Glioblastoma—Unraveling the Threads: A Q&A with Drs. Mark Gilbert and Terri Armstrong of the NIH Neuro-Oncology Branch
, by NCI Staff
Mark Gilbert, M.D., is a senior investigator and chief of the NIH Neuro-Oncology Branch (NOB) within NCI’s Center for Cancer Research (CCR). Terri Armstrong, Ph.D., is a senior investigator in the NOB Patient Outcomes Program. The NOB is a joint program of NCI and the National Institute of Neurological Disorders and Stroke.
With the recent news of Senator John McCain’s glioblastoma diagnosis, we asked Drs. Gilbert and Armstrong to discuss glioblastoma and the research NCI scientists and others are conducting to better understand and treat this cancer.
What is glioblastoma?
Dr. Gilbert: Glioblastoma is a type of astrocytoma, a brain tumor named for the star-shaped cells called astrocytes from which it forms. It is the most common form of brain cancer in adults, accounting for 35-40% of malignant brain tumors.
Approximately 14,000 cases of glioblastoma are diagnosed each year in the United States. They are primary tumors, meaning they originate in the brain rather than spreading to the brain from cancer elsewhere in the body. This type of brain cancer is typically aggressive but rarely spreads outside of the brain.
The disease tends to occur in active, otherwise healthy people, and more frequently in males. Symptoms include headache, memory problems, weakness on one side of the body, difficulty thinking and speaking, drowsiness, nausea, vomiting, and seizures. The onset of symptoms can be sudden and acute; however, in some patients, there may be gradual changes, such as problems with language, concentration, or coordination and strength on one side of the body.
What is the prognosis for people diagnosed with glioblastoma?
Dr. Gilbert: Although glioblastoma does not spread to other parts of the body, it is a very aggressive, grade IV cancer that grows and spreads quickly within the brain and, thus, has a poor prognosis.
We haven’t yet been able to find a cure, but we have seen incremental improvements in survival. The median length of survival was only 8–10 months in the mid-1990s, but it has almost doubled to 15–18 months now. In addition, in the mid-1990s, essentially no patients with glioblastoma survived 5 years after their diagnosis; now 15% of patients survive 5 years.
What are the risk factors for glioblastoma?
Dr. Gilbert: We don’t know what causes glioblastoma and are aware of very few risk factors so far. What we do know is that past radiation to the central nervous system or head increases the lifetime risk of getting glioblastoma. On the other hand, seasonal allergies, such as hay fever, may have a protective effect. The current speculation is that the protection is related to a heightened immune system.
What treatments are currently available for glioblastoma?
Dr. Gilbert: Surgery within a few days of imaging or of presenting symptoms to remove as much of the tumor as possible is the first treatment for the majority of glioblastoma patients. After surgery, patients generally receive a 30-dose course of radiation over a 6-week period and daily treatment with the chemotherapy drug temozolomide (Temodar®) to treat malignant cells that couldn’t be removed with surgery.
Unfortunately, even if the surgeon is able to remove all visible signs of the tumor, these treatments only slow tumor growth and rarely cure the cancer because of microscopic tumor that remains after surgery.
Dr. Armstrong: The standard of care for glioblastoma patients aged 70 and above has been less standardized than that for younger patients. Given the concern over the potential for serious side effects from chemotherapy, a short course of radiation after surgery was often the only treatment administered.
Last year, however, a pivotal Canadian study of glioblastoma in older patients (aged 65 and older) gave new hope to a population of patients who doctors felt were difficult to treat. The study found that older patients given a combination of radiation and temozolomide not only tolerated treatment well but also had improved overall survival. The combination therapy has now been recognized as a potential treatment for older patients with glioblastoma.
Why is glioblastoma so difficult to treat?
Dr. Gilbert: Brain cancers, in general, present many challenges when it comes to treatment. The blood–brain barrier is the most significant factor working against us, because it leads to a drug delivery challenge. This barrier is generally a good feature of the body’s design, a “security system” that protects the brain from threats like viruses or toxins that may be circulating in the bloodstream.
The downside is that it can also impede the delivery of cancer treatments to tumors in the brain and result in a limited portfolio of treatments available to use against brain cancer. Only drugs that are very small and/or fat-soluble, as well as drugs that can be attached to proteins located in the walls of the brain’s blood vessels and transported can cross the barrier and reach the brain. Research is ongoing to discover new ways to penetrate this barrier and reach specific targets in the brain.
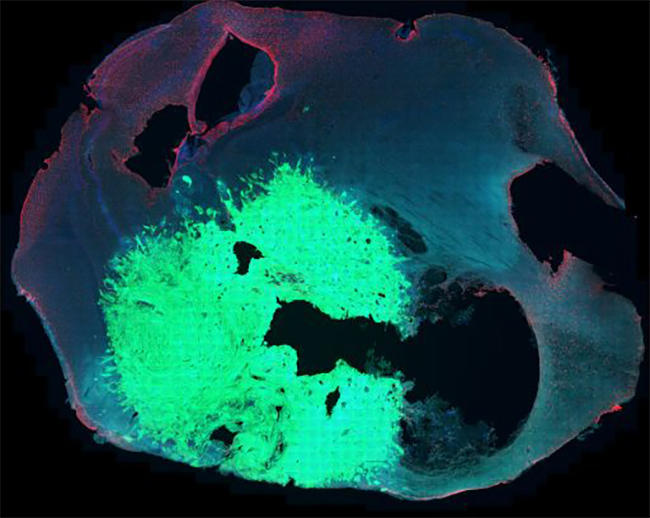
Another treatment challenge we face is the heterogeneity of glioblastoma tumors at the microscopic and genetic levels. Although we may be able to target and kill visible tumor cells, a population of other types of cells in the tumor are resistant to the treatment and continue to proliferate. This results in treatments generally not having long-term success.
