FDA Approves Irinotecan Liposome to Treat Pancreatic Cancer
, by NCI Staff
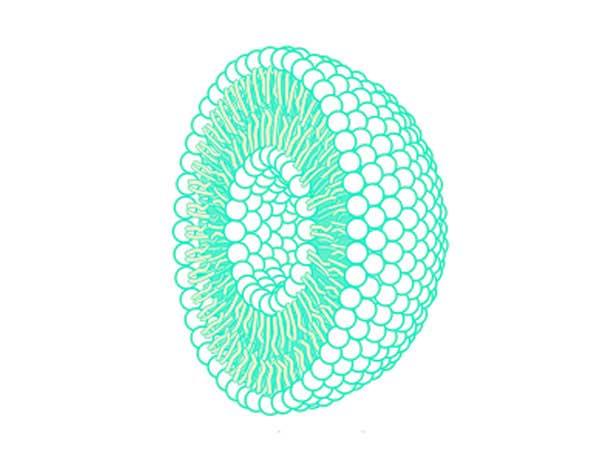
On October 22, the U.S. Food and Drug Administration (FDA) approved irinotecan liposome (Onivyde®) to be used in combination with fluorouracil and leucovorin to treat patients with metastatic pancreatic cancer whose disease has progressed after gemcitabine-based chemotherapy.
The approval was based on results from a clinical trial of 417 patients with metastatic pancreatic cancer. Patients in the trial were randomly assigned to receive treatment with irinotecan liposome alone, irinotecan liposome in combination with the chemotherapy drugs fluorouracil and leucovorin, or with fluorouracil and leucovorin alone.
Patients treated with all three drugs had a median survival of 6.1 months, compared with 4.2 months for those treated with fluorouracil and leucovorin alone. There was no survival benefit with irinotecan liposome alone compared with fluorouracil and leucovorin alone. Patients treated with all three drugs had a 3.1-month delay in tumor growth compared with 1.5 months for those receiving only fluorouracil and leucovorin.
Gemcitabine has been the cornerstone of pancreatic cancer treatment for the past 20 years. A common research approach during much of that time has been to combine gemcitabine with another drug in an attempt to increase its efficacy in previously untreated patients with good performance status, explained Austin G. Duffy, M.D., of the Thoracic and Gastrointestinal Oncology Branch in NCI’s Center for Cancer Research.
“But beyond that there has unfortunately been little progress made in terms of subsequent treatment options for patients who have already received a combination of drugs in the first-line setting and whose cancer has advanced,” Dr. Duffy noted.
“There are relatively few phase III clinical trials performed in this patient population, the so-called second-line setting,” he added. “So any randomized phase III clinical trial, such as this one, that demonstrates a survival benefit in pancreatic cancer is important, both for the obvious reason that it can help individual patients, but also because of the numerous disappointingly negative phase III studies in this disease for drugs that had looked promising in phase II trials.”
Despite these results, Dr. Duffy cautioned that it will still be important to see how well patients tolerate this new therapy and its impact on their quality of life.
Positive trial results and the availability of new options for patients with pancreatic cancer are always good news, he said.
“However, nobody will or should be satisfied with these modest gains,” he continued. “We need to do better at every stage.”