Using Gene Expression to Diagnose Lung Cancer More Accurately
, by NCI Staff
Assessing gene expression in normal cells from the upper airways of current and former smokers with suspected lung cancer may be useful in improving the diagnostic accuracy of bronchoscopy, potentially reducing the need for invasive biopsies, according to a new study published in the New England Journal of Medicine (NEJM).
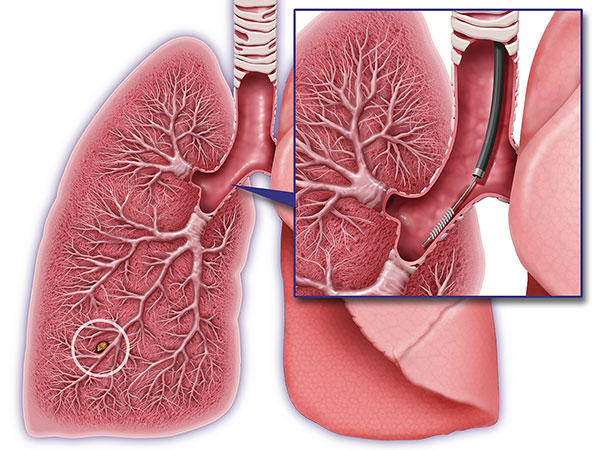
When potentially cancerous lesions in the lung are identified by CT scan, clinicians often use bronchoscopy to evaluate these lesions more closely. Although this procedure is relatively safe, it often fails to produce a definitive diagnosis because the scope cannot reach some areas of the lung. In such cases, an invasive biopsy (surgical or needle) may be required. But these procedures carry the risk of complications, and some investigators have reported more than one quarter of people who undergo a lung biopsy turn out to have benign lesions.
In an effort to help address this problem, the researchers tested the normal bronchial cells in the upper airway, taking advantage of the “field of injury” concept, explained the study’s lead investigator, Avrum Spira, M.D., of the Boston University School of Medicine. When a person smokes, all the cells in their respiratory airways are exposed to tobacco smoke, which causes DNA damage. A distinct pattern of DNA damage can be observed in the epithelial cells of smokers who go on to develop lung cancer, Dr. Spira and his colleagues showed in a 2007 study.
The patterns of DNA damage in normal cells from the upper respiratory tract are “like the canary in the coal mine,” he explained in an interview.
Based on differences in the pattern of DNA damage, the researchers developed a gene expression signature—a genomic classifier—that could be used to test normal cells from the bronchial airway obtained during bronchoscopy for the presence of tumors inside the lungs. In the NEJM study, they applied the findings of the earlier study and showed that “the classifier works in a real-world, clinical setting,” said Dr. Spira.
The study, which was funded in part by NCI’s Early Detection Research Network, enrolled 639 adult current and former smokers who were participating in two clinical trials, AEGIS 1 and AEGIS 2. All participants underwent a bronchoscopy for suspected lung cancer, and a brush was used to collect epithelial cells from the mainstem bronchus of the airway during bronchoscopy. The gene expression patterns in the epithelial cells were analyzed and patients were followed until a diagnosis was made or for 12 months after bronchoscopy. A total of 487 patients were found to have lung cancer.
No diagnosis could be made in 272 patients based on a bronchoscopy alone, they found. Of these patients with a nondiagnostic bronchoscopy, 170 underwent a further invasive procedure to secure a diagnosis (including surgery in 76 patients), 52 of whom were eventually diagnosed with benign lung lesions.
They also assessed the sensitivity and specificity of bronchoscopy plus the classifier, because an accurate diagnostic test not only detects most of the cancers that are present (sensitivity) but it also has a low chance of incorrectly indicating cancer in someone who does not have it (specificity).
Overall, the sensitivity of bronchoscopy plus the classifier was 97 percent compared with 75 percent for bronchoscopy alone. The sensitivity of the combination test was consistently high across nodule size, location, cancer stage, or type, they reported.
The genomic classifier incorrectly suggested cancer in 53 percent of people who did not have lung cancer. Although the test has a high rate of false positives, when both the bronchoscopy and the classifier were negative, the probability that the patient had cancer was reduced.
A negative test result can inform clinical management and eliminate unnecessary invasive biopsies that carry the risk of complications as well as costs to the health care system, Dr. Spira said. “A negative test gives you peace of mind,” he explained.
One limitation of the study is that it was evaluated only in patients who were already strongly suspected of having cancer, said Barry Kramer, M.D., M.P.H., director of NCI’s Division of Cancer Prevention. "The paper doesn’t tell us how this would perform in a true screening setting," Dr. Kramer continued. "The prevalence of cancer in the two cohorts is 74 percent and 75 percent, much higher than in a general population of screened cigarette smokers or former smokers, even with abnormalities on low-dose chest CT."
This is the first time a genomic classifier for lung cancer has been developed and validated in high-risk cohorts, explained Sudhir Srivastava, Ph.D., M.P.H., chief of the cancer biomarkers research group in NCI’s Division of Cancer Prevention. The study, he continued, "lends further support for developing a similar approach for lung cancer screening in an asymptomatic population."
Initially, the test—known commercially as the Percepta Bronchial Genomic Classifier—will be available to 30 to 40 medical centers as part of an early access program before becoming more widely available, according to Veracyte, which manufactures the test.