Patient with Brain Tumor Responds Dramatically to Targeted Therapy
, by NCI Staff
Researchers reported last year that most cases of a brain tumor known as papillary craniopharyngioma harbor a change in the BRAF gene called the V600E mutation. In a new case study, the researchers now say that a patient with this disease had a dramatic response to a targeted drug that inhibits the mutant BRAF protein.
The drug, dabrafenib (Tafinlar®), has been approved by the Food and Drug Administration to treat BRAF-mutant advanced melanoma. The case study describing the patient’s experience appeared in the Journal of the National Cancer Institute on October 23.
Treatment with dabrafinib shrank the patient’s BRAF V600E mutation-positive craniopharyngioma, which had recurred despite four surgical attempts to remove the tumor. The patient also received the drug trametinib (Mekinist®), which inhibits a protein known as MEK and has been shown to enhance the effects of inhibiting BRAF.
"This is the first time that a systemic therapy has shown efficacy against this type of tumor," said study coauthor Priscilla Brastianos, M.D., of the MGH Cancer Center in a news release. "This has the potential of completely changing the management of papillary craniopharyngiomas."
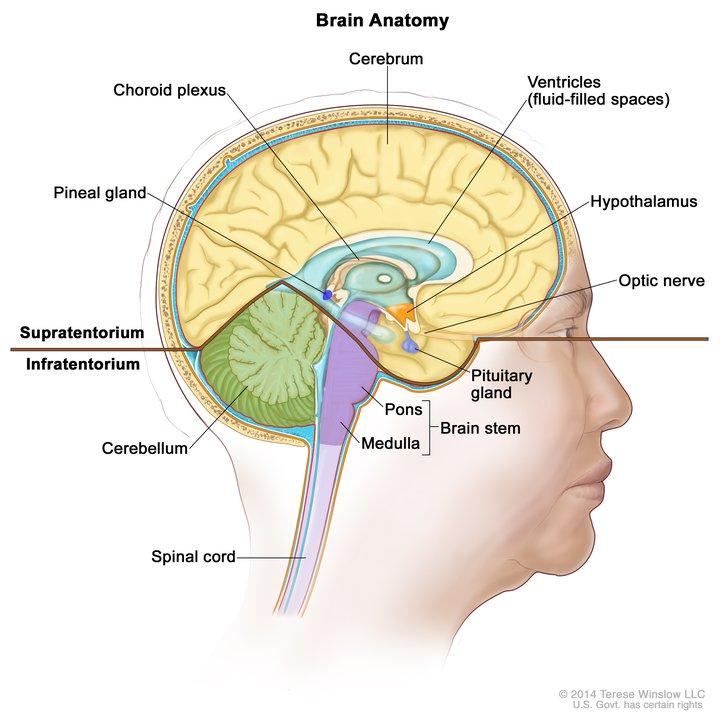
Although they are benign brain tumors, craniopharyngiomas may be considered malignant because the tumors can damage parts of the brain as they grow and cause serious neurological problems. Efforts to treat the tumors with surgery or radiation therapy may damage nearby regions of the brain, and removing these tumors completely is a challenge because the tumor cells may adhere to nearby structures. As a result, the tumors may grow back.
The patient described in the study initially had surgery to remove a tumor enclosed in a fluid-filled sac that was pressing against midbrain structures and preventing cerebrospinal fluid from draining. His symptoms—which included confusion, visual deficits, severe headaches, and vomiting—improved after surgeons removed part of the tumor, but the tumor regrew. Six weeks later, the patient returned to MGH in nearly comatose condition.
When the regrown tumor was removed, doctors confirmed that the tumor was a craniopharyngioma with a BRAF V600E mutation. Just 2 weeks later, before the doctors could start planned radiation therapy, the patient’s tumor had regrown, resulting in another emergency surgery. Seven weeks later, the patient was readmitted to the hospital with progressive vision loss; again, the tumor had expanded.
At this point, the doctors initiated treatment with dabrafinib. After 4 days of treatment, the patient’s tumor was 23 percent smaller; by day 17 the tumor was less than half the size it had been before treatment, and the cyst surrounding the tumor was 70 percent smaller.
On day 21 of treatment, the doctors added trametinib. By day 35, both the tumor and the cyst had lost more than 80 percent of their pretreatment size. Three days later, doctors used endoscopic surgery to remove accessible tumor tissue.
A week later, the patient stopped taking the drugs and soon after began radiation treatment. At the time of publication, the patient remained free of symptoms more than a year since his last treatment.
Another finding of the study was the detection of the BRAF V600E mutation in blood samples taken at different times over the course of treatment. This discovery raises the "hope of potentially diagnosing this mutation and perhaps shrinking these tumors with targeted therapy before surgery, which could make surgical removal safer and possibly unnecessary for some patients," said coauthor William Curry, Jr., M.D., of MGH Neurosurgery in the news release.
Another group of researchers reported last June that a patient with recurrent papillary craniopharyngioma had a “pronounced” response to another BRAF inhibitor, vemurafenib (Zelboraf®). The findings support "the evidence that the BRAF V600E mutation is pathological in this condition," the researchers concluded.