Dr. Armstrong: Glioblastoma is a fast-growing brain cancer. As it progresses, it develops infiltrative tumor that extends from the primary site, resembling threads of a spider’s web.
Depending on where the tumor is located, it can’t always be removed entirely by surgery. With brain surgery, we don’t have the luxury of being able to cut out extra tissue as we do with some other solid tumors, because of the detrimental impact it would have on neurological and cognitive functioning for the patient. A maximal safe resection to remove as much tumor as possible without causing harm to the person or significant symptoms is often the goal. Consequently, surgery rarely cures glioblastoma.
Dr. Gilbert: The skull being a fixed shell presents another challenge in treating glioblastoma. Cancer therapies may cause tissues to swell. When we treat liver cancer, for example, the liver can swell in the abdominal cavity. In the case of the brain, however, there is no place to expand because the skull is a hard shell. We have to be very careful about using treatments that could cause swelling of the brain, and that limits the treatments at our disposal.
Cutting-edge immune-based treatments, which have shown promise in several types of cancer, are still undergoing evaluation for glioblastoma. The brain is what we call partially immune privileged, because it doesn’t have as robust an immune system as the rest of the body. The immune response to brain tumors is generally weak, and the cancer tends to circumvent the already limited immune response by making proteins to block the immune system or stimulating cells to suppress the immune system.
Nevertheless, some studies have shown that immune cells from other parts of the body can be summoned to fight off the brain cancer, although that process is not yet well understood. We do think immunotherapy of glioblastoma will eventually be possible, but it’s not going to be an off-the-shelf, already existing treatment.
Developing the right kind of immunotherapy treatment will require a better understanding of the mechanisms of the brain’s immune system and extensive research into optimizing proven immune-based treatments.
What new treatments are being investigated for glioblastoma?
Dr. Gilbert: The two main types of treatments for glioblastoma that researchers are studying in clinical trials are immunotherapy and agents that target specific signaling pathways that we think control the growth of the cancer cells.
Among the immunotherapies being studied are dendritic cell vaccines. These treatments are derived from a patients’ own immature immune cells, which are collected and coaxed to grow into dendritic cells—cells that muster up the immune responses in our bodies.
These cells are then engineered to target specific antigens—that is, proteins produced by glioblastoma tumor cells and not by normal astrocytes. After the dendritic cells are administered to the patient, they produce a tumor-specific immune response in the body, similar to what happens when we receive a flu vaccine. Studies testing these vaccines have so far involved only small numbers of patients, but some studies have suggested that the vaccines may be able to improve how long patients with advanced glioblastoma live, although these results are preliminary and further testing is needed.
CAR T-cell therapy is another type of immunotherapy that is being tested as a possible treatment for glioblastoma. CAR T-cell therapy also involves removing and engineering a patient’s immune cells—in this case T cells—to bind to specific proteins that are overexpressed by glioblastoma cells, and then readministering the T cells to the patient. It’s an approach that has proven successful in some patients for treating melanoma and leukemia.
Another immune-based approach uses checkpoint inhibitors, drugs that have been developed to prevent the tumor from dampening the immune response. A number of checkpoint inhibitors are being tested in clinical trials in patients with glioblastoma.
Some trials in glioblastoma are also testing checkpoint inhibitors in combination with other therapies. For example, we are conducting a clinical trial at NCI that is testing the use of the checkpoint inhibitor pembrolizumab (Keytruda®) along with radiation therapy, temozolomide, and a personalized treatment vaccine made from a patient’s own tumor cells. The hope is that the body will mount an immune response to the cancer after being injected with the vaccine. The simultaneous administration of pembrolizumab should, in theory, prevent the cancer from blunting the immune response.
New technologies are also being developed to improve the molecular characterization of brain cancer cells, as well as to monitor their growth, both of which may help us better diagnose the cancer and target treatments. On the horizon are new imaging technologies that may allow us to identify and visualize biomarkers linked to tumor growth and metabolism. This type of tool would be tremendously beneficial because it would allow us to evaluate quickly whether a treatment is working.
What are some of the other high-priority areas where more progress is needed?
Dr. Armstrong: Of course, the research focus has been primarily on better targeting the cancer. But in our opinion, there has not been enough emphasis on the patient and caregiver journey.
Glioblastoma is a disease that tends to affect the entire family. Between 80% and 90% of individuals with the diagnosis have difficulty returning to work and daily routines because of the neurological and cognitive effects of the disease and need to rely heavily on the help of their families and close friends.
When patients are enrolled in trials, it’s very important not only to assess the effectiveness of the treatment on the tumor, but also to take a holistic view of the impact of the disease and treatment on the person and family. Survival is not just about quantity of time; it’s also about quality of life.
There is increasing movement towards incorporating a patient-outcomes focus in our studies. That means we examine how the patient is feeling and functioning, their symptoms and side effects and how to best manage them, and the issues that the patient’s family members are dealing with.
Dr. Gilbert: We are aiming for more of a partnership with patients, family members, and health care providers in our studies so that we are better able to ensure the best possible quality of life for patients dealing with the disease.
What does the future hold for glioblastoma research?
Dr. Gilbert: Despite ongoing worldwide efforts to develop new therapies for this type of brain cancer, none has so far improved survival appreciably. This is definitely an area of unmet need—we have to do much more for patients with glioblastoma.
We are testing many options and combinations of options in our search for the most effective and least toxic treatments, some of which have shown promise. But it is critical that we help more patients with glioblastoma participate in trials so that we can find solutions faster.
Although the improvements in outcomes have been small and slow, we are optimistic that with continued research efforts, we will discover better, less-toxic treatments and make progress against this disease.