Lung Cancer Precision Medicine Trials: Adapting to Progress
, by Shakun Malik, M.D.
As recently as a decade ago, a patient diagnosed with advanced lung cancer had a straightforward choice of treatments: chemotherapy or palliative measures. Many oncologists advised their patients against chemotherapy, feeling that the choice offered little if any potential benefit.
Fast forward to the waning days of 2015 and, for a growing number of patients with lung cancer, things have changed dramatically. Over the past 3 years, the Food and Drug Administration (FDA) has approved nine new therapies for patients with lung cancer. Although not beneficial in every patient, these new treatments—both targeted therapies and immunotherapies—can produce substantial tumor responses and, importantly, improved survival in some patients.
In 2015 alone, the FDA has approved five drugs for certain patients with metastatic lung cancer. These include two new immunotherapy drugs—the checkpoint inhibitors pembrolizumab (Keytruda) and nivolumab (Opdivo)—for patients whose tumors are no longer responding to other treatments (including targeted therapies), and three targeted therapies—gefitinib (Iressa), osimertinib (Tagrisso), and necitumumab (Portrazza).
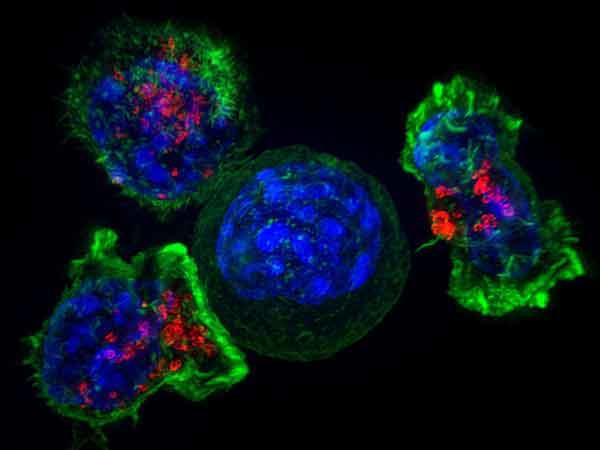
The approvals illustrate how patients with lung cancer are benefiting from the boom in our understanding of the molecular drivers of patients’ tumors and the interplay of the immune system with a tumor and its surrounding environment.
The approvals also capture the rapid pace at which lung cancer therapies are evolving. At NCI, we’re working to stay ahead of that curve, with much of that work falling under the umbrella of precision medicine.
In the Vanguard: Precision Medicine Trials
NCI is, of course, no stranger to precision medicine. We have been at the forefront of efforts to transition the treatment of cancer from a one-size-fits-all approach to one in which treatments are based on the molecular characteristics of each patient’s disease.
A major component of our efforts has been the launch of a series of innovative clinical trials. And given that lung cancer is the leading cause of cancer death, it should be no surprise that two of these trials—ALCHEMIST and Lung-MAP—have their sights set on this disease.
The trials are enrolling two very different patient populations: ALCHEMIST is enrolling patients with early-stage lung cancer, whereas Lung-MAP is enrolling patients with advanced disease. But both trials have a key feature in common: assigning patients to a treatment on the basis of their tumors’ molecular makeup.
Both of these precision medicine trials also share something else in common: they will be undergoing important changes that reflect the emerging role of immunotherapy as an effective treatment for lung cancer.
Amending Trials in Response to Changing Treatments
ALCHEMIST, which was launched last year, is an adjuvant treatment trial; participants have had their early-stage lung tumors completely removed by surgery, and the treatment being studied is administered afterward.
The trial was launched with two treatment groups, or arms (as well as a "screening" arm), and is "matching" participants to their adjuvant treatment—either crizotinib (Xalkori) versus a placebo or erlotinib (Tarceva) versus a placebo—based on whether their tumors have specific alterations in the ALK or EGFR genes, respectively. Patients in the trial whose tumors lack these mutations have received ongoing monitoring.
But with checkpoint inhibitors demonstrating impressive results in patients with advanced lung cancer, we are now taking the next logical step: investigating their role in patients with earlier-stage disease. As a result, a new treatment arm is being added to ALCHEMIST, in which some of the patients whose tumors lack ALK or EGFR mutations will receive nivolumab or no treatment (the control arm).
Lung-MAP is a "master protocol" trial that is assigning patients with advanced squamous cell lung cancer whose cancer has returned after at least one prior therapy to one of a series of sub-studies, or treatment arms.
As is the case for ALCHEMIST, treatment assignment is based on the presence in patients’ tumors of specific genetic alterations. Lung-MAP is testing for specific alterations in multiple cancer-related genes, and patients in each of the trial’s treatment arms are being assigned to the therapy that targets the molecular alteration.
Up to this point in Lung-MAP, patients whose tumors lacked one of the pre-specified alterations were assigned to a study arm testing an investigational immunotherapy agent. However, this trial arm is now being closed and a new arm is being opened in its place. In this new arm, patients whose tumors lack any of the pre-specified alterations will be assigned to either nivolumab alone (the control group) or nivolumab and another immunotherapy drug, ipilimumab (Yervoy).
NCI is currently working with our partners to finalize the details of activating these new immunotherapy arms in ALCHEMIST and Lung-MAP. Updates on these changes will be posted on NCI’s website and promoted on NCI’s social media channels.
These are exciting changes and reflect another important aspect of this new era of clinical trials: the ability to adapt in response to emerging changes in clinical care.
A Bright Future
Clearly we still have a long way to go before we can truly diminish the burden of lung cancer.
Of course, there has been tremendous progress on the prevention and early detection fronts, due in large part to the sharp dip in smoking rates over the past several decades and improvements in screening.
But after many years of feeling stymied and discouraged by the lack of effective new therapies for patients with lung cancer, there is now a palpable sense of enthusiasm among researchers and clinicians that we are turning the corner.
Our hope is that these two precision medicine trials, and others that will surely follow them, will play a key role not just in sustaining this progress but in accelerating it.