FDA Expands Approval of Fulvestrant for Advanced Breast Cancer
, by NCI Staff
On August 28, the Food and Drug Administration (FDA) expanded its approval of the estrogen-blocking drug fulvestrant (Faslodex®) for some women with advanced breast cancer.
The new indication for the drug is as a standalone treatment, or monotherapy, for postmenopausal women with advanced hormone receptor (HR)-positive, HER2-negative breast cancer who have not undergone endocrine therapy previously.
Fulvestrant has already been approved for two other uses in women with breast cancer: as a standalone treatment for postmenopausal women with HR-positive metastatic breast cancer whose disease progressed after treatment with other antiestrogen therapy, and in combination with the CDK4/6 inhibitor palbociclib (Ibrance®) for the treatment of women with advanced or metastatic HR-positive, HER2-negative breast cancer that has progressed after endocrine therapy.
“Fulvestrant is emerging as the most effective single-agent therapy in this setting, previously shown in patients who had been treated with aromatase inhibitors and now in patients not previously treated with endocrine therapy,” said Massimo Cristofanilli, M.D., of Northwestern University’s Robert H. Lurie Comprehensive Cancer Center.
Approval Based on Improved Progression-Free Survival
The expanded approval was based on results of a phase 3 trial of 462 postmenopausal women with HR-positive advanced or metastatic breast cancer who had not received endocrine therapy previously. The women in the trial were randomly assigned to receive either fulvestrant or the aromatase inhibitor anastrozole (Arimidex®).
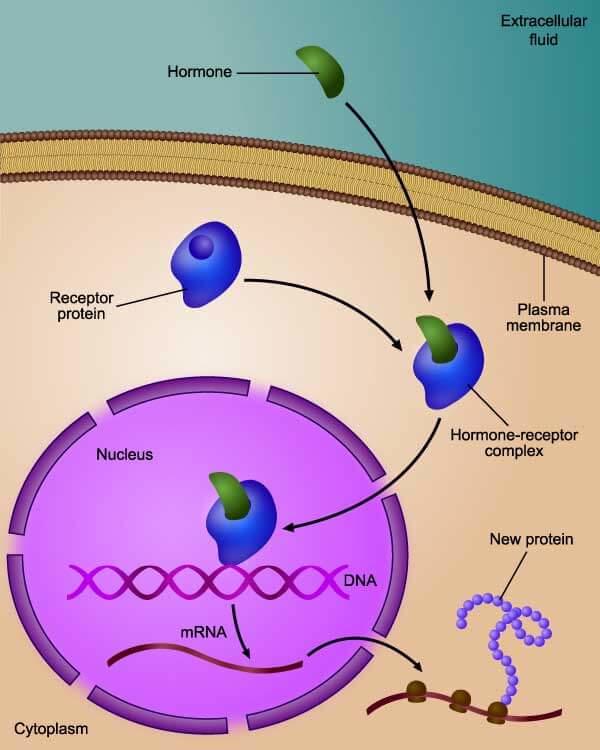
Aromatase inhibitors work by reducing the estrogen available to tumor cells. Fulvestrant works by blocking estrogen from binding to cancer cells.
The primary endpoint of the trial was median progression-free survival. Patients in the fulvestrant group had a median progression-free survival of 16.6 months, versus 13.8 months in the anastrozole group.
Dr. Cristofanilli noted that one group of patients appeared to benefit more than others: Patients whose cancer had not spread to the soft internal organs of the body (that is, those with nonvisceral disease) had a markedly improved progression-free survival rate: 22.3 months with fulvestrant, compared with 13.8 months with anastrozole. By contrast, those whose cancer had spread to visceral organs had a much smaller improvement in progression-free survival: 15.9 versus 13.8 months.
This finding could potentially help doctors plan treatment for patients whose disease shows evidence of spreading at first presentation, Dr. Cristofanilli said.
The most common adverse reactions for women treated with fulvestrant were joint pain, fatigue, hot flashes, and nausea.
Choosing between Fulvestrant and CDK4/6 Inhibitors
Dr. Cristofanilli explained that the treatment of advanced HR-positive breast cancer is becoming more complex as investigators learn more about mechanisms of resistance to endocrine therapy, and as newly approved drugs demonstrate the ability to improve outcomes for women with these cancers.
In this setting, he added, fulvestrant is emerging as an effective single-agent therapy. “In my opinion, this approval provides an excellent, safe, and efficacious option for these patients based on solid prospective clinical data,” he said.
For women with recurrent HR-positive breast cancer, combination treatments that incorporate targeted therapies called CDK4/6 inhibitors with endocrine therapy have emerged as the standard of care, Dr. Cristofanilli continued.
However, “fulvestrant seems to offer an alternative option in women with newly diagnosed HR-positive breast cancer that has never been exposed to endocrine therapy,” he said. “This is probably a group of true endocrine-sensitive patients who may not require or benefit from more aggressive treatments [like combination therapy with CDK4/6 inhibitors].”