be particularly important for people with advanced cancer when treatment is not expected to provide a cure. Instead, therapy in these cases is palliative—that is, it is intended to reduce symptoms of the cancer and improve quality of life.
“You don’t want to take independent older patients and put them in a situation where you [might] substantially improve their cancer but they can no longer live independently or enjoy the parts of life that mean the most to them,” Dr. Hopkins.
Many professional societies recommend doing a geriatric assessment for every adult over the age of 65 who is about to start cancer treatment. But before this trial, it was unclear whether using these assessments in community hospitals and clinics, where most people receive cancer care, could reduce the side effects of treatment.
The clinical trial took place at 40 practice clusters across the country affiliated with the University of Rochester’s hub of the NCI Community Oncology Research Program (NCORP), a national network that brings cancer clinical trials to community-based practices. Practice clusters are groups of community oncology clinics that share one or more doctor, nurse, or other health care team member.
All practice clusters received training on how to perform a geriatric assessment and a temporary staff member who could assist with the assessments. The assessments were given to more than 700 patients aged 70 and older during the study. But what happened after the assessment differed depending on whether health care providers received the results of the assessment.
In the usual care group, summaries of the assessments were not made available to the doctors. In the intervention group, the assessment summaries, along with patient management recommendations, were sent to patients’ oncologists.
In the intervention group, "we gave the oncologists autonomy; they could do whatever they wanted with the assessment," Dr. Mohile explained. "They could throw it in the trash. But they didn't because they thought they were really important. They looked at the summaries, they processed them, and they decided to adjust treatment delivery based on them," she said.
More than 90% of the oncologists in the intervention group implemented at least one management recommendation from the summaries.
Making cancer treatment more tolerable
The treatment adjustments implemented by the oncologists took many forms.
For example, 23% of people in the intervention group compared with 18% of those in the usual care group received a single chemotherapy drug instead of a combination of two or more drugs, which have the potential to cause more side effects. And almost 50% of people in the intervention group, compared with 35% of those in the usual care group, started treatment with lower-than-normal doses, instead of receiving a dose reduction later during treatment if needed.
These adjustments led to a lower rate of serious side effects. Whereas about 70% of people in the usual care group experienced one or more serious side effects—including fatigue, nausea and vomiting, and infection—during treatment, only 50% of people whose doctors used information from the geriatric assessment did. Almost 60% of people in the usual care group required a dose reduction due to treatment side effects compared with just over 40% in the intervention group.
The intervention group also received more supportive care, including referrals to social workers or nutritionists, and, importantly, Dr. Mohile explained, adjustments to medications taken for other health conditions.
The use of several medications at the same time, sometimes called polypharmacy, has the potential to magnify the side effects of cancer treatments, she continued. For example, drugs commonly used to treat conditions like high blood pressure, diabetes, and depression and anxiety can compound dehydration, dizziness, and other side effects from cancer treatment that are risk factors for falls.
“You have to be proactive about stopping or adjusting those [medications]” when possible, she added.
Overall, 21% of people in the usual care group experienced a fall over the 3 months of the study compared with 12% in the intervention group.
Making geriatric assessment accessible
“This is the first nationwide study to show that using a geriatric assessment to make specific changes to how older cancer patients get treated makes a difference [to them]; that it allows them to have fewer serious consequences from therapy,” said Lori Minasian, M.D., also of NCI’s DCP, who was not involved with the study.
“Now that it’s been clearly demonstrated that using the assessment works, are there ways to modify it, make it easier and [more] streamlined for a variety of different scenarios?” Dr. Minasian asked.
Implementing such assessments as they’re done now would likely be challenging for many community practices, said Dr. Hopkins. “Unfortunately, most health care systems don’t have dedicated [staff] in a clinic to do this on a regular basis.”
Some of the NCORP clinics that signed up for the trial could not enroll any patients because of such staffing issues, even with the temporary help provided through the trial, Dr. Hopkins explained. “A new-patient visit might be a 30- or 45-minute slot, or an hour. Adding a geriatric assessment takes, on average, about 20 minutes. That becomes very challenging,” she said.
Dr. Hopkins and other members of an American Society of Clinical Oncology working group are currently creating a simplified geriatric assessment that could be mostly completed by patients and their families at home or in the waiting room.
“Then the remainder could be done by the physician while they’re doing the patient history and physical exam,” she explained.
“I’m very hopeful that, in the next year, we’ll have a template that can be distributed to physicians that … can improve patient care without interfering with [clinic workflow],” said Dr. Hopkins. The team is also planning on creating a training video to teach community oncologists how to perform and interpret the assessment and how to use it to guide patient care.
For now, Dr. Hopkins added, older adults with cancer who want to get a geriatric assessment before treatment may be able to have one done by a geriatrician, if such a specialist is available in their community. “These things can be scheduled separately from an [oncology] office visit," she said.
There are also resources available for doctors who want to implement geriatric assessments at their hospital or clinic now, Dr. Mohile said. For example, the Cancer and Aging Research Group, an association of geriatric oncology researchers, will connect interested oncologists with others around the country who have already implemented geriatric assessments in their practice for advice and mentorship, she explained.
More work is needed to understand which groups of older adults would benefit most from geriatric assessment, explained St. Germain. Research is also needed to determine which components of such an assessment are most useful in different types of cancer because it may not be feasible or necessary to conduct a comprehensive geriatric assessment in all older adults with cancer, she said. For example, the most useful components may be different for patients with early-stage breast cancer compared with those with acute leukemia.
“But it’s now been clearly demonstrated that geriatric assessment works,” said Dr. Minasian. “The next step is to streamline it and refine it for specific populations in a way that benefits [both] patients and practices.”